1 Week Pregnant Symptoms: Week 1 Of Pregnancy And Preconception Tips
1 week pregnant symptoms do not exist because you are not pregnant yet. 1 week pregnancy symptoms are your menstrual symptoms when you are having your period. The first week of pregnancy is calculated from the start of your last menstrual period (LMP). Ovulation and conception usually happen at the end of week 2 or the beginning of week 3.
1 week pregnant marks the start of gestation in pregnancy. Week one of pregnancy starts on the first day of the mother’s last menstrual period (LMP). You are having your period now, and conception has not occurred yet. Therefore, the first week of pregnancy is often considered the “pre-pregnancy” phase. The uterus’s endometrium, or lining, is shed and expelled from the body as menstrual blood during menstruation. This process clears the way for the new cycle to begin. The body prepares a new lining as the old one is shed.
The endometrium thickens in week 1 in anticipation of a fertilized egg. This is called the follicular phase. The hormone follicle-stimulating hormone (FSH) stimulates the growth of several follicles in your ovaries during the follicular phase. Each follicle contains an immature egg.
Ovulation typically occurs 14 days (2 weeks) after the first day of LMP in a 28-day cycle. A mature egg cell (ovum) is released from the ovary during ovulation. The egg (zygote) travels down the fallopian tube and implants in the uterine lining if fertilization occurs, marking the start of pregnancy.
You are technically not pregnant at week one of pregnancy. The changes in your body are due to menstruation, not pregnancy. These changes prepare your body for ovulation, fertilization, and implantation, such as bleeding, hormonal changes, cervical mucus thinning, and low basal body temperature. Tracking basal body temperature (BBT) and monitoring cervical mucus are common methods to predict ovulation, aiding conception efforts.
Preconception health of the mother and father affects conception, pregnancy, and birth outcomes. Mothers and fathers with good preconception health reduce the risks of having low birthweight or preterm infants. Adequate folic acid intake, maintaining a healthy diet, and avoiding harmful substances like alcohol and tobacco are critical preconception care for both parents. Regular physical activity and stress management contribute positively to preconception health. Consulting an OBGYN (OB-GYN or obstetrician-gynecologist) before trying to conceive and managing existing medical conditions improves pregnancy outcomes.
What are the Early Pregnancy Symptoms?
1 week pregnant pregnancy symptoms do not exist because conception and fertilization have not occurred yet. Early pregnancy symptoms at one week of pregnancy are menstrual symptoms, such as abdominal cramping, lower back pain, and bloating. The first week of pregnancy is calculated from the start of your last menstrual period (LMP), and ovulation and conception usually happen around week 2 or 3.
What Is The Importance Of Understanding Being 1 Week Pregnant?
The importance of understanding what it means to be one week pregnant lies in knowing that prenatal care begins even before conception. Your preconception actions and lifestyle choices affect your baby. Whether you smoke, drink, use drugs, or take folic acid now matters. Whether you maintain a healthy weight and manage stress affects pregnancy outcomes. These lifestyle choices affect your baby’s health from the beginning because major organs start forming very early, often before a woman realizes she is pregnant. For example, neural tube defects, caused by the failure of the neural tube to close properly, occur in the early stages of pregnancy.
It is important for women who try to conceive to track their menstrual cycle and estimate the ovulation day, which is the fertile window for successful conception. Monitoring your basal body temperature (BBT) or hormonal changes, such as luteinizing hormone (LH) surges, allows you to pinpoint ovulation further.
Knowing how to count pregnancy weeks lets you estimate your baby’s estimated due date (EDD) once conceived. Adding 280 days to the LMP is your baby’s EDD. When accurate LMP is not available, gestational age is determined using ultrasound measurements in early pregnancy, according to a 2020 study, “Estimating the Beginning of Pregnancy in German Claims Data: Development of an Algorithm With a Focus on the Expected Delivery Date,” published in Frontiers in Public Health.
Tracking your pregnancy week by week helps you start complementary prenatal care early. Prenatal care practices to incorporate now include eating nutritious foods, taking prenatal vitamins, especially folic acid, exercising regularly, and seeking medical advice to address pre-existing health conditions. Monitoring for symptoms and identifying pregnancy signs allows you to recognize early signs of pregnancy in the next few weeks, seek medical advice, engage in family planning, and be emotionally prepared for the upcoming changes early.
