24 Weeks Pregnant Symptoms: Week 24 Of Pregnancy And Prenatal Care
24 weeks pregnant symptoms include frequent urination due to the growing uterus pressing on the bladder, lower back pain from hormonal shifts and weight gain, and “pregnancy brain” characterized by forgetfulness. Another week-24 pregnancy symptom is fatigue, often worsened by sleep disturbances such as insomnia. Many mothers experience swelling (edema) in the lower limbs. Stretch marks appear on the abdomen, hips, and thighs as the skin stretches to accommodate the growing baby. Leg cramps and colostrum production, the first form of milk, are typical at week 24.
Understanding these changes helps expectant mothers manage symptoms effectively. Braxton Hicks contractions, or false labor pains, are common, and staying hydrated or adjusting sleep positions ease physical discomfort. Awareness of symptoms like skin changes, dizziness, and swelling allows self-care and reduces anxiety. Monitoring the baby’s movements and attending regular prenatal checkups ensure healthy development and early detection of complications like preterm labor.

Fetal development at 24 weeks is rapid. The baby weighs around 1.47 pounds and measures the size of an ear of corn. Significant milestones include brain maturation, the development of lungs, and the baby’s ability to hear external sounds. The baby gains body fat and hair, and facial expressions, such as smiling or grimacing, become more defined. The baby’s lungs start producing surfactants, necessary for breathing post-birth, while neural connections are rapidly forming. The baby’s movements, like kicks, become stronger and more noticeable, fostering a deeper connection between the parent and baby. Proper antenatal care and regular monitoring are essential for ensuring the baby’s health and preparing for delivery.
Babies born at 24 weeks, though facing health risks, have over an 81% chance of survival with modern neonatal care, according to a 2004 study from the United States titled “Survival and Long-Term Neurodevelopmental Outcome of Extremely Premature Infants Born at 23–26 Weeks’ Gestational Age at a Tertiary Center,” by Ronald E. Hoekstra et al., published in Pediatrics.
What is 24 weeks pregnant in months? 24 weeks pregnant is 6 months within the second trimester of pregnancy. You’ve finished the sixth month of pregnancy.
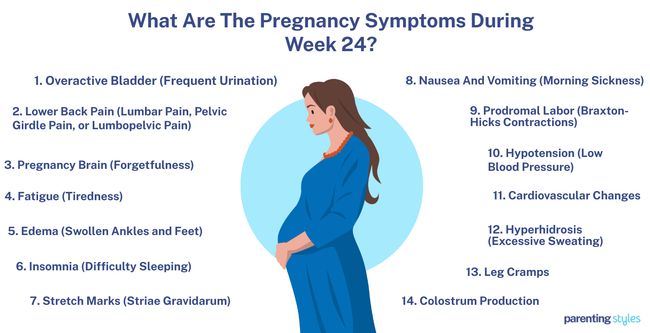
What Are The Pregnancy Symptoms During Week 24?
24 week pregnant symptoms include overactive bladder, lower back pain, pregnancy brain, fatigue, edema, sleeping difficulties, and stretch marks. Below are common 24 weeks pregnancy symptoms expectant mothers experience.
- Overactive Bladder (Frequent Urination): Overactive bladder syndrome (OAB) is the increased frequency and urgency of micturition (urination), usually with a nocturia (waking up at night to urinate). A 24-week pregnant mother with OAB often experiences a strong feeling of urgency to empty her bladder and has frequent urination. Overactive bladder is a urogenital symptom experienced by most mothers during pregnancy. Many women are not bothered by this symptom. Urinary incontinence (UI) accompanies OAB in some women and bothers some women. Urogenital symptoms increase with gestational age but tend to decrease rapidly after childbirth.
- Lower Back Pain (Lumbar Pain, Pelvic Girdle Pain, or Lumbopelvic Pain): Lumbopelvic pain refers to low back pain (LBP) and pelvic girdle pain (PGP). Hormonal changes during pregnancy lead to increased joint laxity, weight gain, and a shift in the body’s center of gravity, putting additional stress on the back and pelvis. Many pregnant women experience sharp, stabbing pain, commonly starting in the second trimester and intensifying between 24 and 36 weeks of pregnancy.
