Third Trimester Symptoms: 3rd Trimester Pregnancy And Prenatal Care
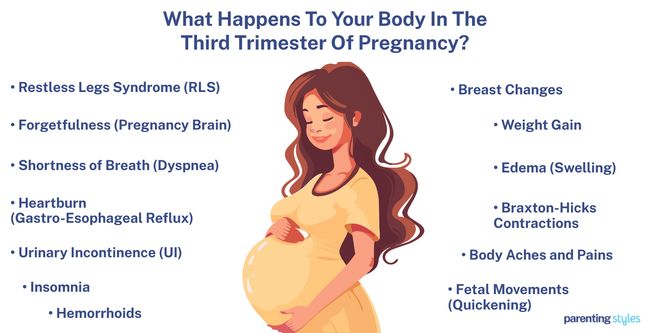
Third-trimester symptoms include restless leg syndrome, pregnancy brain, dyspnea, heartburn, and urinary incontinence. Other 3rd-trimester pregnancy symptoms include difficulties sleeping, hemorrhoids, breast changes, weight gain, edema, and Braxton-Hicks contractions. Emotional symptoms include mood swings, anxiety, and fear of childbirth. The third trimester, spanning weeks 29 to delivery, involves significant physical and emotional changes for mother and baby. The baby undergoes rapid growth, with organ maturation, brain development, and fat accumulation, to prepare for life outside the womb.

Prenatal care is crucial during this period, with regular checkups to monitor maternal and fetal health and address complications like preeclampsia or gestational diabetes. Maintaining a healthy diet, engaging in safe physical activity, and preparing emotionally for labor are vital. Standard prenatal tests include ultrasound, GBS screening, and maternal health checkups. Parents are encouraged to attend childbirth classes, practice relaxation techniques, and prepare a birth plan to ease anxiety and ensure informed decision-making during labor.
Complications that often arise in the third trimester include preterm labor, gestational diabetes, hypertensive disorders, vaginal infections, and placental issues. Preterm labor often occurs due to factors like infections, complications, or fetal anomalies, affecting approximately 10.23% of pregnancies.
When Does the 3rd Trimester Start?
The 3rd trimester starts in week 29 and lasts until the baby’s delivery, often between weeks 37 and 40.
What Are The Pregnancy Symptoms During 3rd Trimester?
Third-trimester symptoms include restless leg syndrome, pregnancy brain, dyspnea, heartburn, and urinary incontinence. Below are the key 3rd-trimester symptoms.
- Restless Legs Syndrome (RLS): Restless legs syndrome (RLS) is the overwhelming urge to move the legs, typically accompanied by unpleasant sensations in the lower limbs. A deficiency in brain iron and dopamine are associated with RLS. Dopamine is necessary for smoother, coordinated muscle movements, and iron is necessary for dopamine production, according to a 2009 study from The United States titled “Leg Cramps and Restless Legs Syndrome During Pregnancy,” conducted by Jennifer G. Hensley at the University of Colorado Denver and published in The Journal of Midwifery & Women’s Health.
- Forgetfulness (Pregnancy Brain): Forgetfulness is one of the most reported symptoms of cognitive decline during pregnancy, affecting about 80.8% of third-trimester pregnancies. The mother transfers glucose to the baby for development, leaving little energy for the maternal brain functioning, causing cognitive decline. Other factors like sleep disruption, fatigue, and anxiety contribute to poor memory functioning. Forgetfulness and other cognitive declines during pregnancy negatively impact daily life, leading to missed appointments and difficulty returning to work.
- Shortness of Breath (Dyspnea): Dyspnea pertains to difficulty breathing, often due to pregnancy-related physiologic changes. The baby’s size during the third trimester limits diaphragm movement, causing difficulty in breathing. Dyspnea affects about 53% of third-trimester pregnant women in the 2017 study “Symptom experience in late pregnancy,” by Kathleen R. Beebe et al. at San Francisco Bay Area and published in the Journal of Obstetric, Gynecologic & Neonatal Nursing.
- Heartburn (Gastro-Esophageal Reflux): Heartburn involves the backflow of stomach acid to the esophagus (acid reflux), causing a burning sensation in the chest and upper abdomen. Hormonal changes during pregnancy relax the lower sphincter in the esophagus, causing the stomach contents to reflux. The growing uterus contributes to heartburn by compressing the stomach and triggering acid flow. Heartburn affects about 81.8% of pregnant women in the third trimester, according to a 2014 study, “Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women,” conducted by Evsen Nazik et al.
- Urinary Incontinence: Urinary incontinence (UI) is the involuntary urine leakage. Hormonal changes during pregnancy weaken the pelvic floor muscles, leading to urinary leakage. Stress UI (leakage during coughing or sneezing) is the most common type of UI during pregnancy. SUI is the worst during the third trimester, affecting 54.2% of pregnant women in the 2019 study “Stress urinary incontinence in relation to pelvic floor muscle strength and associated factors in the third trimester of pregnancy: A cross-sectional study,” conducted by Astrid Yunita et al. in Indonesia and published in F1000 Research. UI is typically accompanied by frequent urination during late pregnancy.
- Insomnia (Trouble Sleeping): Insomnia is difficulty initiating or maintaining sleep. Causes of difficulty sleeping during pregnancy include discomfort, pain, shortness of breath, frequent urination, and anxiety. Insomnia typically worsens before labor as the production of oxytocin promotes wakefulness. 69.9% of pregnant women in the last trimester reported difficulty in maintaining sleep in the 2015 study, “Insomnia and sleep deficiency in pregnancy,” conducted by Cristina A Reichner and published in Obstetric Medicine. Early morning awakenings were described by 34.8%, and difficulty falling asleep was reported by 23.7%.
- Piles (Hemorrhoids): Hemorrhoids are swollen veins in the rectum and anus that cause discomfort, itching, and bleeding. The growing uterus puts pressure on the rectum and other vital veins, reducing blood flow in the muscles controlling the anal opening. High progesterone levels relax the veins, increasing the risk of swelling. Risk factors of hemorrhoids include constipation, diarrhea, and childbirth. Hemorrhoids are most common during the third trimester, affecting 61% of pregnant women, according to a 2022 study titled “Perianal Diseases in Pregnancy and After Childbirth: Frequency, Risk Factors, Impact on Women’s Quality of Life and Treatment Methods.”
- Breast Changes: Breast changes during the third trimester include tenderness, enlargement, and nipple discoloration. Increased estrogen and progesterone levels change the anatomy of the breasts to prepare for breastfeeding. Women in the fifth or sixth month of pregnancy experience leaky breasts, indicating colostrum (the first form of milk) production.
- Weight Gain: Weight gain during pregnancy is necessary to support the baby’s development. Pregnant women with an average weight (18.5–24.9 kg/m2) are recommended to gain 0.8-1 pounds per week during the third trimester. Weight gain shifts the center of gravity, causing pain in the feet and lower back. Pregnant women gaining weight beyond the recommended ranges have higher risks of high blood pressure, gestational diabetes, and labor complications.
- Edema (Swollen Ankles and Feet): Edema during pregnancy typically involves swelling in the thigh, legs, and ankle. Increased body weight and a larger uterus put pressure on the veins, causing swelling in the lower extremities. Other causes of edema include limited physical inactivity and hormonal imbalances. The risk of blood clotting in the veins increases during the third trimester, making swelling more frequent. Severe swelling in the face and hands accompanied by persistent headaches typically signals preeclampsia, a hypertensive disorder occurring after 20 weeks of pregnancy. Make sure to monitor sudden and extreme swelling to receive prompt medical attention.
- Braxton-Hicks Contractions: Braxton-Hicks contractions (prodromal or false labor pains) are painless uterine contractions that occur to prepare the body for labor. The contractions are unpredictable and last less than 30 seconds to 2 minutes. False contractions are only felt in a specific area of the abdomen and do not lead to cervical dilation (opening). Braxton-Hicks contractions are different from true labor pains, which are regular, painful contractions that signal the onset of labor.
- Body Aches and Pains: Body aches and pains during the third trimester typically affect the lower back, back, hand-wrist, and hips. The enlarging uterus shifts the body’s center of mass, causing joint and muscle strains. Hormonal fluctuations and swelling soften ligaments and tissues, adding more pain. Body aches increase during the third trimester as the mother gains weight and changes posture, according to a 2018 study titled “Musculoskeletal pain and symptoms in pregnancy: a descriptive study.”
- Fetal Movements (Quickening): Quickening is the first noticeable movement of the fetus against the maternal abdominal wall. Mothers begin to feel the baby kick and stretch from weeks 14-22, persisting until the fetus exhibits arm-cross movements and responses to the mother’s voice in the third trimester. Motor movements eventually decrease towards the end of pregnancy as brain parts mature and develop.
What Is The Third Trimester Of Pregnancy?
The third trimester of pregnancy starts at week 29 and lasts until the baby’s delivery. 3rd trimester, one of the three pregnancy trimesters, is marked by various changes in the mother’s body to prepare for labor and birth.
The baby experiences enormous growth and development in preparation for life outside the womb. The organs mature, and the translucent skin thickens, gaining a protective layer of fat underneath. A full-term baby (born in weeks 39 and 40) weighs around 3403 grams to 3617 grams (7.50 pounds to 7.97 pounds).
Women in the 3rd trimester of pregnancy experience more intense physical and emotional challenges. Pregnant mothers experience uncomfortable Braxton-Hicks contractions to prepare the body for labor. Backaches become more common as the growing baby adds strain to the body, and hemorrhoids develop from the pressure of the expanding uterus on the veins. The upcoming labor and childbirth bring worries and anxiety to the mother.