Being aware of your body’s changes during week 1 pregnancy empowers you to manage your pregnancy timeline, prioritize your health, and prepare for early pregnancy care.
What To Expect When 1 Week Pregnant?
1 week pregnant, expect to have your period with vaginal bleeding. The duration and symptoms of a menstrual cycle vary from person to person. A typical menstrual cycle lasts 28–29 days. The most common side effects of menstruation include heavy menstrual bleeding, abdominal and pelvic cramps (dysmenorrhea), tender breasts, bloating, tiredness, nausea, headaches or migraines, constipation, and fluctuating mood, according to a 2019 study, “The impact of menstrual symptoms on everyday life: a survey among 42,879 women,” published in the American Journal of Obstetrics and Gynecology.
Hormonal changes are significant at week 1 as estrogen and progesterone levels drop, leading to the shedding of the uterine lining. The body begins to prepare for the next cycle by maturing new follicles in the ovaries. Maintaining a healthy diet and staying hydrated help manage discomfort. Some women experience lower back pain and food cravings during this time, which are common menstrual symptoms or first-trimester symptoms before conception.
When Does Pregnancy Start?
Pregnancy is calculated from the first day of a woman’s last menstrual period (LMP). Ovulation and conception usually happen around two weeks later. The gestational age, calculated from the LMP, helps healthcare providers estimate the baby’s due date and track pregnancy progress.
Gestational age is a standardized way to discuss pregnancy timelines and developmental milestones. Conception occurs during ovulation, around 12-14 days after LMP in a typical 28-day cycle. During ovulation, an egg is released from the ovary and is available for fertilization by sperm.
Understanding the difference between gestational and fetal age is important for interpreting medical information and ultrasound results. While gestational age starts from the LMP, fetal age refers to the growing baby’s actual age from conception. Fetal age is typically about two weeks less than gestational age.
This distinction is crucial for prenatal care and medical assessments, as various tests and screenings are scheduled based on gestational age. Accurate dating impacts the management of the pregnancy, including identifying potential complications early and planning appropriate interventions.
How Does Preconception Health Impact Week 1 Of Pregnancy?
The preconception health of the mother and father impacts week 1 of pregnancy by affecting the egg qualities, sperm qualities, hormonal balances, and reproductive organs’ health. Preconception health is the physical and mental health of men and women during their reproductive years before conception.
For example, women with poorly controlled diabetes, defined as glycosylated hemoglobin (HbA1C) levels above 8.4 percent, experience a 32 percent of pregnancy loss and a sevenfold risk of fetal anomalies compared to women with well-controlled diabetes, according to a 2002 study titled “Preconception Health Care” by S.C. Brundage, published in American Family Physician. Poor mental health in women is associated with an increased risk of pregnancy complications, as shown in the 2012 study “Preconception Mental Health Predicts Pregnancy Complications and Adverse Birth Outcomes: A National Population-Based Study,” published in the Maternal and Child Health Journal.
Optimizing preconception health in women and men increases the chances of a successful pregnancy and reduces the risk of complications in the early weeks and beyond. This includes maintaining a balanced diet, regular exercise, and avoiding harmful substances like tobacco, alcohol, and drugs.
Men’s preconception health is critical. Poor lifestyle choices, such as smoking and excessive alcohol consumption, negatively impact sperm quality, according to a 2018 study, “The effect of paternal factors on perinatal and pediatric outcomes: a systematic review and meta-analysis” by Anja Pinborg, Hannele Laivuori et al., published Human Reproduction Update.
Mothers and fathers’ mental health is essential, as stress and anxiety affect hormonal balance and fertility. Genetic factors influenced by preconception health plays a role in early embryonic development. Ensuring both parents are in optimal health helps prevent genetic anomalies and contributes to the overall health of the embryo.
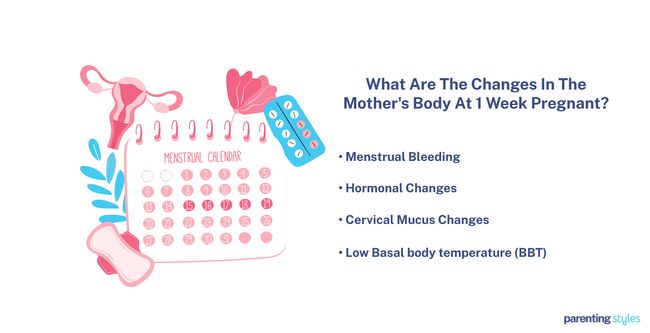
What Are The Changes In The Mother’s Body At 1 Week Pregnant?