- Pregnancy Brain (Forgetfulness): 24-week pregnant mothers often have a “mom brain.” Pregnancy brain or baby brain refers to the subjective decline in cognition in up to 81% of pregnant women. Forgetfulness, reading difficulties, confusion, disorientation, poor concentration, increased absent-mindedness, and reduced motor coordination are manifestations of slowed cognition during pregnancy. Forgetfulness has significant real-world consequences, including impaired conversational fluency at work, frequent forgetting of appointments, and difficulties with reading comprehension.
- Fatigue (Tiredness): Fatigue is one of the most common pregnancy symptoms. It appears physically and mentally as a lack of energy, tiredness, and motivation. Antenatal fatigue weakens the cognitive performance and self-care capability of pregnant women. Tiredness reduces muscle endurance, delays healing after physical effort, and decreases the ability to restore sleep. A study showed that more than 96.5% of pregnant women experienced fatigue.
- Edema (Swollen Ankles and Feet): Lower limb edema is a symptom that often occurs during week 24 of pregnancy. Lower limb edema is swelling that occurs in the feet and lower legs. This swelling occurs due to venous hypertension, which is high blood pressure in the veins. An insufficient muscle pump and valvular regurgitation cause venous hypertension during pregnancy. Valvular regurgitation occurs when valves in the veins that help blood move back to the heart are damaged, causing blood to flow backward. The swelling is linked to venous thromboembolism, which is the formation of blood clots in the veins. Lower limb edema is characterized by symmetrical swelling that appears first in the feet and lower legs but impacts the entire leg. It is associated with heaviness, pain, and a bursting sensation in the limbs. 66.6% of pregnant women experience lower limb edema during their second trimester and more experience swollen ankles and feet in their third trimester.
- Insomnia (Difficulty Sleeping): Insomnia is a sleep disorder characterized by difficulty falling or staying asleep or waking up too early. Sleep disturbances occur in about 80% of pregnant women, with a noticeable decrease in total night-time sleep by 23-24 weeks of gestation, according to a 2016 study titled “Insomnia during Pregnancy: Diagnosis and Rational Interventions,” by Imran S. Khawaja. et al., published in Pak J Med Sci. Hormonal fluctuations, physical discomfort, and anxiety often worsen such issues, leading to increased fatigue and mood changes. Pregnancy symptoms like frequent urination, back pain, and fetal movements further contribute to sleep difficulties.
- Stretch Marks (Striae Gravidarum): Stretch marks initially appear as pink lesions on the pregnant mother’s skin as the skin stretches to accommodate the growing baby. Stretch marks develop in about 58.9% of pregnant women, typically on the abdomen, hips, breasts, and thighs. Stretch marks are most common between weeks 24 and 35 of pregnancy, according to a 2018 study from China titled “Risk factors of striae gravidarum in Chinese primiparous women,” conducted by Liping Liu et al. at Affiliated Hospital of Jiangsu University and published in PLoS ONE. The likelihood of developing stretch marks is higher in women of younger maternal age, women who experience significant weight gain, and those with a higher body mass index (BMI).
- Nausea and Vomiting (Morning Sickness): Nausea and vomiting in pregnancy (NVP) are not limited to the morning hours and happen throughout the day despite the popular name “morning sickness.”
- Prodromal Labor (Braxton-Hicks Contractions): Prodromal labor refers to false labor pains experienced during the second and third trimesters. Braxton-Hicks contractions feel like mild menstrual cramps or abdominal tightening. Contractions from prodromal labor are irregular, unpredictable, and uncomfortable. Prodromal labor is often triggered by factors like physical activity, a full bladder, sexual activity, or dehydration.