Prenatal visits during the 3rd trimester of pregnancy are crucial for monitoring the mother and the baby’s health as the due date approaches. The appointments allow the healthcare providers to discuss birth plans, address symptoms, and monitor fetal growth.
What Is The Importance Of Understanding Third Trimester In Pregnancy?
The importance of understanding the third trimester of pregnancy is recognizing that you are entering the last trimester. This is a vital time for the mother and the baby, as significant physical and emotional changes occur. Attending regular prenatal checkups is vital as the baby experiences rapid growth and development, including maturing lungs and accumulating fat for temperature regulation after birth. Monitoring fetal growth and maternal health helps detect and manage potential complications like preterm labor, gestational diabetes, or high blood pressure.
The mother experiences symptoms such as shortness of breath, heartburn, swelling, and back pain due to the expanding uterus and increased pressure on internal organs. Understanding these changes helps manage discomfort and prepare for a safe delivery. Pelvic floor exercises strengthen muscles to prevent urinary incontinence. Proper hydration and diet reduce swelling and manage heartburn.
Common emotional symptoms include mood swings, anxiety, and insomnia. Hormonal shifts, physical discomfort, and concerns about labor and parenting contribute to these feelings. Attending childbirth classes and practicing relaxation techniques such as deep breathing or meditation alleviate stress and prepare for labor.
Trimester 3 is a critical stage for staying informed about health, maintaining prenatal care, and preparing physically and emotionally for birth.
When Does The Third Trimester Start?
The third trimester of pregnancy starts at week 29 and lasts until delivery, marking the final phase before the baby’s birth. The third trimester weeks cover months 7, 8, 9, and 10.
How many weeks is the third trimester? The third trimester includes 12 weeks (3 months) for a full-term baby delivered at week 40.
What To Expect In The Third Trimester Of Pregnancy?
The third-trimester pregnant mother should expect several changes in her body, physical and emotional, as the baby grows rapidly and the body prepares for labor.
Restless legs syndrome (RLS) arises due to low dopamine levels, leading to an uncontrollable urge to move the legs, especially in the evening. Forgetfulness, often termed “pregnancy brain,” occurs as glucose is prioritized for the baby, causing cognitive decline and memory issues. Shortness of breath (dyspnea) develops as the baby pushes against the diaphragm, making breathing harder. Hormonal changes and increased pressure on the stomach trigger heartburn, while urinary incontinence results from weakened pelvic floor muscles, causing urine leakage during coughing or sneezing.
Insomnia develops from discomfort, frequent urination, and anxiety about the upcoming labor. Hemorrhoids, or swollen veins in the rectum, cause discomfort due to increased uterine pressure. Tender breasts begin to produce colostrum in preparation for breastfeeding. Weight gain shifts the body’s center of gravity, leading to foot and lower back pain, while leg swelling (edema) results from extra pressure on the veins.
Braxton-Hicks contractions, or false labor pains, become more frequent and noticeable as the body prepares for labor. Body aches, especially in the lower back and hips, intensify due to ligament loosening and posture changes. The baby’s movements, such as kicking and stretching, feel stronger but decrease as the baby prepares for birth.
Mood swings, anxiety, and fear about labor arise from hormonal shifts and the physical toll of pregnancy. These changes make it difficult to manage everyday stress and emotions.
What Happens To Your Body In The Third Trimester Of Pregnancy?
Changes that happen to your body in the third trimester include restless legs syndrome, forgetfulness, dyspnea, heartburn, and urinary incontinence. Here are some key changes in the mother’s body during the third trimester of pregnancy.
- Restless Legs Syndrome (RLS): Low dopamine levels increase the urge to move the legs. Symptoms typically worsen in the evening and resolve after childbirth.
- Forgetfulness (Pregnancy Brain): Cognitive decline due to glucose transfer to the baby, sleep disruption, and fatigue, affecting memory and daily functioning.
- Shortness of Breath (Dyspnea): The growing baby restricts diaphragm movement, making breathing difficult.
- Heartburn (Gastro-Esophageal Reflux): Relaxation of the esophageal sphincter and uterine pressure cause acid reflux and a burning sensation.
- Urinary Incontinence (UI): Weakened pelvic floor muscles lead to involuntary urine leakage, especially when coughing or sneezing.
- Insomnia: Sleep difficulties arise from discomfort, frequent urination, and anxiety, which often worsen due to hormonal changes before labor.
- Hemorrhoids: Swollen veins in the rectum develop from uterine pressure and hormonal changes, causing discomfort, itching, and bleeding.
- Breast Changes: Tenderness, enlargement, and colostrum production prepare the body for breastfeeding.
- Weight Gain: Maternal weight gain supports fetal development but shifts the center of gravity, leading to foot and lower back pain.
- Edema (Swelling): Swelling occurs in the legs, ankles, and feet due to increased weight and vein pressure, with a risk of blood clotting.
- Braxton-Hicks Contractions: Painless, irregular uterine contractions prepare the body for labor without causing cervical dilation.
- Body Aches and Pains: Pain in the lower back, hips, and joints results from posture changes, weight gain, and loosening ligaments.
- Fetal Movements (Quickening): Kicking and stretching from the baby become noticeable but decrease closer to labor as brain maturation progresses.
What Are The Emotional Changes During The Third Trimester Of Pregnancy?
The emotional changes during the third trimester of pregnancy include mood swings, fear, stress and anxiety, weepiness, and anger.
The mood changes frequently and unpredictably during the third trimester of pregnancy. The increase in hormones such as estrogen and progesterone tends to make women more sensitive to minor issues. The rise of stress hormones and discomfort from physical changes contribute to the sudden and often unexpected shifts in moods, according to a 2017 study from India titled “Emotive whims distressing pregnant women,” conducted by V. Kiruthiga at SRM University and published in International Research Journal of Engineering and Technology.
Fear tends to increase throughout pregnancy and peak in the 3rd trimester as the woman is afraid of the labor pain and worries about their baby’s health, wondering if the child is free of disabilities and health issues. Fear heightens a mother’s stress and anxiety. Crying and becoming angry for minor issues are often seen in the final trimester as women have a hard time controlling their emotions due to changes in hormones, physical heaviness, lifestyle, and routines.
How Big Can A Mother’s Belly Grow During The 3rd Trimester?
A mother’s belly can grow from approximately 27 to 42 centimeters in fundal height during the third trimester. Belly growth is often tracked by measuring the fundal height or the distance from the pubic symphysis (the front of the pelvis) to the top of the uterus in the past. Uterine size and growth rate are influenced by factors like the mother’s body mass index (BMI), the number of previous pregnancies, variations in amniotic fluid levels, and the size of the fetus.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth in the past. Fundal height typically correlates with gestational age from 20 weeks onwards, with the uterus significantly expanding to accommodate the growing fetus. However, the 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence for using the SFH to predict fetal health.
Are Cramps Worse In The Third Trimester Of Pregnancy?
Yes, cramps do get worse in the third trimester. Braxton-Hicks contractions or false labor pains become stronger as the term approaches, according to a 2020 study titled “Uterine contractions clustering based on electrohysterography,” conducted by Filipa Esghaldo et al. in Portugal and published in Computers in Biology and Medicine journal. Braxton-Hicks contractions intermittently bring menstrual-like cramps in front of the abdomen to prepare the body for labor.
Contractions that do not resemble menstrual cramps are likely true labor contractions. True labor pains affect the abdomen and the back in increasing frequency and intensity. The cramps of true labor contractions worsen and strengthen with maternal movement or position change, signaling the onset of labor.
How Often Do You Feel Contractions In The Third Trimester?
The frequency of contractions in the third trimester is different for every woman. Some reported having Braxton-Hicks contractions or false labor pains every 3-4 hours starting the 20th week, while others reported contractions once every hour. The consensus, however, is that Braxton-Hicks contractions occur more frequently as the due date approaches to prepare the body for labor.
Braxton-Hicks are mild, sporadic contractions in the front of the abdomen. False labor pains last shorter than true labor contractions, ranging between 24 seconds to five minutes, according to a 2020 study titled “Uterine contractions clustering based on electrohysterography.” Contractions that occur longer, stronger, and more regularly indicate true labor contractions. True labor pains are felt around the abdomen and the back and intensify when the mother changes positions. The cervix dilates (widens) during true labor contractions, signaling the first stage of labor.
How Would You Differentiate Normal Contractions To Going Into Labor Contractions?
Normal contractions, or Braxton-Hicks contractions, are painless and sporadic. Braxton-Hicks occur shortly, lasting less than 30 seconds to 5 minutes, and disappear with a change in position or activity level. The pain is felt as belly tightening and does not intensify over time. Regular contractions do not cause cervical dilation (opening) and do not signal labor onset, according to a 2023 study titled “Braxton Hicks Contractions,” by Deborah A. Raines et al., published in StatPearls.
Labor contractions are stronger and longer. The contractions regularly occur at about 3 to 5 minutes apart, accompanied by pain wrapping around the belly and lower back. Labor contractions resemble a crescendo pattern, where the cramps intensify over time. Contractions that signal active labor are typically accompanied by bloody mucus discharge, cervical dilation (opening), and water breaking. Cervical dilation from 0 to 6 centimeters signifies the latent phase, the early part of the first stage of labor. Dilation beyond 6 centimeters indicates the active phase, the final part of the first stage, according to a 2023 study titled “Vaginal delivery” by Ninad M. Desai et al., published in StatsPearl.
How Would You Differentiate Normal Contractions From Preterm Labor Contractions?