There are 5 changes in the mother’s body at 1 week pregnant. Technically, there are no changes in the mother’s body due to pregnancy because you are not pregnant yet, and those symptoms are related to menstruation.
- Menstrual Bleeding: You are having your period as the body sheds the uterine lining prepared for a potential pregnancy that did not happen in the last cycle. Menstruation-related symptoms include mild pelvic cramps, tender breasts, bloating, tiredness, headaches or migraines, and fluctuating mood. This phase is characterized by a drop in progesterone and estrogen levels, leading to the shedding of the endometrial lining.
- Hormonal Changes: Hormonal changes during this week are regulated by the hypothalamus and the pituitary gland. The hypothalamus releases a hormone called GnRH (gonadotropin-releasing hormone), which stimulates the pituitary gland to produce two other hormones: FSH (follicle-stimulating hormone) and LH (luteinizing hormone). FSH helps the ovarian follicles grow, while LH causes ovulation. This period is called the follicular phase. At the same time, levels of estrogen and progesterone change, preparing the body for ovulation.
- Low Basal body temperature (BBT): The mother’s immune system remains vigilant while her body temperature fluctuates slightly. Some women notice a lower basal body temperature. BBT is lowest at the beginning of week 1 due to a lower progesterone level, according to a 2019 study, “Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles,” published in Digital Medicine. Tracking BBT helps identify the start of the fertile window, which is useful for those trying to conceive.
- Cervical Mucus Changes: The cervical mucus changes consistency, becoming thinner and more slippery to help sperm reach the egg. Rising estrogen levels influence this change, making the cervical environment more conducive to sperm movement.
- Psychological and Emotional Changes: Many women experience mood swings, irritability, or heightened emotions during this time, often due to hormonal fluctuations. Managing stress through relaxation techniques or light exercise is beneficial.
Understanding these bodily changes and pre-pregnancy symptoms helps you manage menstrual health and optimize fertility. Pregnancy symptoms begin to appear around the 4th to 6th week of pregnancy when the body produces pregnancy hormones after successful implantation.
When do Pregnancy Symptoms Start to Show?
Pregnancy symptoms start to show typically when you miss the next period, which is 2 weeks after conception or 4 weeks after LMP. By then, you are at the beginning of week 5 of pregnancy. However, pregnancy symptoms start to show at different times for different women. Some women experience few or no noticeable symptoms in the early weeks.
When to Take a Pregnancy Test?
Take a pregnancy test when you miss your period 4 weeks after your last menstrual period (LMP). At-home pregnancy tests that detect human chorionic gonadotropin (hCG) are taken as early as four days before an expected period. Home pregnancy tests offer the ability to detect pregnancy earlier than the traditional method of waiting until after a missed period, according to a 2014 study, “Strips of Hope: Accuracy of Home Pregnancy Tests and New Developments,” conducted in Germany by C. Gnoth and S. Johnson and published in Geburtshilfe und Frauenheilkunde. Researchers cautioned that tests claiming to detect pregnancy eight days before a missed period are often unrealistic due to the variability in hCG levels in early pregnancy.
Are Pregnancy Tests Accurate?
Yes, pregnancy tests are generally accurate, but the accuracy depends on timing, medication, test sensitivity, proper use, test format, laboratory vs home use, and storage.
Taking a test too early in pregnancy sometimes results in a false negative, as there is likely not enough hCG in the urine to be detected. Certain medications containing hCG (e.g., fertility treatments) and rare conditions like ovarian tumors cause false positive results. Tests of different brands have varying sensitivities to hCG. Incorrect test use, such as not following the instructions or misinterpreting the results, leads to inaccurate readings. The test format (strip, cassette, or midstream) sometimes affects accuracy, with midstream tests generally being easier to use and interpret. The accuracy of home pregnancy tests is lower when used by individuals at home compared to laboratory settings. Improper storage of the test tends to affect the results.
What Are The Tips For Increasing Chances Of Getting Pregnant?
Here are 10 tips for increasing the chances of getting pregnant and reducing infertility risk factors, according to a 2018 research, “What do people know about fertility? A systematic review on fertility awareness and its associated factors,” published in Upsala Journal of Medical Sciences. The chances of getting pregnant depend on many factors, such as timing, lifestyle, and medical considerations.
