23 Weeks Pregnant Symptoms: Week 23 Of Pregnancy And Prenatal Care
23 weeks pregnant symptoms include increased micturition (urination) frequency and urgency, lower back pain, and pregnancy brain. 23 weeks pregnancy symptoms that start developing this week include pyogenic granuloma (pregnancy tumor). Pyogenic granuloma is a small lump on the gums that grows quickly but goes away on its own after childbirth, according to a 2017 study from Brazil, titled “Systemic alterations and their oral manifestations in pregnant,” conducted by Camilla Silva de Araujo Figueiredo et al. at the Federal University of Maranhao and published in The Journal of Obstetrics and Gynaecology Research.
23 weeks into pregnancy, or 21 weeks after conception, mothers have more energy than in the first trimester. However, in week 23 of pregnancy, expectant mothers start having less quality sleep as stage 3 NREM (non-rapid eye movement) sleep lengthens and interrupted sleep due to nocturnal GERD (gastroesophageal reflux disease) increases.

Your 23-week-old fetus is about the size of a mango and weighs slightly over a pound. You experience increased quickening (fetal movement) that continues to gain strength, frequency, and variation in types of movements, according to a 2017 study from New Zealand, titled “Maternal perception of fetal movements in the third trimester:,” conducted by Billie Bradford et al. at Victoria University of Wellington and published in Women and Birth. The fetus starts to display blinking by opening and closing eyelids at 23 weeks of gestation.
Continuing with regular prenatal care is essential. Attend your scheduled checkups with your OB/GYN (OB-GYN or obstetrician-gynecologist). Be prepared for a glucose screening test between weeks 24- 28 to check for gestational diabetes. These appointments are an opportunity to discuss concerns and learn more about labor and delivery. Maintaining healthy habits is essential; consume a balanced diet of fruits, vegetables, and lean proteins. Stay hydrated, and engage in moderate exercise approved by your OBGYN.
What is 23 weeks pregnant in months? 23 weeks pregnant is 5 months and 3 weeks within the second trimester of pregnancy. You are in the third week in the sixth month of pregnancy.
What are the Pregnancy Symptoms during Week 23?
23 weeks pregnant symptoms include overactive bladder, lower back pain, and pregnancy brain. Here are 21 pregnancy symptoms expecting mothers often experience when 23 weeks pregnant.
- Overactive Bladder (Increased Urination): Overactive bladder syndrome (OAB) is the increased frequency and urgency of micturition (urination), usually with a nocturia (waking up at night to urinate). A 23-week-pregnant mother with OAB often experiences a strong feeling of urgency to empty her bladder and has frequent urination. Urinary incontinence (UI) accompanies OAB in some women and affects their quality of life. Overactive bladder is a urogenital symptom experienced by most mothers during pregnancy. Many women are bothered by this symptom, and the feeling increases with increasing gestational age. Overactive bladders tend to decrease in prevalence rapidly after childbirth.
- Lower Back Pain (Pelvic Girdle Pain or Lumbar Pain): Two types of lower back pain (LBP) are pelvic girdle pain (PGP) and lumbar pain (LP). Pelvic girdle pain is between the posterior iliac crest (the back, top part of your hip bone) and the gluteal fold (the crease where your buttocks meet the back of your thighs). Lumbar pain is over and around the lumbar spine (lower part of your back). Lower back pain is the most common musculoskeletal complaint for 23 weeks of pregnancy symptoms. PGP is approximately four times as prevalent as LP. Pelvic girdle pain is deep, stabbing, unilateral or bilateral, recurrent or continuous. The pain minimizes physical activity and causes some women to withdraw from social interactions. The prevalence of LBP ranges from 25% to 90%. One-third of women suffer from severe pain, and 10% are unable to work due to it. 38% of women still have the symptom at 3 months postpartum.
- Pregnancy Brain (Forgetfulness): 23-week pregnant mothers often have a “baby brain.” Pregnancy brain or baby brain refers to the subjective decline in cognition in up to 81% of pregnant women. Forgetfulness, reading difficulties, confusion, disorientation, poor concentration, increased absent-mindedness, and reduced motor coordination are manifestations of slowed cognition during pregnancy. Forgetfulness has significant real-world consequences, including impaired conversational fluency at work, frequent forgetting of appointments, and difficulties with reading comprehension.
- Fatigue (Tiredness): Fatigue is one of the most common pregnancy symptoms. It appears physically and mentally as a lack of energy, tiredness, and motivation. Antenatal fatigue weakens the cognitive performance and self-care capability of pregnant women. Tiredness reduces muscle endurance, delays healing after physical effort, and decreases the ability to restore sleep. A study showed that more than 96.5% of pregnant women experienced fatigue.
- Insomnia (Difficulty Sleeping): 23 weeks pregnant symptoms include mothers experiencing difficulty sleeping due to insomnia or sleep deficiency. Pregnancy is a period susceptible to chronodisruption. Mothers’ total nighttime sleep falls as stage 3 NREM (non-rapid eye movement) sleep increases. Nocturnal GERD (gastroesophageal reflux disease) causes more awakenings and interrupted sleep. This sleep disturbance persists throughout the pregnancy and lasts through the first 6 months after childbirth.
- Stretch Marks (Striae Gravidarum or SG): Stretch marks are lesions (damaged skin). SG affects up to 90% of women and appears in the second or third trimester. Stretch marks start as pink to violaceous (pink to purple). Stretch marks is sometimes oedematous (swollen) or pruritic (itchy). Stretch marks mature into white, shiny, atrophic, and crinkly streaks.
- Bleeding and Swollen Gum (Pyogenic Granulomas or Pregnancy Tumor): A gingival pyogenic granuloma is a fast-growing inflammatory lump on the gum, sometimes appearing in 23-week pregnant women. The lump usually has a bumpy appearance and ranges in color from pink to red or purple. Pyogenic granulomas vary in size and bleed when touched. it is more common in the anterior (front) and buccal aspect (outer parts) of the maxilla (upper jaw). Bleeding gum, sensitivity, and aesthetic problems are common issues with these pregnancy oral tumors. The lesion tends to regress spontaneously after childbirth.
- Prodromal Labor (Braxton-Hicks Contractions): Braxton-Hicks contractions (pre-labor or false labor) are sporadic contractions and relaxation of the uterine muscle. Some studies found that Braxton-Hicks contractions started around 6 weeks of gestation, while others didn’t begin until the second or third trimester. Braxton-Hicks contractions are the body’s way of preparing for labor, but they are not true labor at 23 weeks pregnant. Braxton-Hicks contractions are a normal part of pregnancy. These prodromal labor contractors are uncomfortable, but they are not painful. Expecting women describe Braxton-Hicks contractions as feeling like mild menstrual cramps or a tightening in the abdomen that comes and goes.
- Increased Appetite: Increased appetite is an increase in food intake, known as hyperphagia, driven by the body’s need to support the growing fetus and prepare for lactation. Hormonal changes, particularly the rise in progesterone, play a significant role in stimulating appetite. Progesterone increases food intake, an essential symptom during pregnancy, to ensure that the mother and the developing baby receive adequate nutrition.
- Food Cravings and Aversion: Cravings typically peak during the second trimester, which includes Week 23. Many pregnant women experience strong urges for specific foods, with common cravings including sweets (like chocolate and candy), savory high-calorie foods (such as pizza and chips), fruits, and dairy products. Conversely, food aversions, often to meat and other high-protein foods, are prevalent and can be a symptom alongside cravings.