Regular uterine contractions with cervical dilation before 37 weeks of pregnancy indicate preterm labor. Causes of preterm labor include infections, multiple pregnancies, cervical abnormalities, and complications such as diabetes and high blood pressure. The majority of preterm deliveries are late preterm births, occurring between 34 and 36 weeks of pregnancy. Premature babies typically face learning disabilities and visual and hearing problems, according to a 2023 World Health Organization report.
How Does The Baby Develop In Different Weeks Of The Third Trimester?
The baby develops rapidly during the third trimester of pregnancy. Understanding what happens during pregnancy weeks helps expectant mothers be more prepared and connected to these changes. Here is how the baby develops during the third trimester of pregnancy week by week.
1. 29 Weeks Pregnant
Babies beyond 20 weeks are better measured in biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and humerus length (HL) rather than crown-rump length (CRL).
29-week-old babies are about the size of a butternut squash, weighing approximately 1,350 grams (2.98 pounds). The 50th percentile measurements for fetal growth at 29 weeks pregnant are as follows: the BPD is 74 millimeters, the HC is 273 millimeters, the AC is 250 millimeters, the FL is 54 millimeters, and the HL is 49 millimeters, according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
The baby develops rapidly, reaching several key milestones in preparation for life outside the womb. The fetus undergoes significant lung development as alveoli (tiny air sacs) form, preparing for post-birth breathing. Red blood cell production fully shifts to the bone marrow, ensuring adequate oxygen supply as growth continues. Neurons form nerve pathways in the brain, supporting movement and sensory functions. Fat deposits accumulate under the skin, supporting energy storage and temperature regulation after birth. Calcium strengthens the skeleton as secondary ossification centers appear, indicating strong bone development.
29 weeks pregnant symptoms include insomnia, piles, constipation, lower back pain, and forgetfulness. 29 weeks pregnancy symptoms such as restless legs syndrome (RLS) and leg cramps often affect pregnant women at night, contributing to sleep disturbances.
2. 30 Weeks Pregnant
A 30-week-old baby has reached the size of a large cabbage, weighing approximately 1,523 grams (53.72 ounces or 3.36 pounds). The 50th percentile measurements for fetal growth at 30 weeks pregnant are as follows: the biparietal diameter (BPD) is 77 millimeters, the head circumference (HC) is 281 millimeters, the abdominal circumference (AC) is 260 millimeters, the femur length (FL) is 56 millimeters, and the humerus length (HL) is 51 millimeters, according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
Your baby’s movements become stronger and more varied, responding to sounds, touch, and other stimuli, with some movements visible through the skin. Eye movements improve in coordination, and the eyelids are fully open, supporting vision control. Lanugo, the fine hair covering the body, begins to shed, and thicker hair forms on the scalp. Fat accumulates for energy storage and temperature regulation, while the skin becomes smoother due to increased collagen production. Lung development progresses into the saccular stage, preparing the baby for breathing. Most babies assume a head-down position in preparation for birth. Your baby’s brain development accelerates, with growing connections that control movement and sensory functions like vision.
30 week pregnancy symptoms include lower back pain, shortness of breath, prodromal labor, fatigue, and skin changes. Mood swings and snoring are other 30 week pregnancy symptoms.
3. 31 Weeks Pregnant
Your 31-week-old baby is about the size of a coconut, weighing around 1707 grams (60.21 ounces or 3.76 pounds). The 50th percentile measurements for fetal growth at 31 weeks pregnant are as follows: the biparietal diameter (BPD) is 79 millimeters, the head circumference (HC) is 289 millimeters, the abdominal circumference (AC) is 269 millimeters, the femur length (FL) is 59 millimeters, and the humerus length (HL) is 53 millimeters, according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
Stronger kicks and visible movements appear under the mother’s skin as fetal activity increases. Brain development accelerates, forming ridges (gyri) and strengthening nerve pathways to improve nervous system communication. Sensory milestones advance as eyes respond to light and ears distinguish between familiar and unfamiliar sounds. Genital development is well-defined, with testes descending in male fetuses and distinct labia forming in female fetuses. Your baby’s fingernails near full growth at 31 weeks of pregnancy.
31 weeks pregnancy symptoms include dyspnea (shortness of breath), mood swings, morning sickness, nail changes, and prodromal labor (false labor). 31 weeks pregnancy symptoms sometimes include leaking breasts, urinary incontinence, insomnia, lower back pain, and weight gain.
4. 32 Weeks Pregnant
Babies at 32 weeks are about the size of a jicama, weighing approximately 1901 grams (67.06 ounces or 4.19 pounds). The 50th percentile measurements for fetal growth at 32 weeks pregnant are as follows: the biparietal diameter (BPD) is 81 millimeters, the head circumference (HC) is 296 millimeters, the abdominal circumference (AC) is 279 millimeters, the femur length (FL) is 61 millimeters, and the humerus length (HL) is 54 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
Fetal movements become more frequent and noticeable as responses to external stimuli increase. Fat accumulates under the skin to regulate temperature and support brain and nervous system growth. The skin thickens, becoming less permeable, while lanugo, the fine hair on the body, begins to shed. Thicker hair grows on the scalp, and fingernails and toenails fully develop. Genitalia matures, with testes descending in males and labia maturing in females. Bones harden as calcium transfers from the mother, preparing the skeleton for life outside the womb. Babies typically start blinking, and the digestive system functions with meconium accumulating in the intestines. The baby often shifts into a head-down position in preparation for birth.
Week 32 pregnancy symptoms include constipation, leg cramps, dizziness, piles, and leaky breasts. Other 32 weeks pregnancy symptoms include itchy skin, insomnia, and stretch marks.
5. 33 Weeks Pregnant
Your 33-week-old baby is about the size of a pineapple, weighing around 2103 grams (74.18 ounces or 4.64 pounds). The 50th percentile measurements for fetal growth at 33 weeks pregnant are as follows: the biparietal diameter (BPD) is 83 millimeters, the head circumference (HC) is 303 millimeters, the abdominal circumference (AC) is 288 millimeters, the femur length (FL) is 63 millimeters, and the humerus length (HL) is 56 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
Babies at 33 weeks undergo significant physical growth and system maturation. Sensory abilities improve as pupils react to light and eye movements. Brain development accelerates, supporting early memory formation and sound recognition. Bones harden as calcium and minerals transfer from the mother, while the immune system matures through the transfer of maternal antibodies. Facial expressions like smiling and grimacing become more refined, and responses to external stimuli show more complex movements. Developmental milestones at 33 weeks prepare the baby for life outside the womb, aiding temperature regulation and immune function.
33 weeks pregnancy symptoms include pelvic girdle pain, Braxton Hicks contractions, insomnia, wrist pain, and vaginal swelling. 33 weeks pregnancy symptoms involve discomfort in the pelvis due to joint loosening and Braxton Hicks contractions
6. 34 Weeks Pregnant
Your 34-week-old baby is around the size of a cantaloupe, weighing about 2312 grams (81.55 ounces or 5.10 pounds). The 50th percentile measurements for fetal growth at 34 weeks pregnant are as follows: the biparietal diameter (BPD) is 85 millimeters, the head circumference (HC) is 309 millimeters, the abdominal circumference (AC) is 298 millimeters, the femur length (FL) is 65 millimeters, and the humerus length (HL) is 58 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
The rooting reflex, which aids in latching onto the breast, emerges at 34 weeks. Vision improves as the retina and brain coordinate during REM sleep, promoting healthy visual development. Rapid brain growth forms about 40,000 synapses per second, enhancing cognitive and sensory functions. Facial expressions like crying and smiling become more distinct, and hand-to-face movements increase. Bones harden as growth plates develop, and fat accumulation under the skin aids temperature regulation after birth. The immune system strengthens as maternal antibodies transfer, preparing the baby for life after delivery.
Week 34 pregnancy symptoms include fatigue, lumbar pain, constipation, increased vaginal discharge, and prodromal labor. Other 34 weeks pregnancy symptoms include cramping, breast changes, and overactive bladder.
7. 35 Weeks Pregnant
Babies at 35 weeks are about the size of a honeydew melon, weighing approximately 2527 grams (89.14 ounces or 5.57 pounds). The 50th percentile measurements for fetal growth at 35 weeks pregnant are as follows: the biparietal diameter (BPD) is 87 millimeters, the head circumference (HC) is 315 millimeters, the abdominal circumference (AC) is 307 millimeters, the femur length (FL) is 67 millimeters, and the humerus length (HL) is 59 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
The baby reaches several developmental milestones at 35 weeks, including fully developed hearing, allowing for recognition and response to familiar sounds, especially the mother’s voice. Intricate facial expressions like smiling, frowning, and cry-like gestures emerge. About 80% of the skeleton is complete, with calcium and phosphorus from the mother strengthening the bones. Testes in male fetuses fully descend into the scrotum, marking a key step in reproductive development. The cerebral cortex expands to support memory and cognitive functions, while myelination improves brain-body communication. The lungs and kidneys are near full functionality, and fat deposits under the skin help regulate temperature after birth.
35 weeks pregnancy symptoms include breast changes, bad dreams, prodromal labor, lightning crotch, and rip pain. Other 35 weeks pregnancy symptoms include frequent urination, constipation, and body pain.