- Track Timing of Ovulation: Tracking your menstrual cycle to identify your most fertile days increases your chances of getting pregnant. Ovulation typically occurs around the 14th day of a 28-day cycle. Track your menstrual cycle by monitoring basal body temperature, using ovulation prediction kits, or using a fertility tracking app.
- Stop Birth Control: Don’t forget to stop taking birth control pills or remove intrauterine devices (IUDs) if you have been using them previously so that your body returns to its natural reproductive rhythm.
- Manage Stress: High levels of stress interfere with ovulation and conception. Practice relaxation techniques like yoga or meditation.
- Maintain a Healthy Weight: Being overweight (obesity) or underweight affects hormone levels and ovulation.
- Exercise Regularly: Moderate exercise is beneficial for overall health and fertility.
- Stay Hydrated: Drink plenty of water to maintain optimal body functions.
- Conduct Preconception Checkup: Talk to your doctor about your medical history, medications, and any underlying health conditions that affect fertility.
- Check Medications: Check with your medical provider about any medications you are taking that affect fertility.
- Address Underlying Medical Issues: Certain medical conditions, such as polycystic ovary syndrome (PCOS) or endometriosis, affect fertility.
- Encourage Healthy Partner: Encourage your partner to adopt healthy habits, as male fertility plays a significant role in conception.

Are Prenatal Vitamins Important for Conception?
Yes, prenatal vitamins are important for conception by improving egg quality and sperm health and for post-conception by preventing pregnancy complications, such as anemia, depression, gestational diabetes, hypertension, preeclampsia, and premature rupture of membranes. These findings are found in a 2022 study, “Evidence-based recommendations
for an optimal prenatal supplement for women in the US: vitamins and related nutrients,” published in Maternal Health, Neonatology, and Perinatology.
Preconception, adequate intake of essential vitamins and minerals improves the health and quality of a woman’s eggs, increasing the likelihood of successful fertilization. For example, folic acid is crucial for DNA synthesis and repair in healthy eggs. Vitamins and minerals such as vitamin D, iron, and omega-3 fatty acids help maintain hormonal balance, which is crucial for ovulation. Zinc, selenium, and vitamin C improve male fertility by improving sperm quality, motility, and count.
Postconception, taking prenatal vitamins, such as folic acid, reduces the risk of neural tube defects in the developing baby. The Centers for Disease Control and Prevention (CDC) recommends that all women of reproductive age consume 400 mg (micrograms) of folic acid daily to prevent such defects.
Here are 10 prenatal vitamins and minerals important for conception, according to the American College of Obstetricians and Gynecologists (ACOG). ACOG is a professional association of physicians specializing in obstetrics (pregnancy, childbirth, and postpartum care) and gynecology (women’s reproductive health).
- Calcium (1,000 milligrams for ages 19 to 50): Builds strong bones and teeth.
- Iron (27 milligrams): Helps red blood cells deliver oxygen to your fetus.
- Iodine (220 micrograms): Essential for healthy brain development.
- Choline (450 milligrams): Important for developing your fetus’s brain and spinal cord.
- Vitamin A (770 micrograms for people ages 19 to 50): Forms healthy skin and eyesight and helps with bone growth.
- Vitamin C (85 milligrams for ages 19 to 50): Promotes healthy gums, teeth, and bones.
- Vitamin D (600 international units): Builds your fetus’s bones and teeth and helps promote healthy eyesight and skin.
- Vitamin B6 (1.9 milligrams): Helps form red blood cells and helps the body use protein, fat, and carbohydrates.
- Vitamin B12 (2.6 micrograms): Maintains the nervous system and helps form red blood cells.
- Folic acid (400 micrograms preconception, 600 micrograms during pregnancy): Helps prevent birth defects of the brain and spine and supports the general growth and development of the fetus and placenta.
It’s important to note that taking prenatal vitamins alone doesn’t guarantee conception. Many other factors influence fertility, such as timing, underlying medical conditions, and lifestyle choices. Maintaining a healthy weight, managing stress, and avoiding smoking and excessive alcohol consumption contribute to optimizing fertility.
Before starting a vitamin regime, consult your healthcare provider to ensure the prenatal vitamins you choose are appropriate for your needs.
What Types of Foods are Beneficial to Eat for Preconception?