- Round Ligament Pain: One cause of abdominal pain in pregnancy is round ligament pain caused by stretching of the round ligament. The pain tends to be localized to the lower abdominal quadrants, radiating to the groin. This cramp-like pain is worse on movement and is more common in multiparous women.
- Leg Cramps: Leg cramping at 23 weeks pregnant is intense, painful muscle contractions that typically affect the calves or feet and often occur at night, disrupting sleep. Leg cramps at night sometimes lead to daytime fatigue and poor concentration. Cramping at 23 weeks pregnant is prevalent, with up to 30% of mothers experiencing leg cramps.
- Constipation: Constipation is when you have infrequent bowel movements (fewer than three times a week). The stools are hard and painful to pass with a sensation of straining or incomplete evacuation. Severe constipation leads to more serious issues like fecal impaction or rectal bleeding. Constipation occurs because rising progesterone levels slow down gut motility. The muscles in the intestines move waste slowly. Increased water absorption from the gut leads to reduced bowel movements. Constipation affects up to 38% of pregnant women and is common during 23 weeks of pregnancy.
- Heartburn (Gastro-Esophageal Reflux): Heartburn is a burning sensation in the chest or throat. Heartburn occurs when acid flows back into the esophagus. The baby’s growing size pressures the stomach, causing acid to flow back and escape. Heartburn typically starts in the first trimester and becomes more frequent and severe in the 2nd and 3rd trimester. 23-week pregnant mothers are in their second trimester.
- Piles (Hemorrhoids): Piles are swollen veins located around or inside the rectum and anus. Hemorrhoids cause bleeding, pain and discomfort, itching and irritation, prolapse, and mucous discharge during the second and third trimesters. Hemorrhoid symptoms are related to increased abdominal pressure from the growing uterus and constipation.
- Headaches: Headaches cause discomfort and pain in the head, neck, or scalp and indicate serious conditions in pregnancy when sudden and severe. Preeclampsia (a pre-convulsive condition characterized by hypertension) typically presents with headaches after the 20th week of pregnancy, including the 23rd week of pregnancy symptoms. However, headache patterns usually improve later in pregnancy.
- Vision Changes: Vision changes during pregnancy, such as blurred, distant vision, occur due to a myopic shift (increased nearsightedness) caused by hormonal changes that alter the cornea’s shape and thickness. Around 54% of women experience reduced distance vision in the second trimester, and 23-week pregnant mothers are in the second trimester.
- Breast Changes: The breasts swell and become tender due to increased glandular and fat tissue in preparation for lactation. At 23 weeks, your breasts likely feel fuller, often leaking colostrum before full milk production begins. Blood flow to the mammary glands increases significantly at this stage, doubling pre-pregnancy levels by week 24.
- Edema (Swollen Ankles and Feet): Edema, also known as fluid retention, typically affects the lower extremities in pregnancy, causing swelling and discomfort. Edema occurs when the growing uterus pressures blood vessels, hindering blood return from the legs to the heart. About 87% of pregnant women experienced swollen ankles and feet, and around 44% noticed an increase in shoe size by the third trimester due to this swelling.
- Drop in Blood Pressure and Anemia: Hormones like progesterone, nitric oxide, and prostaglandins cause blood vessels to relax and dilate during pregnancy, causing a natural drop in blood pressure. Blood pressure levels drop to their lowest between 20 and 24 weeks, often resulting in hypotension as pregnancy symptoms in week 23. Physiologic anemia of pregnancy develops when plasma volume increases to surpass the red blood cell (RBC) mass in the blood. Anemia results in a lower concentration of hemoglobin and thinner blood.
- Hot Flashes: Hot flashes are sudden, uncomfortable sweating episodes and feeling very warm. Hormonal fluctuations typically cause hot flashes within the first few weeks of pregnancy, similar to those experienced during menopause. Approximately 62% of pregnant mothers reported mild, weekly hot flashes.
Here are the studies and research on common week 23 pregnancy symptoms.
| Week 23 Pregnancy Symptoms | Description | Studies |
|---|---|---|
| Overactive Bladder (Increased Urination) | Overactive bladder syndrome (OAB) is a common urogenital issue during pregnancy, marked by frequent, urgent urination and often accompanied by urinary incontinence, which typically improves after childbirth. | According to a 2006 study from The Netherlands, titled “How Do the Prevalences of Urogenital Symptoms Change During Pregnancy?,” by H. Jorien van Brummen et al, published in Neurourology and Urodynamics: Official Journal of the International Continence Society. |
| Lower Back Pain (Pelvic Girdle Pain or Lumbar Pain) | Lower back pain during pregnancy often manifests as pelvic girdle pain (PGP) or lumbar pain (LP), with PGP being more common, characterized by deep, stabbing discomfort that can limit physical activity and social interaction. | According to a 2011 study from Greece, titled “Pregnancy-related low back pain,” conducted by Kalliopi Alpantaki et al. at the University of Crete and published in Hippokratia. |
| Pregnancy Brain (Forgetfulness) | Many 23 weeks pregnant women experience “baby brain,” a common condition affecting up to 81% of expectant mothers. Forgetfulness, confusion, and poor concentration can impact daily tasks and work performance. | According to a 2018 study from Australia, titled “Cognitive impairment during pregnancy: a meta-analysis,” conducted by Helen Skouteris et al. at Deakin University and published in the Medical Journal of Australia (MJA). According to a 2016 study titled “Insomnia during Pregnancy:Diagnosis and Rational Interventions,” by Imran S. Khawaja. et al., published in Pak J Med Sci. |
| Fatigue (Tiredness) | Fatigue causes physical and mental exhaustion, reducing energy and motivation. It impairs cognitive performance, self-care, muscle endurance, and sleep restoration and affects over 96.5% of pregnant women. | According to a 2017 study from The United States, titled “Fatigue in Pregnancy,” conducted by Kwaghdoo Atsor Bossuah at Tennessee State University and published in the International Journal of Childbirth Education. |
| Insomnia (Difficulty Sleeping) | Insomnia causes difficulty sleeping and disrupts nighttime rest. Difficulty sleeping is linked to nocturnal GERD throughout pregnancy and continues for up to six months after childbirth. | According to a 2016 study titled “Insomnia during Pregnancy:Diagnosis and Rational Interventions,” by Imran S. Khawaja. et al., published in Pak J Med Sci. |
| Stretch Marks (Striae Gravidarum or SG) | Stretch marks affect up to 90% of women during the second or third trimester. These skin lesions begin as pink to purple marks, then mature into white, shiny, crinkly streaks that may be swollen or itchy. | According to a 2015 study from The United States, titled “Stretch marks during pregnancy: a review of topical prevention,” conducted by Frank Wang et al. at the University of Michigan and published in the British Journal of Dermatology. |
| Bleeding and Swollen Gum (Pyogenic Granulomas or Pregnancy Tumor) | A gingival pyogenic granuloma is a fast-growing, pink to purple lump on the gum. These lesions bleed easily and cause gum sensitivity. Bleeding and swollen gum often regresses after childbirth. | According to a 2016 study from China, titled “Initial periodontal therapy for the treatment of gingival pregnancy tumor,” conducted by C.Z. Li et al. at Wuhan University and published in Genetics and Molecular Research. |
| Prodromal Labor (Braxton-Hicks Contractions) | Braxton-Hicks contractions, or false labor, are sporadic uterine contractions that start as early as six weeks and are prevalent in the second or third trimester. These contractions are mildly uncomfortable and not true labor. | According to a 2020 study from Portugal, titled “Uterine contractions clustering based on electrohysterography,” conducted by Filipa Esgalhado et al. at NOVA University Lisbon and published in Computers in Biology and Medicine. |