8. 36 Weeks Pregnant
Your 36-week-old baby is about the size of a romaine lettuce, weighing around 2745 grams (96.83 ounces or 6.05 pounds). The 50th percentile measurements for fetal growth at 36 weeks pregnant are as follows: the biparietal diameter (BPD) is 89 millimeters, the head circumference (HC) is 321 millimeters, the abdominal circumference (AC) is 317 millimeters, the femur length (FL) is 69 millimeters, and the humerus length (HL) is 61 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
The baby at 36 weeks reaches various milestones in preparation for life outside the womb. Sleep patterns mature, with organized REM (rapid eye movement) and non-REM cycles supporting brain development. The baby likely shifts into a head-down position, preparing for birth. Rapid brain growth continues, with improved myelination enhancing communication between the brain and spinal cord. Bone growth slows as hardening continues, while calcium levels remain high from previous weeks. The lungs are near full maturity as alveoli form in preparation for breathing. Lanugo begins to shed, and the baby practices swallowing amniotic fluid, sucking, and responding to external stimuli, such as the mother’s voice.
36 weeks pregnancy symptoms include overactive bladder, forgetfulness, Braxton-Hicks contractions, insomnia, and lightning crotch. Other 36 weeks pregnancy symptoms include swollen feet, vaginal discharge, and leaky breasts.
9. 37 Weeks Pregnant
Your 37-week-old baby is about the size of Swiss chard, weighing around 2966 grams (104.62 ounces or 6.54 pounds). The 50th percentile measurements for fetal growth at 37 weeks pregnant are as follows: the biparietal diameter (BPD) is 90 millimeters, the head circumference (HC) is 326 millimeters, the abdominal circumference (AC) is 328 millimeters, the femur length (FL) is 70 millimeters, and the humerus length (HL) is 62 millimeters, according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
Developmental changes at 37 weeks pregnant ensure the baby is well-prepared for life outside the womb. Most babies shift into a head-down position in preparation for birth. Coordinated movements like sucking, swallowing, and practicing breathing continue to strengthen, though movement often seems reduced due to limited space. The skin is fully developed, with all five layers present and covered by vernix caseosa for protection. Major organs, such as the kidneys and lungs, approach full development, preparing for independent function. Rapid brain growth continues, with increased myelination enhancing nerve signal transmission.
37 weeks pregnancy symptoms include pregnancy brain, prodromal labor, abdominal and pelvic pressure, body aches and pains, and water breaking. Other 37 weeks pregnancy symptoms include frequent micturition, constipation, and indigestion.
10. 38 Weeks Pregnant
Babies at 38 weeks are about the size of a leek, weighing around 3186 grams (112.38 ounces or 7.02 pounds). The 50th percentile measurements for fetal growth at 38 weeks pregnant are as follows: the biparietal diameter (BPD) is 92 millimeters, the head circumference (HC) is 332 millimeters, the abdominal circumference (AC) is 338 millimeters, the femur length (FL) is 72 millimeters, and the humerus length (HL) is 63 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
Lung maturation progresses as the baby prepares for breathing. The brain supports memory and learning, allowing the baby to recognize familiar voices and sounds, such as the mother’s voice, and respond with a slower heart rate. Most fine lanugo hair is shed, while vernix caseosa remains on the skin to regulate temperature and protect against amniotic fluid. Fat builds under the skin, aiding temperature regulation after birth. The immune system nears full development, ready to fight infections. Major organs, including muscles, kidneys, and the digestive system, are nearly complete, signaling readiness for life outside the womb.
Symptoms at week 28 include pregnancy brain, gastrointestinal issues, leaky breasts, flu-like symptoms, and bloody show. Other 38 weeks pregnancy symptoms include lower back pain, overactive bladder, and pelvic pain.
11. 39 Weeks Pregnant
Babies at 39 weeks are about the size of a mini watermelon, weighing approximately 3403 grams (120.04 ounces or 7.50 pounds). The 50th percentile measurements for fetal growth at 39 weeks pregnant are as follows: the biparietal diameter (BPD) is 94 millimeters, the head circumference (HC) is 337 millimeters, the abdominal circumference (AC) is 350 millimeters, the femur length (FL) is 73 millimeters, and the humerus length (HL) is 64 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
Brain development continues rapidly, with myelination improving communication between regions, supporting sight, movement, and hearing. The lungs now breathe air and keep maturing after birth. The digestive system is ready to absorb nutrients. The baby’s thick skin has shed most lanugo, while vernix caseosa remains for protection. The skeletal system is strong, with fully developed femur and humerus bones. Your baby’s developed muscles, organs, and ability to recognize sounds and respond to light indicate preparedness for life outside the womb.
39 weeks pregnancy symptoms include pregnancy brain, GERD, frequent contractions, backache, and lightning crotch. Other 39 weeks pregnancy symptoms include insomnia, anxiety, and rib pain.
12. 40 Weeks Pregnant
Your 40-week-old baby is about the size of a pumpkin, weighing around 3617 grams (127.59 ounces or 7.97 pounds). The 50th percentile measurements for fetal growth at 40 weeks pregnant are as follows: the biparietal diameter (BPD) is 96 millimeters, the head circumference (HC) is 342 millimeters, the abdominal circumference (AC) is 363 millimeters, the femur length (FL) is 73 millimeters, and the humerus length (HL) is 64 millimeters, according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine. The baby is now fully developed and ready for birth.
“Lightening,” or the baby dropping into the lower pelvis, eases pressure on the diaphragm while increasing pressure on the bladder. The lungs are mature, with sufficient alveoli for breathing outside the womb. The digestive system, liver, and kidneys are fully functional and ready to process nutrients and waste. The skin is developed, though dry patches appear as vernix caseosa sheds. Muscles are fully developed and comprise 20.5% of the baby’s body weight. Reflexes like sucking and swallowing are well-practiced, necessary for feeding. Strong bones, developed organs, and enhanced sensory functions show the baby is fully prepared for life outside the womb.
40 weeks pregnancy symptoms not to ignore include forgetfulness, crowning, contractions, diarrhea, and pelvic pain. Other 40 weeks pregnancy symptoms include leg cramps, insomnia, and nesting.
Do Babies Still Develop Their Brain In The 3rd Trimester?
Yes, babies do still develop their brains in the third trimester. The neuronal pathway for voluntary motor function becomes more developed by week 29, allowing for control of voluntary movements in the lower limbs.
Babies hear by week 29 as the auditory system becomes well-developed. Sleeping states are more organized at weeks 28-30 as the brainstem (responsible for vital functions) and thalamus (brain’s information relay station) start functioning.
The cortex develops significantly by week 32, setting the stage for future cognitive and motor functions. The right and left hemispheres synchronize between weeks 34-35, allowing for more coordinated movements.
Your baby’s brain development continues beyond the trimester. Critical biological processes like breathing and temperature regulation mature substantially after delivery. The autonomic nervous system develops, enabling more organized sleeping patterns outside the womb, according to a 2019 study from Italy titled “Correlation between human nervous system development and acquisition of fetal skills: An overview,” conducted by Elisa Borsani et al. at the University of Brescia and published in Brain and Development.
What Are The Tips For Prenatal Care In The Third Trimester?
Tips for prenatal care (antenatal care) in the third trimester include attending prenatal appointments and childbirth classes, taking prenatal vitamins, maintaining a healthy lifestyle, and engaging in physical activity. Here are 7 tips for a healthy pregnancy in the third trimester.
- Attend Antenatal Care Appointments: Regular prenatal visits help monitor fetal and maternal health by tracking essential indicators like blood pressure, weight, your baby’s growth, and abdominal measurements. Visits with your OBGYN typically involve monitoring fetal heartbeat, movements, and position. Prenatal tests like group B strep, a complete blood count, urinalysis, alpha-fetoprotein (AFP), nonstress test, and glucose screening detect fetal and maternal complications during the third trimester. Pregnant mothers often require more frequent checkups in the last trimester, with appointments typically scheduled every two weeks until week 36, followed by weekly visits from week 37 until delivery. Discuss birth plans and care strategies with your OB-GYN to prepare for childbirth.
- Attend Childbirth Classes: Childbirth classes provide essential information about the stages of labor, helping reduce anxiety about the approaching due date. Childbirth classes emphasize the importance of a support system, encouraging participation from your partner or labor coach to assist during labor and postpartum recovery. Parents explore different birthing options, such as natural delivery and epidurals, along with pain management techniques, aiding in confident, informed decisions when creating a birth plan. Care strategies for labor and delivery are discussed, helping you feel more prepared and confident for childbirth.
- Continue Taking Prenatal Vitamins: Prenatal vitamins provide essential nutrients to support your health and the development of your fetus. Folic acid, iron, calcium, vitamin D, choline, protein, and other nutrients maintain energy and promote fetal growth, preparing your baby for life outside the womb. Always check serving sizes on the label to avoid exceeding the recommended dosage, as excessive vitamin A often leads to birth defects.
- Maintain a Healthy Diet and Lifestyle: Eat a varied diet, including plenty of fruits, vegetables, low-fat protein, and fiber, to support your health and the baby’s growth. Consume healthy foods and monitor your calorie intake to meet the increased nutritional needs during pregnancy. Avoid alcohol use and smoking, which increase the risks of complications like early delivery and fetal alcohol syndrome. Stay hydrated by drinking lots of water, and incorporate fiber-rich foods into your meals to maintain digestive health.
- Engage in Physical Activity: Physical activity positively impacts physical and psychological well-being, especially during the third trimester. Exercises like walking, swimming, and Kegel exercises help improve circulation, strengthen the pelvic floor, and alleviate discomfort like back pain. Staying active, unless experiencing swelling or pain, boosts energy levels, improves mood, and promotes better sleep. Start an exercise routine with gradually increasing intensity to ensure safety and avoid strain.
- Find a Comfortable Sleep Position: Sleep issues often arise in the final months of pregnancy due to fatigue and discomfort from leg cramps, urinary incontinence, shortness of breath, and back pain, according to a 2016 study titled “The relationship between sleep disturbance in late pregnancy and labor outcomes,” by Abdul-monim Batiha et al. and published in International Journal of Health. Using pillows helps you find a comfortable position, with side sleeping being especially beneficial for comfort and safety as your uterus expands.