- Hypotension (Low Blood Pressure): Hypotension occurs when blood pressure drops below normal levels. Increased blood volume and decreased systemic vascular resistance during pregnancy contribute to lower blood pressure, while progesterone causes blood vessels to relax. The lowest blood pressure levels are recorded between weeks 20 and 24 of pregnancy, according to a 2014 study from the United States, titled “Physiologic and pharmacokinetic changes in pregnancy,” conducted by Maged M. Constantine at the University of Texas Medical Branch and published in Frontiers in Pharmacology.
- Cardiovascular Changes: Cardiovascular system changes involve adaptations in the heart and blood vessels during pregnancy to help meet the metabolic demands of the mother and the baby. Cardiac output increases by up to 45% compared to pre-pregnancy levels, maternal heart rate rises by 10-20 beats per minute, and vasodilation decreases systemic vascular resistance.
- Hyperhidrosis (Excessive Sweating): Hyperhidrosis is excessive perspiration, the body’s regulating temperature. Hormonal fluctuations stimulate heightened activity in the eccrine sweat glands, leading to increased sweating, according to a 2016 study from The United States, titled “Inflammatory and glandular skin disease in pregnancy,” conducted by Catherine S. Yang et al. at The Warren Alpert Medical School of Brown University, and published in Clinics in Dermatology.
- Leg Cramps: Leg cramping at 24 weeks pregnant is intense, painful muscle contractions that typically affect the calves or feet and often occur at night, disrupting sleep. Leg cramps at night sometimes lead to daytime fatigue and poor concentration. Cramping at 24 weeks pregnant is prevalent, with up to 30% of mothers experiencing leg cramps.
- Colostrum Production: Colostrum production is the secretion of colostrum from the breasts. Colostrum is the first form of milk produced by the breasts. Colostrum is produced to prepare the breasts for lactation after the birth.
What is the Importance of Understanding Being 24 Weeks Pregnant?
The importance of understanding being 24 weeks pregnant is to understand the physical and emotional changes to help manage symptoms effectively. The growing uterus exerts pressure on the bladder, leading to frequent urination and possible incontinence, while hormonal changes cause discomfort like lower back pain, round ligament pain, and insomnia. Braxton Hicks contractions, which are practice contractions for labor, sometimes occur; however, they are irregular and typically stop with a change in position. Awareness of these symptoms, including skin changes, dizziness, and loss of balance, enables pregnant women to take steps to alleviate discomfort. Staying hydrated and adjusting sleep positions help improve rest and ease discomfort. OBGYNs recommend monitoring the baby’s movements closely during this stage. Learning about pregnancy week by week can provide valuable insight.
Emotional changes are common, with “pregnancy brain” or forgetfulness being a well-recognized symptom. Understanding that forgetfulness is a natural reaction to pregnancy helps mothers cope with feelings of frustration and anxiety, which are intensified by fatigue and sleep disturbances. Knowing that leg cramps, stretch marks, and swelling are typical at this stage reduces worry and promotes self-care.
Week 24 marks a crucial phase in fetal growth, where the baby continues to develop rapidly in size, senses, and organ function. A 24-week baby weighs about 1.47 pounds and is around the size of an ear of corn (or a large turnip). Key developmental features include the maturation of the brain, lungs, and sensory organs. The brain is growing, and myelination (developing protective sheaths around nerves) begins and improves nerve function. The lungs start producing surfactants, a critical substance for breathing after birth. The baby’s inner ears are formed, allowing them to hear sounds. The baby’s ability to respond to light is established.
The baby gains more body fat, hair, eyelashes, and eyebrows. Taste buds, fingerprints, and footprints are developed, while neural connections supporting the baby’s senses and motor functions rapidly form. The first facial expressions, like smiling or grimacing, emerge. The baby’s movements become more noticeable, fostering a connection between the parent-to-be and the baby. Recognizing these milestones helps mothers feel more connected to their babies and provides reassurance that the baby is preparing for life outside the womb.
Babies born at 24 weeks face increased risks, but they are able to survive with the help of modern neonatal care, which has significantly improved the survival rate of preterm babies. The chance of survival in the 24th week is over 81% with expert care.