| Increased Appetite | Appetite increases due to the body’s growing nutritional needs. | According to a 2021 study from USA, titled “The Importance of Nutrition in Pregnancy and Lactation: Lifelong Consequences,” by Nicole E. Marshall et al., published in The American Journal of Obstetrics and Gynecology. |
| Food Cravings and Aversion | Food cravings often peak around Week 23, including sweets, savory foods, fruits, and dairy. Many women also experience food aversions, especially to meat and other high-protein foods. | According to a 2014 study from The United States, titled “Pickles and ice cream! Food cravings in pregnancy: hypotheses, preliminary evidence, and directions for future research,” conducted by Natalia C. Orloff et al. at University at Albany – State University of New York and published in Frontiers in Psychology. |
| Round Ligament Pain | Round ligament pain causes abdominal discomfort from stretching ligaments. Usually felt in the lower abdomen and groin, it intensifies with movement and is more frequent with multiple pregnancies. | According to a 2017 study from Japan titled “Round ligament varicosities diagnosed as inguinal hernia during pregnancy: A case report and series from two regional hospitals in Japan,” by Yuka Mine et al., published in the International Journal of Surgery Case Reports. |
| Leg Cramps | Up to 30% of mothers experience leg cramps at 23 weeks. | According to a 2009 study from The United States, titled “Leg Cramps and Restless Legs Syndrome During Pregnancy,” conducted by Jennifer G. Hensley at the University of Colorado Denver and published in The Journal of Midwifery & Women’s Health. |
| Constipation | Constipation, which affects up to 38% of women at 23 weeks, involves infrequent, hard, and painful bowel movements. Severe cases can cause fecal impaction or rectal bleeding. | According to a 2015 study from the UK, titled “Constipation in Pregnancy,” by Pallavi Latthe et al., published in Constipation in Pregnancy. The Obstetrician & Gynaecologist. |
| Heartburn (Gastro-Esophageal Reflux) | Heartburn is a burning sensation in the chest or throat when stomach acid flows back into the esophagus, often worsening in the second and third trimesters. | According to a 2014 study from Turkey, titled “Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women,” by Gulsen Eryilmaz et al., published in the Journal of Clinical Nursing. |
| Piles (Hemorrhoids) | Piles are swollen veins in the rectum and anus that cause bleeding, pain, and itching. | According to a 2014 study from The United States, titled “Physiologic and pharmacokinetic changes in pregnancy,” conducted by Maged M. Constantine at the University of Texas Medical Branch and published in Frontiers in Pharmacology. |
| Headaches | Headaches can signal serious conditions like preeclampsia after the 20th week but often improve later in pregnancy. | According to a 2017 study from Italy, titled “Headache and pregnancy: a systematic,” conducted by Andre Negro et al. at Sant’Andrea Hospital and published in The Journal of Headache and Pain. |
| Vision Changes | Vision changes, like blurred distance vision, result from hormonal shifts that alter the cornea’s shape and thickness. 54% of women experience this in the second trimester. | According to a 2014 study from Iran, titled “Visual Acuity Changes during Pregnancy and Postpartum: A Cross-Sectional Study in Iran,” by Abolfazl Mehdizadehkashi et al., published in Journal of Pregnancy. |
| Breast Changes | Swelling, tenderness, fullness, and colostrum leakage occur due to increased glandular tissue and blood flow in preparation for lactation. | According to a 2014 study from The United States, titled “Physiologic and pharmacokinetic changes in pregnancy,” conducted by Maged M. Constantine at the University of Texas Medical Branch and published in Frontiers in Pharmacology. According to a 2009 study from Australia, titled “Ultrasound imaging of the lactating breast: methodology and application,” conducted by Donna T. Geddes at The University of Western Australia and published in the International Breastfeeding Journal. |
| Edema (Swollen Ankles and Feet) | Edema, or fluid retention, causes swelling in the ankles and feet, affecting about 87% of pregnant women. | According to a 2010 study from The United States, titled “Lower Extremity Changes Experienced During Pregnancy,” conducted by Priya Ponnapula et al. at SSM DePaul Health Center, Bridgeton, MO and published in The Journal of Foot and Ankle Surgery. |
| Drop in Blood Pressure and Anemia | Blood vessels relax during pregnancy, causing a drop in blood pressure (lowest between 20 and 24 weeks), and plasma volume increases faster than red blood cell mass, causing physiologic anemia. | According to a 2014 study from The United States, titled “Physiologic and pharmacokinetic changes in pregnancy,” conducted by Maged M. Constantine at University of Texas Medical Branch and published in Frontiers in Pharmacology. |
| Hot Flashes | Hot flashes, characterized by sudden warmth and sweating, are caused by hormonal fluctuations. About 62% of pregnant women experience mild, weekly hot flashes. | According to a 2005 study from The United States, titled “Hot flashes during pregnancy: a comparative study,” conducted by James C. Coyne et al. at the University of Pennsylvania and published in the European Journal of Obstetrics & Gynecology and Reproductive Biology. |

What is the Importance of Understanding Being 23 Weeks Pregnant?
The importance of understanding being 23 weeks pregnant is being prepared for more pregnancy symptoms.
Common 23-week symptoms include overactive bladder, lower back pain, pregnancy brain (forgetfulness), and fatigue. The expanding uterus places pressure on the bladder, leading to frequent urination, while hormonal changes contribute to cognitive challenges like forgetfulness. Lower back pain, which affects many pregnant women, arises due to the strain on the spine and pelvis as the body adapts to the growing baby.
Increased appetite, food cravings, round ligament pain, leg cramps, and insomnia are also typical at this stage. The mother’s body requires more nutrients, leading to heightened hunger, while hormonal shifts cause cravings and aversions. Round ligament pain occurs as the ligaments supporting the uterus stretch, while leg cramps, often disrupting sleep, are linked to circulation and muscle strain changes.
Understanding pregnancy week by week allows expectant mothers to seek proper care and adopt coping strategies that enhance their comfort and well-being. Awareness of the fetus’s growth and development—such as the formation of fingerprints, ongoing brain development, and lung maturation—helps parents connect with their baby and track essential milestones.
What to Expect at 23 Weeks Pregnant?
23 weeks pregnant mothers should expect overactive bladder, lower back pain, and pregnancy brain. Other common second-trimester symptoms include insomnia, stretch marks (striae gravidarum or SG), bleeding gum, Braxton-Hicks contractions, increased appetite, and food cravings.
23-week baby reaches several key developmental milestones. The baby’s skin becomes plumper as fat deposits stabilize, providing insulation and energy. Unique fingerprints and footprints form as tissue differentiation occurs, setting the baby apart as an individual. The brain continues its rapid growth, with measurable increases in key dimensions, reflecting ongoing development.
Facial features, such as the eyes, nose, and mouth, are becoming more defined, and fine motor skills are improving as the baby makes more intentional movements, like touching their face. Hair follicles and sweat glands are maturing, helping with postnatal functions like temperature regulation. The skin also undergoes keratinization, making it more resilient.
Around this time, your baby’s hearing and light sensitivity are progressing. They may startle at loud noises and react to light shining through the womb. The lungs form crucial structures for gas exchange, preparing for the first breaths after birth. Breathing-like movements are also seen in preparation for life outside the womb, and the baby shows distinct rest and wake cycles, including REM sleep, indicating brain activity related to dreaming.
By week 23, your baby’s pancreas matures to produce insulin, vital for regulating blood sugar. The baby is also developing a sense of touch, aided by the maturation of neural pathways in the brain. These sensory and physiological developments mark significant milestones in preparing the baby for life after birth.