- Prepare for Labor and Delivery: Active participation in antenatal education classes as part of prenatal care offers realistic insights into parenting, labor, and pain management options. Expecting parents to pre-register at the hospital and prepare key items like a hospital bag with nursing pads, baby clothes, and necessary medicines. Keep important contacts, including your OBGYN or midwife, easily accessible. Monitor symptoms like contractions, fluid leaks, bleeding, and other signs of labor. Pelvic exams are performed to check for dilation and effacement as delivery nears.

What Types Of Foods Are Essential In The Third Trimester?
Types of foods beneficial to eat during the third trimester include foods rich in calcium, iron, iodine, choline, vitamins A, C, D, B6, B12, and folate to support your health and baby’s growth. Here are 14 beneficial foods to eat during the third trimester of pregnancy.
- Calcium-rich foods: Calcium supports the development of strong bones and teeth in your baby. Consume cheese, yogurt, and milk.
- Iron-rich foods: Iron facilitates red blood cell production, delivers oxygen to your baby, and supports muscle development. Get iron from prune juice, poultry, lean meats, dried beans, lentils, and peas.
- Iodine-rich foods: Iodine is essential for your baby’s brain development. Try eggs, iodized table salt, and seafood.
- Choline-rich foods: Choline supports brain and spinal cord development in your baby. Good sources include beef liver, soy products, milk, and eggs.
- Vitamin A-rich foods: Vitamin A helps form red blood cells and supports immune function. Try sweet potatoes, dark leafy greens, broccoli, and carrots.
- Vitamin C-rich foods: Vitamin C aids in iron absorption and supports skin health. Incorporate broccoli, berries, strawberries, and citrus fruits into your diet.
- Vitamin D-rich foods: Vitamin D is important for healthy bone development. Get Vitamin D from fortified milk, salmon, and sardines.
- Vitamin B6-rich foods: Vitamin B6 helps your body use protein, fat, and carbohydrates. Try pork, bananas, whole-grain cereals, and starchy foods like potatoes.
- Vitamin B12-rich foods: Vitamin B12 supports the formation of red blood cells and nervous system health. Consume fish, poultry, milk, and eggs.
- Folic acid-rich foods: Folic acid prevents birth defects and supports fetal growth and development. Sources include dark green leafy vegetables, fortified cereal, enriched bread, and pasta.
- Whole grains: Whole grains provide fiber, B vitamins, and folic acid, supporting fetal growth and digestion. Try brown rice, whole-wheat pasta, quinoa, and oatmeal.
- Fruits: Fruits offer antioxidants, vitamins, and fiber. Try fresh fruit, bananas, berries, dried fruit, and frozen fruit.
- Vegetables: Vegetables provide essential vitamins, minerals, and fiber. Choose from canned, raw, or frozen vegetables.
- Dairy products: Dairy products supply calcium, vitamin D, and protein. Get pasteurized milk, yogurt, hard cheese, and low-fat or fat-free dairy.
What Exercises Are Safe And Beneficial During The Third Trimester?
Safe and beneficial exercises during the third trimester include walking, swimming, stationary cycling, stretching, and Kegel exercise, according to the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Here are 5 beneficial exercises for the third trimester of pregnancy.
- Walking: Walking is a safe, low-impact exercise that helps with cardiovascular fitness, joint health, and overall well-being during the third trimester.
- Swimming: Water-based activities are particularly beneficial as they reduce joint strain and provide a full-body workout, improving endurance, muscle strength, and flexibility.
- Stationary cycling: Riding a stationary bike offers a way to keep up your cardiovascular activity without the risk of falling, which becomes more critical as your center of gravity shifts. It helps maintain cardiovascular fitness and joint health.
- Stretching: Gentle stretching improves flexibility and helps relieve discomfort, especially in the back and legs.
- Pelvic floor muscle training: Pelvic exercises like Kegel strengthen pelvic floor muscles, prevent urinary incontinence (involuntary urine leakage), and help relax and stretch the perineum in preparation for delivery.
Avoid exercises that carry a high risk of falling or involve intense contact. Stay hydrated, particularly when exercising in warm conditions, and avoid overexertion.

What Are The Things To Avoid In The 3rd Trimester Of Pregnancy?
Things to avoid in the third trimester include alcohol, smoking, recreational drugs, caffeine, certain medications and supplements, and high-mercury fish. Here are 15 things you must avoid during the second trimester of pregnancy.
- Alcohol: Completely avoid alcohol during pregnancy. Alcohol causes severe birth defects and developmental issues like fetal alcohol spectrum disorders (FASD). Even small amounts lead to cognitive and behavioral problems in the baby, according to a 2020 study from Oregon Health and Science University and Oregon State University, published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Smoking increases the risks of premature birth, low birth weight, and miscarriage. Exposure to secondhand smoke is harmful, according to a 2020 study published in the International Journal of Environmental Research and Public Health by Gillian S. Gould and others. Seek help to quit if necessary.
- Recreational Drugs: Recreational drugs pose dangers to the baby’s health, leading to complications like developmental delays.
- Cannabis: Like other drugs, cannabis leads to low birth weight and developmental issues for the baby.
- Caffeine: Limit caffeine intake to 200 mg per day (about one 12-ounce cup of coffee). Excessive amounts increase the risk of fetal complications like low birth weight.
- Certain Medications and Supplements: Always consult your healthcare provider before taking medications, supplements, or herbal remedies, as some are unsafe during pregnancy.
- High-Mercury Fish: Avoid fish high in mercury, such as swordfish, sharks, and king mackerel, as mercury harms the baby’s nervous system.
- Undercooked or Raw Meat: Ensure all meats are thoroughly cooked to avoid infections like toxoplasmosis, which harms your baby. Raw or undercooked foods must be completely avoided to minimize health risks.
- Deli Meats and Unpasteurized Foods: Avoid deli meats unless thoroughly heated to steaming, and avoid unpasteurized dairy products and soft cheeses to prevent exposure to harmful bacteria like listeria, a key concern during pregnancy.
- Excessive Physical Activity: Avoid strenuous exercises or activities that increase the risk of falls or abdominal trauma. Physical activities requiring heavy lifting or prolonged standing often harm you and your baby.
- Hot Tubs and Saunas: Stay away from hot tubs and saunas, as exposure to high temperatures harms the baby, especially in the third trimester. High temperatures exacerbate conditions like varicose veins and spider veins.
- Toxic Chemicals: Avoid exposure to harsh chemicals such as pesticides, solvents, and some household cleaners. Chemical substances pose risks to the mother and the developing baby.
- Cat Litter: If you have cats, avoid changing the litter box to prevent toxoplasmosis, a parasitic infection that affects your pregnancy.
- Stress: Managing stress is important in the third trimester. Avoid stressors and practice relaxation techniques to maintain joint health and overall well-being.
- Hair Dye: Avoid hair dyes to prevent potential exposure to chemicals. Consult your doctor for advice on safe hair treatments.
Follow precautions and contact your healthcare provider to ensure a safe third trimester for you and your baby.
Is It Safe To Travel By Air In The Third Trimester Of Pregnancy?
Yes, it is considered safe to travel by air during the third trimester of pregnancy. Air travel does not increase the risks of adverse pregnancy outcomes, according to the American College of Obstetricians and Gynecologists (ACOG). Pregnant women with medical conditions that require emergency care or worsen during flight, however, must avoid air travel to avoid increasing complication risks.
Pregnant travelers must observe precautions such as reviewing the airline’s policies and flight duration. Most airlines allow women to fly up until 36 weeks of pregnancy, though some have earlier restrictions. Seatbelts must be fastened low across hipbones throughout the flight to minimize the risk of injury from turbulence. Gas-producing foods or drinks are avoided before flight as air travel causes bloating. Consult your healthcare provider to discuss your safety for travel and any preventive measures you must consider.
How Can A Partner Support The Mother During The 3rd Trimester?
A partner can support the mother during the third trimester through emotional and physical support, affection, encouraging healthy habits, and involvement in maternal health. Here are 5 ways a partner can support the mother in the third trimester.
- Emotional Support: Provide emotional support to enhance your partner’s mental and emotional health. Listen, show care, and make an effort to understand the mother’s feelings to reduce anxiety. Spend quality time together to strengthen your bond, be patient, and offer affirming words to ease fears about childbirth and parenting. A partner’s presence during labor and reassurance during difficult moments help provide significant comfort.
- Physical Support: Take on household chores, laundry, and other physical tasks to relieve your partner of daily burdens, especially with heavy lifting or labor-intensive activities like cleaning or making meals. Help manage housework to give your partner more time to rest to help relieve body aches or swollen feet. Ensure that your partner avoids unsafe physical work and has the opportunity to rest and recover as needed.
- Affection: Show your partner affection through small gestures like hugs, gentle touches, hand-holding, or kisses. Offer back or foot massages to provide comfort and relief from pregnancy-related discomforts, such as swelling. Acts of affection help strengthen the bond between partners, reduce stress and anxiety, enhance feelings of being loved and secure, and promote well-being, according to a 2006 study, “Effective social support: Antecedents and consequences of partner support during pregnancy.” Supporting each other through physical affection is especially important for partners during pregnancy.
- Encourage Healthy Habits: Partners positively influence each other’s behaviors, leading to more nutritious choices like increased fruit and vegetable intake. Engage in meal planning, eat together, and regularly exercise as a team to create a supportive environment. Help your partner avoid unsafe foods, and consider quitting unhealthy habits like smoking to maintain a healthy environment for the mother and baby.