Understanding these developments is essential for monitoring the baby’s health and identifying potential complications. Regular prenatal checkups detect preterm labor or growth issues. Being informed at 24 weeks empowers mothers and promotes healthier outcomes. Preparing for labor and birth helps the parent-to-be feel more confident and ready for what lies ahead.
What to Expect at 24 Weeks Pregnant?
24-week pregnant mothers should expect physical and emotional changes as their baby develops rapidly. The growing uterus, now about 2 inches above the belly button, often puts pressure on the bladder, leading to frequent urination and sometimes overactive bladder symptoms, including an urgent need to urinate and nocturia (waking up at night to urinate). Urinary incontinence is bothersome but is one of the common second-trimester symptoms.
Many women experience lower back pain caused by hormonal changes that relax joints and shift the body’s center of gravity, intensifying pressure on the back and pelvis. Round ligament pain, which feels like a sharp pain on the sides of the abdomen or hip area, is common due to the stretching of ligaments as the womb tilts and grows.
Forgetfulness or “pregnancy brain” is prevalent during week 24. Many mothers find themselves more absent-minded, having trouble concentrating or struggling with memory. Mom’s brain often interferes with daily activities, but it is a normal response to pregnancy. Tiredness is another common experience at 24 weeks.
Fatigue occurs and is worsened by difficulty sleeping. Insomnia often occurs due to discomfort, frequent urination, or anxiety. Leg cramps often disrupt sleep at night, exacerbating sleeping problems.
Stretch marks appear as the skin stretches over the abdomen, breasts, hips, and thighs to accommodate the baby’s growth. These areas sometimes feel itchy as the skin tightens and expands. Darker patches or red streaks develop in areas where the skin stretches the most.
Swollen or bleeding gums are another symptom caused by increased blood flow during pregnancy. Swollen ankles and feet (edema) are common, often due to increased blood volume and pressure on veins, which sometimes lead to blood clots. Headaches, indigestion, heartburn, bloating, constipation, and nosebleeds are common in week 24.
The 24-week baby’s brain is growing rapidly. The baby’s senses, including hearing, develop, allowing the baby to respond to sounds outside the womb. Facial expressions, such as smiling and grimacing, emerge. The baby’s eyebrows and eyelashes are developing, and hair on the head is becoming more visible. The baby’s muscle control is improving, and movements, such as pokes and kicks, are becoming stronger and more noticeable. Loss of balance and dizziness sometimes occur due to the growing baby and shifting body dynamics.
The baby’s lungs enter the saccular stage of development, with the first production of surfactant, a substance crucial for breathing after birth. The skin develops its protective outer layer. The week-24 baby is starting to respond to light and sound, blinking and showing facial expressions in response to stimuli. Internally, the baby’s neural connections form, supporting the development of senses and motor functions.
The 24-week-old fetus weighs about 1.47 pounds and is roughly the size of an ear of corn. The baby’s movements are stronger and more noticeable, including kicks and pokes felt by placing a hand on the belly. The baby papers for life outside the womb, achieving significant milestones such as sucking and responding to sounds, which are critical for feeding and interaction after birth.
How Is The Baby Developing At 24 Weeks Pregnant?
Your 24-week-old baby is around the size of an ear of corn and weighs approximately 665 grams (about 1.47 pounds). Your baby grows rapidly. Rather than measuring crown-to-rump length (8 inches long), the focus now shifts to parameters like biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and humerus length (HL). The average measurements at this stage are a BPD of 60 millimeters, HC of 222 millimeters, AC of 197 millimeters, and femur and humerus lengths around 43 millimeters. These measures are detailed in a 2017 study titled “The World Health Organization Fetal Growth Charts: A Multinational Longitudinal Study of Ultrasound Biometric Measurements and Estimated Fetal Weight,” by Kiserud, T. et al., published in Plos Medicine.
Your baby is developmentally making significant strides. The face is almost fully formed, with a full set of eyelashes and eyebrows. Hair is present, with some growing on the head. The baby’s skin is wrinkled and translucent, with a pink to red color due to blood visible through the capillaries. The baby is gaining more fat, including brown fat, which helps regulate body temperature by burning lipids to generate heat.