Here are 10 types of foods that are rich in minerals and vitamins and 5 food groups that are beneficial to eat for preconception and during pregnancy, according to the American College of Obstetricians and Gynecologists (ACOG). ACOG is a professional association of physicians specializing in obstetrics (pregnancy, childbirth, and postpartum care) and gynecology (women’s reproductive health).
Nutrient, Daily Recommended Amount (DRA) for Week 1 Pregnant
Why You Need It in Week 1
Best Sources for First Week of Pregnancy
Calcium (1,000 milligrams for ages 19 to 50)
Builds strong bones and teeth
Pasteurized milk, cheese, yogurt, sardines. Dark green leafy vegetables
Iron (27 milligrams)
Makes red blood cells and helps deliver oxygen to your fetus
Lean red meat, poultry, fish, dried beans and peas, iron-fortified cereals, prune juice
Iodine (220 micrograms)
Essential for healthy brain development
Iodized table salt, dairy products, seafood, meat, some breads, eggs
Choline (450 milligrams)
Important for developing the fetus’s brain and spinal cord.
Beef liver, eggs, soy products, peanuts
Vitamin A (770 micrograms for ages 19 to 50)
Helps form red blood cells. Helps the body use protein, fat, and carbohydrates
Carrots, green leafy vegetables, sweet potatoes
Vitamin C (85 milligrams for ages 19 to 50)
Promotes healthy gums, teeth, and bones
Citrus fruit, broccoli, tomatoes, strawberries
Vitamin D (600 international units)
Builds bones and teeth. Helps promote healthy eyesight and skin
Sunlight, fortified milk, fatty fish such as salmon and sardines
Vitamin B6 (1.9 milligrams)
Helps form red blood cells and helps the body use protein, fat, and carbohydrates.
Beef, liver, pork, ham, whole-grain cereals, bananas
Vitamin B12 (2.6 micrograms)
Maintains nervous system. Helps form red blood cells.
Meat, fish, poultry, milk (vegetarians take a supplement)
Folic acid (400 micrograms preconception. 600 micrograms during pregnancy)
Helps prevent birth defects of the brain and spine and supports the general growth and development of the fetus and placenta.
Fortified cereal, enriched bread and pasta, peanuts, dark green leafy vegetables, orange juice, and beans.
Grains
Sources of folic acid, fiber, iron, and B vitamins.
Oats, barley, quinoa, brown rice, bulgur, and other whole grains products. Whole grains are those that haven’t been processed
Fruits
Sources of vitamins and minerals, antioxidants, and fiber.
Fresh, canned, frozen, or dried fruit. Whole fruit is better than juice.
Vegetable
Sources of calcium, vitamin D, and protein.
Raw, canned, frozen, or dried vegetables or drink 100 percent vegetable juice
Protein
Sources of protein, iron, zinc, and omega-3 fatty acids.
Meat, poultry, seafood, beans, peas, eggs, processed soy products, nuts, and seeds
Dairy
Sources of calcium, vitamin D and protein.
Pasteurized milk and milk products, such as cheese and yogurt.
In week 1, avoid foods you are allergic to or intolerant of. Always consult your OBGYN before changing your diet.
Are there Exercises that a Mother Can Do for Preconception?
Yes, there are exercises a mother can do for preconception (week 1), according to a 2016 study, “The Role of Physical Activity in Preconception, Pregnancy and Postpartum Health” by Leanne M. Redman, Cheryce L. Harrison, Lisa J. Moran et al., published in Seminars in Reproductive Medicine. The findings suggest moderate regular physical activity positively influences fertility and birth rates.
Healthy non-pregnant adults are recommended to do 150-300 minutes of moderate-intensity aerobic physical activity or at least 75-150 minutes of vigorous-intensity aerobic physical activity. This advice is detailed in the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Moderate-intensity aerobic physical activities include walking, running, swimming, and bicycling.
Moderate intensity refers to the physical activity performed between 3 and less than 6 times the intensity of rest on an absolute scale. Moderate-intensity physical activity is usually a 5 or 6 on a scale of 0–10 on a scale relative to an individual’s capacity. Vigorous intensity refers to physical activity performed at 6.0 or more on an absolute scale. Vigorous-intensity physical activity is usually a 7 or 8 on a scale of 0–10 on a scale relative to an individual’s capacity.