- Involvement in Maternal Health: Participating in pregnancy and birth preparations and offering practical and emotional support enhances the bond between partners. Attend prenatal appointments to stay informed about the mother and baby’s health. Take an active role as a birth partner by attending antenatal classes and asking questions during check-ups. Educate yourself by reading pregnancy books and joining midwife visits to help with important decisions. Being actively involved in these activities helps develop joint coping strategies that benefit the mother, partner, and baby.
How To Manage Stress In The Third Trimester Of Pregnancy?
To manage stress in the third trimester of pregnancy, rest, cut back on tasks, stay active, eat well, maintain sleep hygiene, and talk to a professional. Below are ways to manage stress in the last trimester of pregnancy.
- Rest and Relax: Eliminate stressful things and participate in activities that promote relaxation to reduce stress in the morning and evening. Practice relaxation activities like mindfulness and gratitude to further improve emotional well-being, as recommended in the 2016 study “Effects of a Novel Positive Psychological Intervention on Prenatal Stress and Well-being: A Pilot Randomized Controlled Trial,” conducted by Karen Matvienko-Sikar et al. in Ireland and published in Women and Birth journal.
- Cut Back on Tasks: Ask your partner to help with your workload. Pregnant women reported feeling relaxed and comfortable when partners help with cooking, cleaning, or building the baby’s bedroom in the 2020 study “Active husband involvement during pregnancy: a grounded theory,” by Brandon P. Eddy et al. Partner physical support provides additional emotional support, helping mothers navigate pregnancy more easily.
- Get More Exercises: Physical activities boost pregnant women’s overall well-being. Sports help pregnant women become relaxed and psychologically healthy. Aim for at least 150 minutes of moderate physical activity such as walking and Kegel weekly to improve health.
- Eat Well: Foods high in fat and sugar are linked to stress during pregnancy, according to a 2017 study, “The interplay between maternal nutrition and stress during pregnancy: Issues and considerations,” by Karen L. Lindsay et al. and published in Annals of Nutrition and Metabolism. Focus on eating healthy foods like fruits, vegetables, and dairy products. Consume oily fish rich in omega-3 polyunsaturated fatty acids as healthy fats help reduce stress and other depressive symptoms. Take prenatal vitamins containing B-complex, zinc, iodine, chromium, and vitamin D, as your healthcare professional recommends.
- Start a Sleep Routine: Stress and sleep quality during pregnancy are closely linked. Pregnant women are advised to get at least 8 hours of sleep each night, with bedtime around 10:00 pm or earlier, to enhance sleep quality.
- Talk to a Professional: Stress levels during pregnancy peak in certain periods, according to a 2014 study, “Longitudinal study of perinatal maternal stress, depressive symptoms, and anxiety.” Pregnant women are therefore encouraged to consult a mental health professional to monitor symptoms and provide interventions that prevent stress from worsening and progressing after birth.
What Are The Possible Complications That Can Occur In The Third Trimester?
Possible complications that can occur in the third trimester include vaginal infections, urinary tract infections, gestational pemphigoid, gestational diabetes, and hypertensive disorders. Below are complications that can happen in trimester 3.
- Vaginal Infection: Vaginal infections like aerobic vaginitis (AV) typically occur due to vaginal microbiota disturbances. AV is characterized by an abnormal presence of aerobic enteric bacteria, increased inflammation, and impaired epithelial (tissue) maturation, affecting about 4.2% of pregnant women in the 2019 study titled “Aerobic vaginitis in late pregnancy and outcomes of pregnancy” by Cha Han et al. in Tianjin Medical University General Hospital and published in European Journal of Clinical Microbiology & Infectious Diseases. Risk factors include external hemorrhoids during pregnancy and previous infections. AV is often linked to complications during pregnancy, such as premature rupture of membranes (PROM), making vaginal health monitoring essential throughout pregnancy.
- Urinary Tract Infection (UTI): Urinary tract infection (UTI) involves frequent or burning sensations during urination and lower abdominal pain, often caused by hormonal and physiological changes in pregnancy. Elevated progesterone and estrogen levels reduce ureteral and bladder tone, while increased plasma volume leads to lower urine concentration and higher bladder volume, promoting bacterial growth. Physical changes like urethral dilation often cause urinary retention, increasing risks for UTI. UTI occurs most frequently in the third trimester, affecting approximately 78.46% of pregnant women.
- Gestational Pemphigoid: Gestational pemphigoid is a rare autoimmune skin disorder commonly occurring during the second or third trimester of pregnancy. Gestational pemphigoid involves intense itching around the navel, along with red, inflamed bumps (papules), itchy patches resembling hives (urticarial plaques), or itchy, ring-shaped marks (annular target lesions). Pregnant women typically develop blisters with lesions ranging from small vesicles to larger blisters. Gestational pemphigoid is associated with increased risks for preterm birth and fetal growth restriction, according to a 2014 study from Finland titled “Gestational pemphigoid” by Kaisa Tasanen et al. at Oulu University Hospital and published in Orphanet Journal of Rare Diseases.
- Gestational Diabetes Mellitus (GDM): Gestational Diabetes Mellitus (GDM) is characterized by elevated blood sugar levels first recognized during pregnancy, affecting about 15% of pregnancies worldwide, according to a 2022 study titled “Gestational Diabetes Mellitus – Recent Literature Review”. GDM increases risks for conditions like pre-eclampsia, gestational hypertension, cesarean section births, excessive fetal growth (macrosomia), and neonatal breathing difficulties. Monitor your glucose levels for early detection and effective management of GDM.
- Hypertensive Disorders: Preeclampsia (PE) is a pregnancy-related hypertensive disorder occurring after week 20. Symptoms of PE include hypertension (high blood pressure) of 140/90 or higher, protein in the urine, sudden weight gain, persistent headaches, vision changes such as spots or flashing lights, and sudden swelling in the hands, face, or feet. Severe cases sometimes lead to HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), which impacts the liver and blood. Monitoring and controlling blood pressure is critical for managing preeclampsia.
- Preterm Labor: Preterm labor occurs when the mother gives birth before 37 weeks, typically classified as early or late preterm births. Early preterm births occur before 33 weeks, while late preterm births involve delivery between weeks 34-36. Infection-induced inflammation often triggers contractions, membrane rupture, and cervical changes, leading to early delivery. Symptoms of pre-term labor include strong and frequent contractions, menstrual-type cramps, backaches, and pressure without bleeding.
- Premature Rupture of Membranes or PPROM: Premature Rupture of Membranes (PPROM) occurs when the amniotic sac or “water” breaks before 37 weeks of pregnancy. Signs of PPROM include a sudden gush of fluid, maternal fever, rapid fetal heart rate, uterine tenderness, and foul-smelling amniotic fluid. PPROM affects 2-3% of pregnancies and causes about one-third of preterm births, according to a 2021 study from Spain titled “Obstetric and Perinatal Outcomes after Very Early Preterm Premature Rupture of Membranes (PPROM)-A Retrospective Analysis over the Period 2000–2020,” by Ernesto González-Mesa et al. and published in Medicina. Potential complications of PPROM include placental abruption, cord prolapse, and perinatal mortality. Close monitoring with your OBGYN is essential to avoid further risks to you and your baby’s health.
- Placental Abruption: Placental abruption involves placental detachment from the uterus before delivery, leading to significant vaginal bleeding and fetal oxygen deprivation. Symptoms include abdominal pain, heavy bleeding, and uterine tenderness. Placental abruption often leads to complications like low birth weight, developmental delays, and neonatal mortality. Monitoring signs of placental abruption is crucial, especially for women with risk factors such as high blood pressure, smoking, or a prior placental abruption.
- Placenta Previa: Placenta previa is characterized by a low-lying placenta near or over the cervix, leading to painless bleeding as the lower uterine segment (LUS) and cervix develop. Placenta previa is associated with placenta problems like placental abruption and often leads to serious complications like postpartum hemorrhage or, in rare cases, maternal death. In cases of significant bleeding, an emergency cesarean delivery is typically required to ensure maternal and fetal safety. Always consult your OBGYN for proper testing and management if you experience vaginal bleeding during pregnancy.
- Malpresentation: Fetal malpresentation occurs when the fetus is not in the vertex (head first) position during labor. The most common malpresentation is the breech presentation (feet or buttocks present first), affecting about 3-4% of deliveries, according to a 2017 study titled “Fetal Malpresentation and Malposition: Diagnosis and Management” by Aaron B. Caughey, M.D., et al. in Oregon Health & Science University and published in Obstetrics and Gynecology Clinics of North America. Key risk factors include premature birth, congenital anomalies, placenta previa, and uterine anomalies. Breech malpresentation often leads to cesarean section births, as vaginal deliveries increase risks for head entrapment and birth trauma. The external cephalic version (ECV) is sometimes attempted by healthcare providers to manually rotate a breech fetus to a safer position, helping to reduce complications during childbirth.
- Intrauterine Growth Restriction (IUGR): Intrauterine Growth Restriction (IUGR) occurs when fetal growth falls below the expected pattern for gestational age. Major contributing factors include maternal age, hypertension, diabetes, substance abuse, infections, reduced blood flow, placental dysfunction, chromosomal abnormalities, congenital diseases, and genetic factors. IUGR poses several risks for the baby, including fetal growth restriction, lower birth weight, and higher risks of health problems and neonatal death.