Facial expressions begin to emerge, reflecting early emotional engagement. The lungs undergo rapid maturation, becoming more complex with the formation of terminal sacs and the production of pulmonary surfactant cells to support breathing after birth. Babies born at this stage often face respiratory challenges because the lungs are still developing.
The baby’s inner ears are fully developed, giving the baby a sense of balance. The brain grows rapidly, and the senses are becoming more refined. The taste buds are more sensitive, and the eyes begin to respond to light, marking substantial progress in sensory development. Hearing is developed, allowing your baby to hear sounds outside the womb.
The skin’s outer protective layer, the stratum corneum, starts developing around this time, while the olfactory system allows the baby to begin sensing smells in the amniotic fluid. Neural development progresses with the initiation of myelination, and your baby starts to blink, indicating early sensory processing. The buildup of fat tissue, essential for temperature regulation and energy storage, increases.
Your baby’s auditory system is now mature enough to hear sounds from outside the womb, and the sucking reflex begins to develop, which is vital for feeding after birth. The baby’s eyes are functional, helping the baby respond to light and establish circadian rhythms.
How Big is Your Baby at Week 24 of Pregnancy?
Your 24-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 24-week-old fetus is about the size of an ear of corn. The 50th percentile measurements for 24-week fetal growth are as follows: the biparietal diameter (BPD) is 60 millimeters, the head circumference (HC) is 222 millimeters, the abdominal circumference (AC) is 197 millimeters, the femur length (FL) is 43 millimeters, and the humerus length (HL) is 41 millimeters. The 24-week-old fetus weighs 665 grams (23.46 ounces or 1.47 pounds), according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
What are the Key Developmental Milestones of Babies at Week 24 of Pregnancy?
The developmental milestones for babies in week 24 include engaging facial expression, mature lungs, and terminal sacs. The 11 developmental milestones are listed below.
- Facial Expressions: Facial expressions are early signs of fetal emotional and social engagement. Fetuses respond with mouth-opening movement when mothers sing nursery rhymes, suggesting fetuses mimic or respond with rudimentary mirroring behaviors at 24 weeks pregnant, according to a 2016 study from Italy titled “Ultrasonographic Investigation of Human Fetus Responses to Maternal Communicative and Non-communicative Stimuli,” by Pier F. Ferrari et al., published in Frontiers in Psychology.
- Mature Lungs: Lung maturation refers to the development of the fetal lungs in the canalicular phase of development from weeks 16 to 27 of pregnancy. Your baby’s lungs have formed most airways and developed smooth muscle to help regulate fluid movement during the canalicular stage. The lungs mature to resemble adult lungs by week 24 of pregnancy, with a blood-gas barrier thin enough to support effective gas exchange and survival after birth. Lung maturation is outlined in a 2013 study from the United Kingdom, titled “Early lung development: lifelong effect on respiratory health and disease,” conducted by Janet Stocks et al. at University College London and published in The Lancet Respiratory Medicine.
- Terminal Sacs: Terminal sacs (saccules) are clusters of airspaces in the developing lungs. Saccules start forming around 24 weeks of pregnancy and are initially made up of type II pneumocytes that mature and differentiate into type I. During the saccular stage of lung development, which starts in pregnancy week 24, the airways expand, and thin-walled terminal sacs with a double capillary network develop. The Type II pneumocytes produce pulmonary surfactant in week 24, which is crucial for fetal lung stability. Infants born at 24 weeks often struggle with immature lungs and insufficient surfactant.
- Mature Outer Layer in Skin: The mature outer layer of skin is called the stratum corneum (SC). The epidermis is thinner in infants, and the corneocytes are smaller than in adults, leading to a weaker skin barrier and increased susceptibility to harmful elements. The SC begins to mature at around 24 weeks of pregnancy and fully develops by about 34 weeks, acting as a barrier against moisture and harmful substances.