How is the Baby Developing at 23 Weeks Pregnant?
Your 23-week baby is approximately the size of a mango, weighing around 565 grams (1.25 pounds). Growth is now measured using key dimensions such as the biparietal diameter (57 mm), head circumference (210 mm), abdominal circumference (185 mm), and femur and humerus lengths (41 mm each). These precise measurements reflect the baby’s development across different body areas.
Key week 23 developmental milestones are rapidly taking place. Fingerprints and footprints have formed, and the baby’s skin becomes plumper as fat deposits stabilize, providing energy storage and insulation. The baby’s brain and facial features continue to develop, with more distinct facial structures emerging, often visible on 3D ultrasounds.
Hair follicles and sweat glands are maturing, and keratinization is progressing, making the skin more resilient and less transparent. The baby is also becoming more responsive to sensory stimuli. Hearing develops, and the baby might react to loud sounds while the eyes begin showing sensitivity to light. Fine motor skills improve as the baby’s movements become more intentional, like reaching toward their face.
The lungs are in a crucial stage of development, forming structures necessary for gas exchange and preparing for life outside the womb. Meanwhile, the pancreas continues maturing, developing the ability to produce insulin, which is vital for regulating growth. Overall, week 23 marks a period of significant physical and neurological growth as your baby becomes more active and responsive.
How Big is Your Baby at Week 23 of Pregnancy?
Your 23-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 23-week-old fetus is about the size of a mango. The 50th percentile measurements for 23-week fetal growth are as follows: the biparietal diameter (BPD) is 57 millimeters, the head circumference (HC) is 210 millimeters, the abdominal circumference (AC) is 185 millimeters, the femur length (FL) is 41 millimeters, and the humerus length (HL) is 38 millimeters.
The 23-week-old fetus weighs 565 grams (19.93 ounces or 1.25 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
What are the Key Developmental Milestones of Babies at Week 23 of Pregnancy?
Week 23 of pregnancy shows the following 19 key developmental milestones in the babies.
- Fingerprints and Footprints: Between weeks 21-24 of pregnancy, unique ridges and valleys form on the tips of the fingers and feet. Tissue differentiation causes the formation of these fingerprints and footprints when cells (including skin cells) specialize into specific types.
- Fingerprints Develop: Fingerprints are unique patterns on the tips of the fingers, which start forming around week 13 of pregnancy. Primary ridges develop on your baby’s palms and soles by week 17, and secondary ridges begin to form between them, shaping the overall fingerprint pattern.
- Plump Skin: The first fat deposits start to form at week 14 of pregnancy, primarily in the cheeks, contributing to your baby’s plump skin. These fat deposits stabilize by week 23, providing insulation and energy storage for the fetus. Between weeks 23 and 29, adipose (fat) tissue grows as fat lobules enlarge and develop adipocytes and a supporting capillary network.
- Brain Development: The fetus’ brain structures continue to grow, and specific measurements are used to assess this development, including the front-occipital diameter (FOD), cerebral biparietal diameter (CBD), and transverse cerebellar diameter (TCD). At 23 weeks, the expected values indicating normal brain development are FOD at 64 mm, CBD at 46 mm, and TCD at 25 mm.
- Facial Features: Your baby’s facial features become more distinct and recognizable. Between weeks 23 and 30 of pregnancy, 3D ultrasound scans often reveal the developing fetal facial structure, including the nasal bridge, mouth, eyelids, and even subtle facial expressions.
- Hair Follicle and Sweat Gland Development: The skin and hair structures essential for postnatal functions like temperature regulation and external protection are maturing by week 23 of pregnancy. Hair follicles form as epidermal buds at 14 weeks and continue to elongate at 23 weeks. Eccrine sweat glands, which start developing at 20 weeks, elongate and coil during this period.
- Skin Keratinization: Your baby’s skin starts producing keratin, a protein that forms a protective barrier between 20-25 weeks of gestation. This process, known as keratinization, causes the skin to become less transparent and blood vessels to become more visible. Before keratinization, the fetal skin is vulnerable to environmental influences, like substances in the amniotic fluid, but it becomes more resilient and less porous as keratin develops.
- Hearing: Your baby begins to show a startle response to sound, indicating the development of the auditory system. This early responsiveness suggests that babies start forming memory traces from sounds in the womb, with the developing brain processing external sounds like the mother’s voice or music.
- Light Sensitivity: Your baby’s eyes and neurological system become more responsive to light. Shining a bright light on the mother’s abdomen causes increased fetal movement or changes in heart rate, reflecting the ongoing development of the visual system and neural responses to external stimuli.
- Fine Motor Skills: Fine motor skills involve the precise coordination of small muscles in the hands and fingers. Fetal movements become more intentional, and your baby reaches toward sensitive areas like the mouth, hands, and face. Fine motor skills develop around week 23 as the fetus engages in spontaneous movements (motor babbling), helping it explore its body and surroundings and laying the foundation for advanced skills like grasping after birth.
- Lung Structure for Gaseous Exchange: The basic structures for gas exchange are formed and vascularized in the fetal lung between the 16th and 28th weeks of pregnancy. Your 23-week fetus is in this stage, where the airways widen, the cell lining thins and capillaries move closer to the airways. Primitive respiratory bronchioles develop in the gas-exchanging region called the acinus, and the acinar epithelium begins differentiating into type II pneumocytes, which produce lung surfactant.
- Lung Maturation: The peripheral airways grow and mature into fully developed respiratory airways between weeks 16-27 of pregnancy, with the adult form of the lung emerging by week 24. Epithelial cells differentiate into two types of alveolar cells, including those responsible for producing lung surfactant, while the capillary network continues to develop. The blood-gas barrier is as thin as in an adult lung by week 27 and provides sufficient surface area for adequate gas exchange, which is crucial for survival after birth.
- Pancreas Development: The fetal pancreas is maturing to supply insulin, with insulin-producing beta cells developing as early as 19 weeks of pregnancy. Insulin helps regulate blood sugar levels and support growth. Poor maternal health, such as severe diabetes or malnutrition, sometimes leads to impaired development of the fetal pancreas and reduced insulin production later in life.
- Rapid Eye Movement: Week 23 is the onset of REM (rapid eye movement), which is more frequent and drawn out in the following weeks. REM is typically observed during dream sleep stages in humans. Advanced ultrasound imaging detects REM as quick, simultaneous movements of both eyes, contrasting to the slower eye movements seen earlier in fetal development.
- Sense of Touch: Thalamocortical pathways reach the maturing somatosensory cortex, where touch sensations are processed. This aids in developing your baby’s sense of touch and ability to perceive tactile stimuli, including pain.
- Breathing Movements: Fetal breathing movements are episodic and primarily occur during REM sleep. Breathing in fetuses involves short, rapid diaphragm bursts and intercostal muscle activity. Breathing movements are detectable on ultrasound as early as week 13. The 23-week fetus continues to practice breathing and strengthen respiratory muscles in preparation for life outside the womb.
- Rest/Wake Cycles: Your baby exhibits more distinct rest (quiescence) and active (awake) periods, which become more synchronized and refined as pregnancy progresses. Rest/wake cycles in the fetus are connected to autonomic nervous system development, which controls functions like heart rate and digestion.
- Blinking: Your baby begins to blink, opening and closing its eyelids independently and responding to light between weeks 23 and 26 of pregnancy. This early blinking action shows the fetus’s maturing sensory and nervous systems.