Consult your OBGYN when starting or continuing an exercise routine for preconception to ensure your exercise plan is safe and appropriate for your health. Listen to your body and avoid over-exertion. Drink plenty of water before, during, and after exercise to stay hydrated. Include proper warm-up and cool-down sessions to prevent injury.
What are the Things to Avoid if a Mother is Trying to Get Pregnant?
Here are 8 things to avoid if a 1-week-pregnant mother is trying to get pregnant.
- Stress: High levels of stress interfere with hormone production and ovulation. Find healthy ways to manage stress, such as yoga, meditation, or spending time in nature.
- Certain Lubricants: Some lubricants hinder sperm movement and decrease the chances of fertilization. Choose a sperm-friendly lubricant if needed.
- Certain Medications: Some medications interfere with fertility or pose risks during pregnancy. Consult your OBGYN about any medications you are taking.
- Hot Tubs and Saunas: Expectant parents, especially fathers, must avoid high-temperature places, such as saunas and hot tubs, as high temperatures harm sperm.
- Extreme Diets: Rapid weight loss or restrictive diets sometimes disrupt hormone levels and ovulation, making conception more difficult.
- Harmful Substances: Avoid harmful substances, including alcohol, smoking, and recreational drugs like cannabis.
- Excessive Exercise: While moderate exercise is beneficial, excessive or intense exercise negatively impacts ovulation and hormone balance.
- Infections: Untreated infections, especially sexually transmitted infections (STIs), affect fertility and the health of the mother and baby. Regular screenings and treatments are important.
How to Prepare for Motherhood Before Pregnancy at 1 Week Pregnant?
To prepare for motherhood in the first week of pregnancy, select an OB-GYN, get a preconception checkup, take prenatal vitamins, eat a healthy diet, exercise regularly, gather information about parenting, discuss with your partner, and reduce stress. Below are how to prepare for motherhood before pregnancy.
- Select an OBGYN: Choosing the right obstetrician-gynecologist (OB/GYN) is a critical step in preparing for pregnancy. An OBGYN will guide you through your pregnancy, labor, and delivery. Finding someone you trust and feel comfortable with is essential. Start by researching local providers, requesting recommendations from friends and family, and scheduling consultations to see if the doctor’s approach aligns with your needs and preferences. Check if your health insurance covers the OBGYN.
- Get a Preconception Checkup: Get a thorough preconception checkup with your OBGYN. Your doctor will assess your overall health, review your medical history, screen for specific health conditions, adjust current medications, provide up-to-date vaccines, and address issues that affect pregnancy.
- Take Prenatal Vitamins: Taking prenatal vitamins even before becoming pregnant is essential in building the nutritional foundation for your baby’s development. Folic acid (folate) helps prevent neural tube defects. Essential vitamins and minerals, such as iron, calcium, and vitamin D, support your body in preparing for pregnancy. Your OBGYN will guide you on which prenatal vitamins best suit your needs.
- Eat Healthily: A well-balanced, nutrient-rich diet boosts fertility and prepares your body for pregnancy. Focus on incorporating whole foods, plenty of fruit, vegetables, lean proteins, and whole grains. Limit processed foods, added sugars, and unhealthy fats. Consult a nutritionist to create a meal plan supporting optimal reproductive health.
- Exercise Regularly: Regular physical activity helps your body stay fit and maintain a healthy weight, positively affecting fertility and reducing pregnancy complications. Aim for at least 150 minutes of moderate-intensity weekly exercise, such as walking, swimming, or stretching. If you’re new to exercise, start gradually and consult your healthcare provider for guidance.
- Gather Information: Educate yourself about pregnancy and childbirth. Read books, attend prenatal classes, and explore reputable online resources to familiarize yourself with what to expect during pregnancy and in the early days of motherhood. Knowledge empowers you to make informed decisions and feel more confident in your journey to motherhood.
- Discuss with Partner: Discuss parenthood’s emotional, physical, and financial responsibilities openly. Talk about your goals and expectations and how to support each other through the changes ahead. Ensure you’re on the same page and work together as a team.
- Decide on Your Style of Parenting: Research the different parenting styles. Understand the pros and cons of each parenting style and why the authoritative parenting style is most recommended by psychologists worldwide. Choose and discuss your preferred parenting style with your parenting partner.
- Reduce Stress: Chronic stress interferes with fertility and impacts pregnancy health. Practice stress-reduction techniques like mindfulness, meditation, or deep-breathing exercises.