- Vaginal Bleeding: Vaginal bleeding, especially when accompanied by severe cramping, contractions, and lower back pain, raises concern for maternal well-being. Multiple episodes of heavy bleeding, abdominal pain, or tightening in the uterus typically indicate complications like miscarriage or ectopic pregnancy. Bleeding events later in pregnancy are often linked to serious conditions like lower birth rate and perinatal death, making prompt medical care essential if bleeding or severe cramping occurs.

How Is Fetal Growth Restriction Diagnosed?
Fetal growth restriction (FGR) is diagnosed depending on the country’s clinical guidelines. The American guideline defines FGR as a fetal estimated weight less than the 10th percentile for the same gestational age, gender, and race. FGR is typically diagnosed using prenatal ultrasounds and Doppler ultrasonography. The fetal abdominal circumference, femur length, and biparietal diameter are measured using a two-dimensional ultrasound. A Doppler ultrasonography identifies abnormalities in the umbilical cord and placenta that limit the baby’s growth, according to a 2018 study from Canada titled “Screening for fetal growth restriction and placental insufficiency,” by Melanie C. Audette et al., published in Seminars in Fetal & Neonatal Medicine.
Some countries diagnose FGR when the baby exhibits signs of malnutrition and growth restriction, regardless of fetal weight. FGR is differentiated from small for gestational age (SGA), a condition where the baby’s estimated weight is less than the 10th percentile of the same gestational age, gender, and race. SGA babies are diagnosed with FGR only if malnutrition and in-utero growth retardation are present at the time of the birth. Babies whose weight is normal are considered FGR if there are features of malnutrition and growth retardation.
Symmetrical FGR is diagnosed when all the baby’s growth parameters (e.g., length, weight, head circumference) are proportionally reduced. Asymmetrical FGR is diagnosed when the baby’s abdominal circumference is reduced while other measurements are relatively normal.
Asymmetrical FGR is often diagnosed in the late second or third trimester of pregnancy, with preeclampsia (a hypertensive disorder after 20 weeks of pregnancy) as the primary cause. High blood pressure reduces blood flow in the placenta, resulting in a smaller fetal liver and less fat tissues but relatively normal brain growth.
What Prenatal Tests Are Needed In The Third Trimester?
Prenatal tests needed in the third trimester include routine ultrasound, maternal checkup tests, vaccinations, amniocentesis, and GBS screening.
- Routine Third-Trimester Ultrasound: Routine third-trimester ultrasound scans are typically conducted between 30-33 weeks but are possible throughout pregnancy. Ultrasound scans help assess the baby’s head position in relation to the pelvis and detect malformations not visible earlier, including urogenital and cardiac issues. Abnormalities from infections, late-presenting neurological conditions, and fetal growth restriction (FGR) are identified with ultrasound scans to prevent adverse fetal outcomes.
- Maternal Checkup Tests: Blood tests include a complete blood count (CBC) to screen for conditions like anemia and infections, such as HIV, syphilis, and hepatitis B. The Rhesus (Rh) factor blood test checks for Rh incompatibility to identify if the mother produces antibodies that attack fetal red blood cells. Urine tests, such as urinalysis and urine culture, check for protein, sugar, and infections to screen for complications like preeclampsia, gestational diabetes, and urinary tract infections.
- Vaccinations: Live vaccines, especially for conditions like German measles (Rubella) and Chickenpox (Varicella), are typically recommended before and after pregnancy to reduce risks of perinatal infections and congenital anomalies. Women are recommended to undergo pre-pregnancy screenings to identify virus susceptibility and receive vaccinations before conception. OBGYNs usually advise waiting for at least 4 weeks postvaccination before trying to conceive. If virus susceptibility is detected during pregnancy, the first vaccine dose is immediately administered after delivery to prevent neonatal exposure and infection.
- Amniocentesis (Amnio Test): Amniocentesis is conducted anytime after 15 weeks of pregnancy to analyze amniotic fluid for intra-amniotic fetal infection, open neural tube defects (ONTDs) like spinal muscular atrophy, and genetic disorders, such as cystic fibrosis. Amniocentesis involves carefully inserting a sterile needle into the abdomen with the guidance of ultrasound to collect fluid from the amniotic sac for examination.
- Group B Strep (GBS) Screening: Group B Streptococcus (GBS) is a harmful bacteria leading to complications like maternal chorioamnionitis, endometritis, and newborn infection. GBS screening typically involves a single vaginal and rectal swab performed between 35-37 weeks of pregnancy.
How Often Are Ultrasound Scans Recommended?
One routine ultrasound scan before 24 weeks of pregnancy is recommended to assess gestational age, detect fetal anomalies and multiple pregnancies, reduce the likelihood of labor induction for post-term pregnancies, and improve overall pregnancy experience, according to the 2016 World Health Organization Recommendations on Antenatal Care For a Positive Pregnancy Experience. Ultrasound scans after 24 weeks are typically offered only for pregnant women who have not had a scan in the recommended weeks, while repeat scans are necessary for mothers with high-risk pregnancies.
First-trimester scans (up to 13 weeks) confirm viability, establish gestational age and number of fetuses, and determine whether babies in multiple pregnancies share the same placentas (chorionicity) and amniotic sacs (amnionicity). Second-trimester scans (between 18 and 24 weeks) allow for a detailed assessment of fetal anatomy and anomalies, identify placental location, and estimate gestational age. Third-trimester scans typically performed between 30-33 weeks, monitor fetal position and detect complications like fetal growth restriction or late-presenting anomalies, such as neurological malformations.
Repeat scans are typically recommended in the presence of concerns like fetal bradycardia (abnormally slow heart rate) to further determine fetal viability. Babies with abnormal cardiac output often require repeat scans until the heartbeat stabilizes or becomes absent. Women who experience trauma, injuries, or symptoms like severe vaginal bleeding and pelvic pain often require additional evaluations to monitor the mother and baby’s health.
When Should You Contact Your Doctor If Something Feels Unusual?
Contact your doctor if something feels wrong in the third trimester of pregnancy or if you experience symptoms like fever, persistent headaches, decreased fetal movement, severe nausea, or extreme swelling. Here are 6 symptoms you must report to your OBGYN in the third trimester.
- Fever Over 100.4°F (38°C): A fever over 100.4°F often signals an infection and is associated with fetal risks like neural tube defects, congenital heart defects, and oral clefts, based on a 2014 study, “Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring,” conducted by Anne-Marie Nybo Andersen, Gabriele Berg-Beckhoff, and Julie Werenberg Dreier and published in Pediatrics. Fever accompanied by weakness, fatigue, muscle aches, severe headache, or cold symptoms, sometimes signals the flu or COVID-19, requiring immediate medical attention to protect mother and baby.
- Severe Headaches: Severe, persistent headaches often indicate preeclampsia (high blood pressure after 20 weeks gestation), especially if accompanied by vision changes, dizziness, confusion, or fainting spells. Preeclampsia causes a spike in the mother’s blood pressure, leading to severe complications if left untreated.
- Decreased Fetal Movement: Sudden changes in your baby’s movements often indicate complications like fetal growth restriction, stillbirth, or declining health. Pay close attention to fetal movements and contact your OBGYN if your baby moves less than normal (fewer than ten movements per hour).
- Severe Vomiting or Nausea: Severe vomiting often indicates hyperemesis gravidarum (HG), a serious condition beyond normal morning sickness. HG leads to dangerous dehydration and causes dizziness, dry mouth, significant weight loss, and complications like electrolyte imbalances or preeclampsia. Symptoms such as severe dizziness, heartburn, or the sensation of food caught in the throat or chest typically signal serious gastrointestinal issues. Call your OBGYN if you’re experiencing severe nausea and vomiting that stops you from eating or drinking.
- Extreme/Sudden Swelling: Sudden and extreme swelling in the face and hands often signal preeclampsia, a serious condition marked by high blood pressure. Other symptoms include persistent headaches, confusion, blurred vision, fainting, and sudden weight gain. If untreated, preeclampsia poses serious consequences for you and your baby. Seek immediate medical attention if you experience any of these symptoms.
- Heavy Vaginal Bleeding: Vaginal bleeding during pregnancy typically indicates complications like placental abruption (early detachment of the placenta from the uterine wall) or placenta previa (placenta implants near the cervical opening), which commonly occurs in the third trimester. Contact your OBGYN immediately if heavy bleeding occurs.
When Can You Feel That Your Body Is Preparing For Labor?
You can feel that your body is preparing for labor when there is blood, cramping, water breaking, increased body pains, or baby drops. Below are the signs you can feel when your body prepares for labor.
- Bloody Show: Bloody shows involve a blood-stained vaginal discharge resulting from the loss of mucus plug in the cervix. Pregnant women sometimes report a bloody show three days before labor onset.
- Cramping: Cramps and abdominal tightening often occur from uterine contractions. Contractions lasting from 30-90 seconds, constantly becoming stronger, and occurring regularly every 3-5 minutes typically signal the first stage of labor. True labor contractions include cervical dilations (widening), unlike Braxton-Hicks contractions (practice contractions), which are often painless, sporadic, and do not cause cervical changes.
- Waters Breaking: Rupture of amniotic membranes, or “waters breaking,” is characterized by vaginal fluid leakage, which is sometimes mistaken as urine. Tests like sterile speculum exam and pH testing are often conducted to verify membrane rupture. Contact your OBGYN immediately when experiencing fluid leakage during the third trimester.
- Increased Body Pains: Increased body pains, particularly low back pain and lower abdominal pain, occur during labor due to hormones and the baby’s position. The relaxin hormone loosens the joints, and the baby presses into the spine, triggering low back pain that intensifies as labor progresses. Most mothers (54.29%) reported muscle pain and soreness, while some (45.7%) feel continuous back pain during labor, according to a 2008 study titled “Low Back Pain During Labor and Related Factors” by Ya-Ling Tzeng et al., published in Journal of Nursing Research. Sharp pains in the pelvic, vaginal, and perineal areas occur as the baby descends through the birth canal.