- Breathing movements: Rhythmic contractions of the diaphragm that mimic breathing are observed in the fetus, becoming more pronounced as your baby prepares for life outside the womb. Nasal fluid flow velocity waveforms (NFFVWs), which reflect fluid movement through the fetal nose and indicate breathing-like activities, are detected by week 22. Abdominal wall movements associated with fetal breathing are observed in about 61% of fetuses between weeks 21 and 25.

How to Know if Your Baby is Healthy during Week 23 of Pregnancy?
- Keep Track of Movement: Monitoring fetal movement is one of the oldest methods to assess your baby’s health. 23-week pregnant women are encouraged to keep track of their baby’s daily activity by counting movements or being alert to changes. Although babies exhibit varying movement patterns, regular fetal movements generally indicate a healthy baby, while decreased fetal movement (DFM) is linked to stillbirth or fetal growth restriction.
- Perform Ultrasound Test: An ultrasound uses high-frequency sound waves to assess fetal growth and anatomy by providing a clear view of your baby in the womb. A second-trimester ultrasound offers reassurance about your baby’s health and helps identify multiple pregnancies or fetal abnormalities, allowing for timely intervention if needed.
- Listen for Fetal Heartbeat: A regular fetal heart rate typically ranges from 120 to 160 beats per minute. A regular heartbeat observed during an ultrasound scan at 23 weeks indicates a healthy fetus.
- Measure Amniotic Fluid Levels: Decreased amniotic fluid (oligohydramnios) can signal issues like kidney problems, while excess fluid (polyhydramnios) may be linked to conditions like diabetes or fetal obstruction. Amniotic fluid levels usually stabilize at week 23. Ultrasound is a noninvasive method used to measure and monitor these fluid levels, helping to detect and manage potential complications.
- Report Suspicious Complication Symptoms: Pregnant women with complications like ectopic pregnancies may not show symptoms like abdominal pain, vaginal bleeding, or decreased fetal movement until later stages. Mothers must be vigilant in reporting suspicious symptoms, even if unsure.
Can You Hear Your Baby’s Heartbeat through a Stethoscope at 23 Weeks Pregnant?
Yes, you can hear your baby’s heartbeat through a stethoscope at 23 weeks pregnant in some women. The baby’s heartbeat is strong enough to be detected with a stethoscope by weeks 17-20 of pregnancy, according to a 2021 study from India, titled “Advantages of Screening for Glucose Tolerance in the Sequential Weeks of Gestation,” by N. Bhavatharani et al., published in Journal of Social Health and Diabetes.
What Are The Changes In The Mother’s Body At 23 Weeks Pregnant?
- Swollen Ankles: As pregnancy progresses, increased levels of estrogen and relaxin cause blood vessels to dilate, leading to swelling (edema) in the feet and ankles. Over 80% of women report swollen ankles and feet during pregnancy, often resulting in larger shoe sizes as term approaches, according to a 2010 study titled “Lower Extremity Changes Experienced During Pregnancy.”
- Varicose Veins: Varicose veins are visibly swollen, twisted veins that cause aching or burning sensations in the legs. Varicose veins of the lower extremities (VVLE) develop as blood volume and pressure in the veins increase due to the expanding uterus. VVLE in pregnancy typically begins to appear in the second trimester, peaking between weeks 19 and 24—right where you are at 23 weeks pregnant, according to a 2010 study, “Varicose Veins of Lower Extremities in Pregnant Women and Birth Outcomes”.
- Breast Changes: As your body prepares for lactation at 23 weeks pregnant, the glandular tissue in the breasts, responsible for milk production, increases. The total blood flow to the breasts rises and will double pre-pregnancy levels by week 24, according to a 2009 study, “Ultrasound imaging of the lactating breast: methodology and application“. This increased blood flow supports tissue formation and the development of milk ducts, preparing your body for breastfeeding.
- Uterus Size / Abdominal Growth: At 23 weeks, the mother’s uterus is undergoing significant growth to accommodate the rapidly developing fetus. Between weeks 20 and 32, the uterus elongates, and its walls thin to make room for the growing baby. While each pregnancy is unique, the uterus can increase in weight from 70 grams to between 1,000 and 1,100 grams and expand in volume from 10 mL to about 5 liters during pregnancy.
- Weight Gain: Weight gain is a natural and essential part of pregnancy as your baby grows and your body stores more water for circulation, amniotic fluid, and the placenta. The weight gained varies depending on your pre-pregnancy BMI (body mass index). For a mother with an average pre-pregnancy weight (BMI 18.5-24.9), typical weight gain throughout pregnancy ranges from 11.5 to 16 kg. However, sudden weight gain exceeding 0.5 kg per week may indicate potential health concerns and should be monitored closely.
- Braxton Hicks Contractions: Braxton Hicks contractions are irregular and unpredictable false labor pains that help prepare the mother’s body for true labor. These contractions often resemble mild menstrual cramps or a tightening sensation in the abdomen. Braxton Hicks contractions usually start at week 6 and continue at 23 weeks pregnant, preparing the body for true labor pains.
- Linea Nigra: Linea nigra is a dark vertical line that appears on the abdomen as a result of hyperpigmentation, usually running from the pubic bone to the belly button and sometimes extending up to the chest. This skin change typically occurs in the second trimester and is triggered by increased levels of hormones like estrogen and progesterone, which stimulate melanin production. Linea nigra is a normal, temporary change that fades postpartum.
- Increased Heart Rate: By the end of the first month of pregnancy, the mother’s heart rate grows, with maximum cardiac output reached by week 24. At 23 weeks pregnant, that’s just one week away. By week 28, your heart rate rises by approximately 10 to 15 beats per minute to help support the higher blood volume and cardiac output needed during pregnancy. This increased heart rate typically plateaus between weeks 28 and 32.
- Maternal Circadian Rhythm: The circadian rhythm is the body’s internal clock that follows a roughly 24-hour cycle. Hormones like melatonin, which peaks at night, and cortisol, which peaks in the early morning, help synchronize the body’s systems. Disruptions in these rhythms during pregnancy, even as early as 23 weeks, can lead to complications such as preterm birth and low birth weight.
How Big is a 23-Week Pregnant Belly?
A 23-week pregnant belly has a fundal height of around 23 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 23-week-pregnant belly measures around 23 centimeters, between 21 to 25 centimeters. The expanding uterus grows to accommodate the growing fetus. The 23-week pregnant uterus has grown enough to be palpated above the navel level.
The uterine size and its growth rate are affected by several factors, such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than those with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. However, the 2016 World Health Organization (WHO) ANC Guidelines concluded that there was inadequate evidence of using the SFH to predict fetal health.
Can You Feel Contractions as Early as 23 Weeks Pregnant?
Yes, you can feel contractions as early as 23 weeks pregnant, known as “Braxton-Hicks contractions.” Unlike true labor contractions, Braxton-Hicks contractions are less localized and tend to spread across more expansive uterus areas as delivery approaches, preparing your body for labor. These contractions vary with each pregnancy, occurring from once an hour to every 3-4 hours. Braxton-Hicks at 23 weeks pregnant is entirely normal since these contractions typically begin around the 20th week of gestation, becoming more frequent and stronger as you near term.
Talk to your OBGYN if you experience pains that aren’t related to Braxton-Hicks at 23 weeks, such as intense abdominal pain that does not go away, upper abdominal pain (especially under the ribs on the right side), or burning urination with abdominal pain, according to a 2023 study, “Braxton Hicks Contractions”.

Is Skin Discoloration Common at 23 Weeks Pregnant?