How Does Stress Management Influence Week One Of Pregnancy?
Stress management influences week one of pregnancy by protecting the delicate balance of hormones necessary for ovulation and implantation and strengthening the immune response. Women with higher perceived stress are associated with reductions in fecundability, according to a 2018 study, “Perceived Stress and Fecundability: A Preconception Cohort Study of North American Couples” by Kenneth J. Rothman, Ann Aschengrau, Amelia K. Wesselink, Lauren A. Wise et al., published in the American Journal of Epidemiology. Chronic stress weakens the immune system, making it harder for the body to fight off infections that interfere with conception or early pregnancy.
How Can a Partner Support the Mother During Week One Of Pregnancy?
Here are 5 ways a partner can support the mother during week one of pregnancy.
- Show Excitement and Optimism: Share in her anticipation and express your enthusiasm about possibly starting a family.
- Make Healthy Lifestyle Changes Together: Support her efforts to eat a balanced diet, exercise together regularly, and manage stress.
- Create a Relaxing Environment: Help her create a peaceful and stress-free environment at home.
- Attend Preconception Appointments Together: If the mother has any checkups or consultations, offer to accompany her.
- Be Intimate and Have Fun: Don’t let the pressure of trying to conceive overshadow the enjoyment of intimacy.
Is it Important to Go to a Doctor for a Preconception Visit?
Yes, it is important to visit a doctor for a preconception visit in week one. Your healthcare provider evaluates your health, medical history, and any existing conditions that affect pregnancy.
During the preconception visit, your OBGYN offers nutritional guidance, recommends prenatal vitamins, and advises on healthy lifestyle habits such as maintaining a healthy weight, exercising, and avoiding smoking, alcohol, and drugs.
Your doctor reviews and adjusts your medications and supplements (prescription and over-the-counter), checks your immunization records, and ensures you are up-to-date on vaccinations like rubella and influenza. If there is a family history of genetic disorders, genetic counseling or testing is usually recommended. The doctor helps identify risks like diabetes, high blood pressure, or thyroid issues, minimizing complications during pregnancy.
For fertility concerns, the doctor discusses potential issues, examines your reproductive health, and recommends further tests or treatments.
The doctor assesses your emotional well-being and offers support if you’re experiencing anxiety or depression related to conception or pregnancy.
This visit helps build a relationship with your healthcare provider. The doctor discusses your plans, helping you prepare mentally and physically for the changes ahead. They provide information on family planning options and help you choose the best method. The doctor suggests a health evaluation for your partner if needed.
What does Parenting Styles Suggest about 1 Week Pregnant?
Parenting Styles has five suggestions for the first week of pregnancy. First, 1 week pregnant is the ideal time to focus on strengthening the bond with your partner. Use the opportunity to reconnect and engage in activities you and your partner enjoy. Pick a shared, relaxing hobby, go on walks, or spend quality time together. Nurture your relationship now creates a solid foundation for the journey ahead. Pregnancy tends to bring emotional and physical challenges. Building a strong connection early on helps ensure you and your partner are better prepared to face these changes as a team.
“Building a strong, supportive relationship with your partner early in pregnancy lays the emotional groundwork for the challenges and joys that come with parenthood,” says Pamela Li, parenting specialist, Founder and Editor-in-Chief of Parenting Styles.
Second, managing stress is crucial when trying to conceive, as high levels of stress negatively impact fertility. Learning stress-management techniques like meditation and yoga improves mental well-being and physical health. Revisiting old hobbies or discovering new ones provides a sense of relaxation and fulfillment. Cultivating stress-relief habits is beneficial throughout your pregnancy, promoting overall well-being for you and your growing baby.
Third, financial preparation ensures a stable future for the parents and the baby. Find out what your pregnancy health insurance coverage is. Create a budget for prenatal care, hospital fees, and the many costs that arise after the baby is born. Saving as early as possible reduces the stress of sudden or unforeseen expenses.
Fourth, Understanding maternity rights at work is essential for stress reduction.
“Knowing your rights regarding maternity leave, pay, and job security provides peace of mind,” Li explains.
Lastly, choose an OB-GYN and schedule a preconception visit. Choose a provider with the medical expertise that makes you feel comfortable and supported. Verify that your health insurance covers the doctor and the hospital. Confirm whether any procedures require prior authorization to avoid last-minute stress.
Congratulations on this exciting journey!