- Baby Drops: Baby drops (lightening) occur as the baby descends and settles into the pelvis, signaling preparedness for birth. The baby’s descent eases pressure in the stomach and the lungs but increases bladder and pelvic pressure, leading to a “lightening” sensation as the body prepares for labor.
- Cervix Dilates: Cervical dilations (widening) and effacement (thinning) occur to assist the baby’s delivery. A digital cervical exam is often performed to assess cervical dilations, in which an OBGYN inserts two fingers in a v-shape to estimate cervical opening width. Cervical dilations measure from 0-10 cm, with 10 cm indicating full dilation and preparedness for delivery.
- Diarrhea: Diarrhea is characterized by an increased urge to go to the toilet alongside loose and watery stools. Diarrhea during the final weeks of pregnancy often indicates approaching labor as prostaglandins, the hormones facilitating cervical ripening, increase. Elevated prostaglandins cause intestinal contractions, leading to frequent bowel movements.
- Mucus Plug Discharged: The mucus plug fills the cervical canal, preventing vaginal bacteria from entering the uterus and reducing risks for infection and preterm labor. Cervical changes like dilations (widening) and softening lead to the loss of mucus plug, signaling that labor is near.
- Nesting: Nesting is characterized by a sudden urge to prepare a suitable home for the baby. Mothers typically express the urge to nest during the third trimester, exhibiting a surge of energy to clean and organize household spaces in preparation for the baby’s arrival. Nesting is associated with hormonal fluctuations and serves as a protective instinct for the vulnerable baby, according to a 2020 study titled, “Nesting behaviours during pregnancy: Biological instinct, or another way of gendering housework?” by Arianne Shahvisi Brighton at Sussex Medical School and published in Women’s Studies International Forum.
How To Prepare Yourself Going Into Labor?
To prepare yourself for labor, learn the different labor types, create a birth plan, practice relaxation techniques, balance activity and rest, take birth classes, keep yourself comfortable, and assign a birth support person. Below are the different ways to prepare yourself for labor.
- Learn Different Labor Positions: Learn and practice different labor positions, such as upright and supine positions. Upright labor positions include standing, kneeling, or squatting, while supine positions involve lateral or hand-and-knee positions. Women in an upright position had more regular contraction patterns, leading to a shorter labor period, according to a 1990 study titled “Maternal Position, Labor, and Comfort” by Claire M. Andrews et al. in Case Western Reserve University, published in Applied Nursing Research. Consider birthing ball exercises to practice upright positions. The exercise stretches and strengthens the muscles, encouraging a smoother fetal descent and shorter labor. Have your birth plan ready, and always discuss your preferences with your OBGYN or midwife.
- Create a Birth Plan: A birth plan contains your labor and delivery preferences, including your chosen pain management interventions and birthing positions. Preparing a birth plan ahead helps calm your mind and empower you during labor and childbirth. Attending childbirth classes offers a helpful guide in creating a birth plan, according to a 2020 study titled “Primiparous women’s knowledge and satisfaction based on their attendance at childbirth preparation classes” by Robab Hassanzadeh et al. and published in Nursing Open Journal.
- Use Relaxation Techniques: Relaxation improves emotional well-being, leading to reduced anxiety, depressive symptoms, and worries, according to a 2012 study from Switzerland titled, “Relaxation during pregnancy: what are the benefits for mother, fetus, and the newborn? A systematic review of the literature” by Nadine S. Fink et al. and published in The Journal of Neonatal and Perinatal Nursing. Take warm baths or a hot compress to relieve muscle aches and pains. Consider learning breathing techniques like abdominal breathing, counted breathing, and engaged breathing to help you work through contractions and stay in control during labor.
- Balance Activity and Relaxation: Engage in physical activities while resting and taking breaks as needed. Physical activities like long walks and stretching help reduce exhaustion during childbirth and prevent risks of needing artificial labor induction and episiotomy (small cut between the vagina and perineum during delivery). Try exercises like rocking on a birth ball during the final 4-6 weeks of pregnancy, which is associated with an increased likelihood of vaginal delivery, according to a 2015 study titled “The Effect of Birth Ball Exercises during Pregnancy on Mode of Delivery in Primiparous Women” by Mohammad Taghi Shakeri in Mashhad University of Medical Sciences and published at the Journal of Midwifery and Reproductive Health.”. Consider relaxation techniques like yoga, massage, and guided imagination to help calm yourself and reduce stress and anxiety before labor.
- Go to Birthing Classes: Childbirth classes help expecting parents gain knowledge and confidence about labor, childbirth, and parenting. Parents understand what to expect during labor, allowing for informed decisions about important matters like pain management techniques and reducing anxiety, according to a 2017 study titled “Perceived Benefits of Childbirth Education on Future Health-Care Decision Making,” by Jane Leach et al. and published in The Journal of Perinatal Education.
- Keep Yourself Comfortable: Consider using lumbar support to improve seating posture. Keep your feet elevated on a small stool to help ease physical discomfort, which worsens as labor approaches. Take naps, rest in bed as needed, and prepare sleeping pillows to support your spine, abdomen, and legs. Heat therapy, such as warm baths or showers and heat pads, helps manage symptoms like back pain, insomnia, and headaches. Make sure to consult your OBGYN for personalized advice.
- Have a Birth Support Person: Call a birth support person, such as your partner, to assist with labor and help prepare essentials for your baby’s delivery. Attend prenatal appointments and join birthing classes to ensure you and your partner are actively involved and well-informed about the pregnancy. Active husband involvement during pregnancy is linked to stronger trust, communication, and support, which helps maintain a healthy relationship after childbirth, according to a 2020 study titled “Active husband involvement during pregnancy: a grounded theory,” conducted by Brandon P. Eddy et al. in Texas Tech University and published at Family Relations.
What Weeks In The 3rd Trimester Should You Be Admitted For Labor?
Women are typically admitted to the hospital between 37-42 weeks (full-term) of pregnancy for labor. Common symptoms during full-term labor include regular contractions in increasing intensity, cervical dilation, vaginal bleeding, and fluid leakage.
Some mothers are admitted to the hospital earlier than 37 weeks of pregnancy due to complications. Women in preterm labor (labor before 37 weeks) must be hospitalized to check for cervical dilation (widening) and fetal well-being. Mothers in preterm labor after 34 weeks of pregnancy are typically discharged if the cervix has not dilated or if there are no signs of complications.
Preterm premature rupture of membranes (PPROM), the spontaneous rupture of the amniotic sac before 37 weeks of pregnancy, is another condition that requires early hospitalization. The healthcare provider checks the mother for signs of labor, infection, placental abruption, and umbilical cord compression. Maternal vital signs and fetal well-being are monitored to check for complications.
Women with heavy or continuous vaginal bleeding at 36 weeks of pregnancy or greater require immediate hospitalization for a cesarean section. The vaginal bleeding is typically caused by placenta previa (the placenta covers the opening of the cervix) and increases the risks of a hemorrhage (blood loss) and death among the mother and the baby, making hospitalization necessary.
Attend prenatal appointments and regularly consult your OBGYN to know when to go to the hospital for labor. Discuss with your healthcare provider what to expect and where to go during labor onset.
How Common Is Preterm Labor?
Preterm labor is not common. Preterm labor occurs in 10.23% of pregnancies in the United States, affecting one out of 10 babies in 2019. Early preterm cases accounted for 2.77%, while late preterm cases made up 7.46%, according to a 2020 study from The United States titled “Preterm Labor and Birth,” by Kellie M Griggs et al., published in the American Journal of Maternal/Child Nursing. Preterm labor affects over 15 million pregnant women worldwide, according to a 2018 report by the World Health Organization.
Preterm labor involves regular uterine contractions and cervical dilation (opening) before 37 weeks of pregnancy. Early preterm labor occurs before 34 weeks of pregnancy, while late preterm labor occurs between 34-36 weeks.
Infection is a leading cause of preterm labor, with conditions like chorioamnionitis triggering hormone release that initiates labor. Other risks include premature rupture of membranes (PPROM), placental abruption, placenta previa, and vaginal bleeding. Maternal factors such as smoking, age (under 18 or over 40), poor nutrition, low body mass index, and environmental influences contribute. Fetal anomalies, growth restriction, and abnormal amniotic fluid levels further increase the risk of preterm labor.
What Does parentingstyles.Com Suggest About The Third Trimester Of Pregnancy?
parentingstyles.com suggests five key practices for the third trimester of pregnancy. First, stay active by engaging in light exercise such as walking or stretching to promote physical stamina, which helps during labor and delivery. Second, prepare for breastfeeding by learning about proper latching techniques, recognizing feeding cues, and familiarizing yourself with available lactation support. Third, practice relaxation techniques such as deep breathing or meditation to help manage anxiety and prepare for the childbirth process. Fourth, get adequate rest, as fatigue often increases during the third trimester, and good sleep is vital for the mother and baby’s health. Lastly, finalize the birth plan, including labor, delivery, and postpartum care preferences, and communicate these plans with your OB/GYN.
parenting styles offers online classes on parenting, child development, and child psychology. parenting styles was founded by Pamela Li, a Stanford-trained parenting specialist in child development, behavior, and mental health, and the Editor-in-Chief of parentingstyles.com. parenting styles empowers parents with research-backed information and guidance, including week-by-week pregnancy updates, parenting practices, and child psychology. parenting styles emphasizes user privacy and does not sell personal information.