Yes, skin discoloration (maternal hyperpigmentation) is common at 23 weeks pregnant. Hyperpigmentation is observed in 70% of pregnant women during the second trimester, according to a 2014 study from Turkey, titled “The physiological changes in pregnancy and their distribution according to trimester,” conducted by Ayse Neslin Akkoca et al. at the University Faculty of Medicine and Research Hospital and published in Journal of Gynecology and Obstetrics. You are in the second trimester at 23 weeks.
Skin Discoloration occurs due to increased levels of estrogen and progesterone, which stimulate the skin to produce more pigment. Hyperpigmentation in pregnancy typically includes darkening of areas such as the areola, navel, and genitals, as well as the appearance of the “linea nigra,” a dark line that runs down the center of the belly.
Why Does UTI Occur More Often At Week 23 Of Pregnancy?
Urinary tract infections (UTIs) occur more often at week 23 of pregnancy due to fluctuating hormone levels, ureteral dilation, increased plasma level, vaginal pH level, and uterine growth.
Estrogen helps maintain a healthy level of protective bacteria in the vagina, such as Lactobacillus, which prevents the colonization of harmful bacteria and infection. This was highlighted in a 2016 study titled “The Vaginal Microbiota and Urinary Tract Infection.” However, fluctuating hormone levels during pregnancy sometimes cause temporary estrogen depletion, increasing the risk of UTI-causing bacteria moving into the urinary tract. Additionally, increased levels of progesterone and estrogen during pregnancy reduce muscle tone of the ureters and bladder, leading to conditions like urinary stasis and ureteric reflux, which promote bacterial growth and increase the risk of infections like UTIs, according to a 2011 study, “Prevalence Of Urinary Tract Infection During Pregnancy”.
Around the 6th week of pregnancy, progesterone causes the ureters (tubes that carry urine from the kidneys to the bladder) to relax and dilate, which peaks between weeks 22 and 26 of pregnancy, according to a 2018 study titled “Urinary Tract Infection During Pregnancy: Current Concepts on a Common Multifaceted Problem.” As the uterus grows, it places pressure on the ureters, causing hydronephrosis, a condition where the kidneys swell due to urine buildup. This urine buildup slows the flow of urine, leading to urinary stasis, where urine remains in the urinary tract for extended periods, creating an environment that promotes bacterial growth.
Increased blood plasma volume in pregnant women leads to more diluted urine and a larger bladder volume. This dilution decreases the concentration of urinary antibacterial substances, reducing urine’s effectiveness in fighting infections. Additionally, pregnancy alters urine pH, leading to glucose and amino acids in urine, which provide nutrients for bacteria and promote their growth.
The growing uterus places pressure on the bladder and urinary tract, which increases the likelihood of urinary stasis. This, in turn, promotes bacterial growth and raises the risk of developing a UTI during the second trimester.
Why is Your Skin More Sensitive at 23 Weeks Pregnant?
Your skin is more sensitive at 23 weeks pregnant due to hormonal changes, stretching skin, and increased maternal blood flow.
Elevated hormone levels, particularly progesterone and estrogen, stimulate melanocytes (the cells responsible for skin pigmentation), leading to changes in skin color and increased sensitivity to touch or friction. Estrogen and progesterone boost oil production, making some women’s skin more sensitive and prone to acne.
As the baby grows, physical stretching of the mother’s skin causes stretch marks to form, often beginning around week 23 of pregnancy. This stretching can lead to irritation and itching in areas like the scalp, abdomen, and genitals.
Increased maternal blood flow typical of pregnancy often leads to vascular skin changes and sensitivities, such as the development of spider veins and reddened palms.
What are the Tips for Prenatal Care during Week 23?
- Take Prenatal Vitamins: Taking prenatal vitamins during week 23 and throughout your pregnancy provides you and your baby with the necessary nourishment for healthy growth. Essential nutrients include folic acid, iron, calcium, vitamin D, choline, omega-3 fatty acids, and B vitamins. Folic acid prevents birth defects in the baby’s brain and spine, while iron supports blood production.
- Track Fetal Movement: Maternal perception of fetal movements remains the oldest and most common method for assessing fetal well-being. A noticeable decrease in fetal movements sometimes indicates complications, such as stillbirth or fetal growth restriction. At 23 weeks pregnant, it’s essential to remain attentive to your baby’s daily activity and promptly alert your OBGYN if you notice any drastic changes in movement.
- Maintain a Healthy Diet and Lifestyle: Pregnant women should eat a varied diet that includes all food groups to support their health and their baby, adding two to three extra servings to their daily intake. Taking a daily prenatal multivitamin containing folic acid and iron is essential. Regular physical activity, such as prenatal yoga, walking, and swimming, helps manage pregnancy-related discomforts.
- Engage in Physical Activity: Physical activity (PA) positively impacts physical and psychological well-being during the second and third trimesters, according to a study published in the International Journal of Environmental Research and Public Health. Activities like brisk walking or prenatal yoga improve overall health, boost energy levels, and enhance mood. A routine, including regular physical activity, helps to reduce common pregnancy discomforts for a more enjoyable pregnancy experience by week 23.
- Stay Engaged with Your Healthcare Provider: Regular consultations with your OB-GYN ensure consistent maternal and fetal health monitoring through tailored advice and prenatal screening.
- Prepare for Parenting: As a couple, it’s important to seek realistic information on parenting skills and attend antenatal classes focusing on infant care, breastfeeding, and the roles and responsibilities of new parents. Educate yourselves about managing relationship changes and adjusting to new responsibilities together to help ease your transition into parenthood.
- Practice Relaxation Techniques: Techniques like mindfulness lower maternal heart rate, blood pressure, and stress hormones, improving emotional health during pregnancy. Maternal relaxation practices have been shown to reduce fetal heart rate and motor activity, contributing to a calmer in-utero environment.
- Prepare for Labor and Delivery: Active participation in antenatal education classes as part of prenatal care provides realistic insights into parenting. Both parents should have access to information on newborn care and resources to help navigate the changes ahead. Maintain open communication and rely on support systems as you prepare for the journey ahead.
What Types of Foods are Beneficial to Eat during Week 23 of Pregnancy?
Foods that are beneficial to eat during week 23 of pregnancy include foods rich in folic acid, calcium, iron, iodine, choline, vitamin A, vitamin C, vitamin D, vitamin B6, Vitamin B12, and the 5 food groups.
Folic acid: Helps prevent birth defects and supports overall fetal development. Incorporate dark green leafy vegetables, fortified cereal, and orange juice into your diet.
Calcium: Supports bone and teeth development. Try including yogurt, sardines, and dark green leafy vegetables.
Iron: Helps make red blood cells that deliver oxygen to your baby. Add lean red meat, dried beans and peas, and prune juice to your meals.
Iodine: Essential for your baby’s brain development. Incorporate iodized table salt, seafood, and eggs into your diet.
Choline: Important for your baby’s brain and spinal cord development. Enjoy peanuts, beef liver, and soy products for a choline boost.
Vitamin A: Assists in red blood cell formation. Foods like carrots, green leafy vegetables, and sweet potatoes are good choices.
Vitamin C: Promotes healthy gums, teeth, and bones. Include strawberries, tomatoes, and broccoli in your meals.
Vitamin D: Supports bone health and eyesight. Opt for sunlight, fortified milk, and fatty fish like salmon.
Vitamin B6: Helps in red blood cell production and nutrient utilization. Try whole-grain cereals, bananas, and pork.
Vitamin B12: Important for nervous system function and red blood cell formation. Eat poultry, milk, and fish for your B12 needs.
Grains: Include quinoa, brown rice, and oats for plenty of fiber and B vitamins.
Fruits: Choose fresh, frozen, or dried fruit, with whole fruit better than juice.
Vegetables: Add raw, frozen, or dried vegetables for essential nutrients like calcium and protein.
Protein: Include seafood, beans, and eggs to ensure you get enough protein, iron, and omega-3s.
Dairy: Consume pasteurized milk, cheese, and yogurt for calcium and vitamin D.
These food options will help ensure you and your baby receive the necessary nutrients during week 23 of pregnancy.
What Exercises Can You Do during Week 23 of Pregnancy?
The 6 recommended moderate-intensity aerobic and muscle-strengthening activities for week 23 of pregnancy are based on the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour.
| Week 23 of Pregnancy Exercise | Description |
|---|---|
| Walking | Low-impact exercise that supports cardiovascular health. |
| Swimming | A full-body workout that is gentle on the joints. |
| Stationary Bicycling | Cardiovascular exercise with reduced risk compared to outdoor cycling. |
| Stretching | Improves flexibility and relieves muscle tension. |
| Pelvic Floor Exercises | Strengthens the muscles supporting the bladder, uterus, and bowels, reducing urinary incontinence risks. |
| Low-Impact Aerobics | Safely elevates heart rate, enhancing endurance and circulation. |
When exercising during week 23, aim for at least 150 minutes of activities. Stay hydrated by drinking plenty of water before, during, and after exercise. Avoid high-risk activities such as excessive heat, and maintain proper hydration for health and safety during pregnancy.
What Can You Do To Prevent UTI At 23 Weeks Pregnant?
You can go for bacteriuria screening to prevent UTI at 23 weeks pregnant. Bacteriuria screening involves testing urine for bacteria, even if you have no symptoms, to allow for early detection and treatment, reducing the risk of complications from an infection.
A urine sample is collected and tested during the screening using urine culture sensitivity tests to detect any bacteria. Antibiotics are prescribed to treat the infection if bacteria are found, followed by additional tests to ensure the infection is cleared.
Incorporating routine bacteriuria screening into your regular antenatal care helps prevent the progression of symptomatic UTIs, avoiding potential complications for you and your baby.
Maintaining personal hygiene and strict sanitation practices during pregnancy is crucial in preventing UTIs. Pregnant women should especially adhere to these habits to reduce the risk of infection.
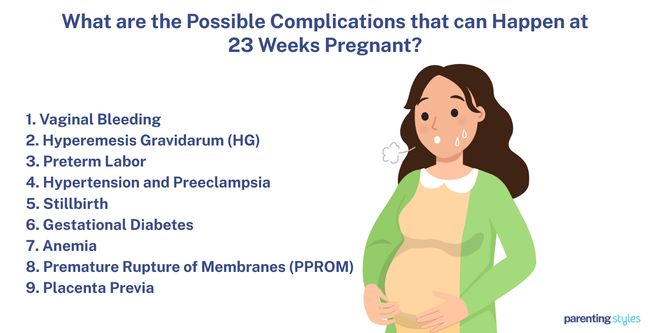
What Are The Possible Complications That Can Happen At 23 Weeks Pregnant?
- Vaginal Bleeding: Heavy or prolonged bleeding during pregnancy increases the risk of low birth weight and perinatal death, particularly when multiple episodes occur. Vaginal bleeding is experienced in about 25% of pregnancies and can triple the risk of preterm delivery, making it essential to seek prompt medical advice if bleeding occurs.
- Hyperemesis Gravidarum (HG): Hyperemesis gravidarum (HG) is a condition characterized by severe nausea and vomiting during pregnancy, leading to maternal dehydration, weight loss, and electrolyte imbalances. HG affects up to 10.8% of pregnant women and increases the risk of serious complications such as kidney failure or liver damage. For the fetus, HG is associated with risks like low birth weight, developmental delays, preterm birth, and intrauterine growth restriction.
- Contractions/Preterm Labor: True contractions pose significant risks to the fetus if they lead to preterm delivery between 22 and 37 weeks. These risks include respiratory distress, infections, and developmental delays. Preterm labor is believed to be triggered by an infection that causes inflammation, leading to contractions, membrane rupture, and cervical changes that ultimately result in early delivery.
- Hypertension and Pre-eclampsia: Pre-eclampsia is a serious condition that causes an increase in maternal blood pressure after the 20th week of pregnancy. Pre-eclampsia typically occurs in the second half of pregnancy and affects approximately 4.6% of pregnancies, while hypertension affects around 2.1%. These complications increase the risk of placental abruption, growth problems, and preterm birth.
- Stillbirth: Miscarriage refers to pregnancy loss before 20 weeks, while losses after 20 weeks are termed stillbirths. Key factors contributing to miscarriage include fetal abnormalities (chromosome issues), maternal health problems (incompetent cervix, hormonal imbalances, chronic conditions), and infections (bacterial). Stillbirth occurs in 0.3% of pregnancies between 20 and 27 weeks, although the likelihood of miscarriage decreases as pregnancy progresses.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) is a type of diabetes that develops during pregnancy, leading to elevated blood sugar levels. GDM increases maternal risks for conditions such as gestational hypertension, pre-eclampsia, cesarean section, and delivery complications. Additionally, both the mother and child face an increased risk of developing type 2 diabetes and cardiovascular problems later in life.
- Anemia: Anemia is a condition characterized by insufficient hemoglobin, the protein that carries oxygen in the blood. During pregnancy, the body’s need for iron increases to support the expanded blood volume and fetal growth. Iron deficiency during this time leads to low birth weight, preterm birth, and long-term cognitive issues in the baby, such as impaired memory and learning abilities.
- Premature Rupture of Membranes (PPROM): Premature Rupture of Membranes (PPROM) occurs when the amniotic sac ruptures before labor begins. This condition poses significant risks to the fetus, including pulmonary hypoplasia, limb deformities, placental abruption, cord prolapse, and infection. When PPROM occurs at 23 weeks, the survival rate for the fetus at discharge is only 39.5%, according to a 2018 study, “Preterm premature rupture of membranes at 22–25 weeks’ gestation: perinatal and 2-year outcomes within a national population-based study (EPIPAGE-2).”
- Placenta Previa: Placenta previa is a condition where the placenta is located near or over the cervix, leading to usually painless bleeding as the lower uterine segment (LUS) and cervix develop. The risk of significant bleeding increases with a low-lying placenta and can begin even before labor. In cases of significant bleeding, an emergency cesarean delivery is often required to ensure the safety of both the mother and baby.
How can a Partner Support the Mother at 23 Weeks Pregnant?
- Lifestyle Changes: Encourage and participate in healthy behaviors together, such as avoiding smoking and adopting a balanced diet, to positively influence the mother’s well-being and support the baby’s healthy growth.
- Emotional Support: Support your partner by actively listening, showing affection, empathy, and understanding, and being present during stressful times. Celebrating milestones like reaching 23 weeks likely helps reduce prenatal anxiety and strengthens your relationship.
- Physical Support: Take on household chores, grocery shopping, and meal preparation to relieve your partner of daily burdens. Engage in stress-relief activities together, such as gentle exercises or prenatal yoga, to reduce anxiety and contribute to a positive pregnancy experience.
- Physical Affection: Offer your partner a hug and show your affection through small gestures of intimacy. These acts of affection reduce partner stress and anxiety, enhance security, and promote well-being, according to a 2006 study, “Effective social support: Antecedents and consequences of partner support during pregnancy.”
- Open Communication: Engage in open dialogue with your partner by sharing your fears, concerns, needs, and insecurities while actively listening to theirs. Open communication deepens mutual understanding and fosters trust, helping both partners navigate pregnancy’s physical and emotional changes. This approach strengthens your bond and helps you feel more supported and connected throughout this journey.
- Mental Support: Offer your partner mental security by being present and maintaining a stable, safe environment. Providing consistent support significantly reduces maternal distress during pregnancy, helping your partner feel more secure and confident.
When to Call for Your Doctor if Something Feels Wrong at Week 23 of Pregnancy?
- Decreased Fetal Movement: In clinical settings, “normal” fetal movement at 23 weeks of pregnancy is typically defined as at least 10 movements within two hours. However, this can vary based on the mother’s perception of her baby’s activity. Decreased fetal movement (DFM) is a risk factor for complications such as fetal growth restriction, stillbirth, preterm birth, and emergency cesarean section.
- Severe Abdominal Cramping: Sudden and severe abdominal cramping at 23 weeks of pregnancy is sometimes a sign of severe conditions like ectopic pregnancy or intestinal obstruction. Ectopic pregnancy occurs when a fertilized egg implants outside the uterus, often in the fallopian tube. This can cause sharp abdominal pain and possible bleeding, although ectopic pregnancies usually occur earlier in pregnancy. Intestinal Obstruction is more likely to happen during the fourth and fifth months of pregnancy, just before week 23. As the uterus grows and moves into the abdomen, it places pressure against the intestines, potentially causing a blockage. Symptoms of intestinal obstruction include nausea, vomiting, and difficulty passing gas or stools.
- Vaginal Bleeding: Vaginal bleeding during the second trimester triples the risk of preterm labor, according to a 2013 study from Iran, titled “The relationship between vaginal bleeding in the first and second trimester of pregnancy and preterm labor,” conducted by Seyedeh Hajar Sharami, M.D. et al. at Guilan University of Medical Sciences and published in Iranian Journal of Reproductive Medicine. Preterm labor increases the chances of complications such as low birth weight and perinatal mortality and requires immediate attention.
- Dizziness or Fainting: Decreased blood flow to the brain or blood vessel dilation causes dizziness and fainting (syncope) during pregnancy, often preceded by lightheadedness, nausea, or palpitations. Call your doctor to assess your condition if you experience repeated or severe dizziness.
- Bad Smelling Vaginal Discharge: Pathological vaginal discharge (PVD) during pregnancy is a yellowish-green, foul-smelling discharge that is sometimes accompanied by itching or pain. This contrasts with normal vaginal discharge, which is typically clear or milky and odorless. Infections like bacterial vaginosis or candidiasis generally cause PVD and require prompt medical evaluation.
- Extreme/Sudden Swelling: Extreme swelling in the face and hands often indicates preeclampsia, a serious pregnancy condition characterized by high blood pressure. In addition to swelling, symptoms of preeclampsia include persistent headaches, confusion, vision problems, and sudden weight gain. Preeclampsia has severe consequences for both the mother and baby if left untreated.
- Fluid Leakage from Vagina: Fluid leakage from the vagina in the second trimester of pregnancy often signals Spontaneous Previable Rupture of Membranes (SPROM), a condition where the amniotic sac breaks prematurely, leading to fluid loss before labor is expected. SPROM increases the risk of preterm labor, pregnancy loss, and neonatal health complications. Contact your OB-GYN immediately if you notice persistent fluid leakage.
- Fever/Chills: 1 in 5 women report experiencing a fever during pregnancy, according to a 2014 study from Denmark, titled “Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring,” conducted by Anne-Marie Nybo Andersen et al. at University of Southern Denmark and published in Pediatrics. Elevated maternal body temperature during pregnancy, particularly 39°C (100.4°F) and over, increases the risk of fetal neural tube defects, congenital heart defects, and oral clefts.
- Regular or Frequent Contractions: Braxton-Hicks contractions feel like a tightening of your abdomen at 23 weeks but are not typically painful. Regular uterine activity includes fewer than three contractions per hour. However, severe or continuous pain usually indicates a problem. If you experience more than four contractions per hour, contacting your OB-GYN immediately is important.
- Mood and Anxiety Disorders: As pregnancy progresses, some pregnant women experience symptoms like depressed mood, loss of interest in activities, significant appetite changes, and physical discomforts like headaches or back pain. Depression scores of pregnant women tend to increase between weeks 18-32 of pregnancy, according to a 2003 study from Sweden, titled “Point prevalence of psychiatric disorders during the second trimester of pregnancy: a population-based study,” conducted by Liselott Andersson et al. at Umeå University and published in American Journal of Obstetrics and Gynecology. It is important to seek advice from your doctor if you feel constant fatigue, excessive worry, or difficulty concentrating.
- Excessive Vomiting: Excessive vomiting during pregnancy often indicates hyperemesis gravidarum, a severe condition leading to dehydration and weight loss. Hyperemesis gravidarum is linked to an increased risk of low birth weight, which can cause long-term health issues for the baby. If you experience persistent vomiting, dehydration, or weight loss or feel that something is wrong with the baby, call your midwife or OB-GYN for early interventions to these complications.

What are the 23 weeks pregnant symptoms not to ignore?
23 weeks pregnant symptoms not to ignore include decreased fetal movement, severe cramping, vaginal bleeding, fainting, bad-smelling vaginal discharge, sudden swelling, fluid leakage, fever, regular contractions, depression or anxiety symptoms, and excessive vomiting. Always trust your instincts during pregnancy. If something feels off at week twenty-three, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are there Prenatal Vitamins that need to be Taken during Week 23 of pregnancy?
Yes, essential vitamins should be taken during week 23 of pregnancy for optimal maternal and fetal health, as emphasized by ACOG.
Calcium at 1,000 mg helps build strong bones and teeth for both mother and baby as the baby’s skeletal structure develops.
Iron, at 27 mg, is crucial for producing red blood cells, delivering oxygen to the baby, and preventing anemia during pregnancy.
Iodine, at 220 mcg, supports healthy thyroid function and is key for the baby’s brain development and growth.
Choline at 450 mg is vital for the development of the baby’s brain and spinal cord, helping prevent neural tube defects.
Vitamin A, at 770 mcg, aids in developing the baby’s organs while supporting healthy skin, eyesight, and bones.
Vitamin C, at 85 mg, promotes healthy connective tissues, supports the immune system, and improves iron absorption.
Vitamin D, at 600 IU, ensures proper bone and teeth development by aiding in calcium absorption.
Vitamin B6, at 1.9 mg, helps with red blood cell production and supports the baby’s brain development while reducing pregnancy nausea.
Vitamin B12, at 2.6 mcg, is essential for red blood cell formation and nervous system health and prevents certain birth defects.
Folic acid at 400 mcg helps prevent birth defects of the brain and spine while promoting healthy placenta and fetal growth.
ACOG advises taking prenatal vitamins as directed, ensuring no more than the recommended doses are consumed. Taking a high-quality prenatal supplement daily ensures these vital nutrients are covered, helping to support both the mother’s health and the baby’s development through week 23. Always consult your OBGYN to ensure your diet and supplement regimen meet your specific needs during pregnancy.
What does Parenting Styles Suggest about 23 Weeks Pregnant?
Parenting Styles suggests monitoring fetal movement as a noticeable decrease in pattern must be reported to your OBGYN. Week 23 is the perfect time to capture the glow of motherhood in a stunning maternity photoshoot.
“Capture the magic of this moment. A maternity photoshoot is your forever keepsake,” advises Pamela Li, writer, Founder and Editor-in-Chief at Parenting Styles.
Congratulations on being 23 weeks pregnant!