- Smell: Fetuses begin to detect odor-active molecules in the amniotic fluid by 24 weeks of pregnancy. The fetal nasal orifices open now, allowing olfactory sensory neurons to develop and detect smells. Early exposure to flavors in the amniotic fluid helps prepare newborns for the postnatal environment by familiarizing them with different scents and tastes.
- Myelination and Formation of Neural Connections: Myelin (a fatty substance) forms around nerve fibers for better signal transmission. At 24 weeks pregnant, thalamocortical axons advance into the somatosensory, auditory, visual, and frontal cortices, helping with processing sensory information and performing higher-level cognitive functions. Myelination of the corticospinal tract is underway, allowing the fetus to respond to stimuli.
- Blinking: Blinking is the action of opening and closing the eyelids, observable between 23 and 26 weeks of gestation. Blinking indicates active communication between the developing nervous system and the eyes. Blinking is triggered by light stimuli at 24 weeks pregnant, reflecting early visual processing in the brain.
- Increase in Fat Tissue: Fat tissue is crucial for insulation and energy storage in the developing baby. Precursors for fat cells (adipocytes) appear by week 14. Adipogenesis (formation of adipocytes) is regulated by insulin, which stimulates fatty acid synthesis from glucose. Fetuses of diabetic and obese mothers often accumulate more fat, affecting the risk for future obesity.
- Hearing/Auditory Startle Reflex: The auditory startle reflex indicates that the baby’s auditory system functions as the fetus responds to sounds. The cochlea (spiral structure in the inner ear) has matured enough to detect and convert sound waves into electrical signals. The baby hears external sounds such as voices or music by 24 weeks.
- Start of Sucking: Sucking is characterized by tongue movement from back to front, typically starting between 18 and 24 weeks of gestation, coinciding with the myelination of the brain stem. A fetus exhibits rhythmic sucking patterns by 24 weeks pregnant. The coordination of swallowing and breath control are milestones and precursors to oral feeding after birth.
- Functional Eyes: Functional eyes refer to the ability of the eye to perceive and respond to light, enabling the baby to see. The baby’s retina contains cells to help regulate the circadian timing system by 24 weeks pregnant. The cells send light information to the brain’s suprachiasmatic nuclei (SCN), which are crucial for maintaining circadian rhythms and supporting growth.

How to Know if Your Baby is Healthy During Week 24 of Pregnancy?
To know if your 24-week-old baby is healthy, symphysis-fundal height, fetal measurements, and ultrasound biometry are helpful indicators. Here are 7 ways to tell if your baby is healthy during week 24 of pregnancy.
- Symphysis-Fundal Height (SFH) Measurement: SFH is an outdated method of fetal growth measurement. Fundal height is measured from the top of the uterus (fundus) to the pubic bone and recorded every few weeks to observe trends and identify potential issues at 24 weeks pregnant.
- Fetal Measurements: An OBGYN uses ultrasound to provide data on fetal size and estimated fetal weight (EFW) to better manage growth concerns.
- Ultrasound Biometry: OBGYNs compare fetal measurements to established normal values for the gestational age. For example, the mean total fetal lung volume is approximately 27.8 mL at week 24, with measurements below expected ranges often suggesting issues like underdevelopment of the lungs, according to a 2018 study from The United States, titled “Fetal Lung Volumes by MRI: Normal Weekly Values From 18 Through 38 Weeks’ Gestation,” conducted by Mariana L. Meyers et al. at Department of Pediatric Radiology, Children’s Hospital Colorado, University of Colorado Denver, and published in American Journal of Roentgenology.
- Fetal Spine Length: Fetal spine length averages about 121.5 mm by week 23. A regression equation shows spine length increases by about 7.16 mm per week, and shorter lengths indicate congenital anomalies like skeletal dysplasia.
- Cerebroplacental Ratio: An OBGYN calculates the cerebroplacental ratio (CPR) by comparing the pulsatility index of the middle cerebral artery (MCA) to the pulsatility index of the umbilical artery (UA). A low CPR indicates potential fetal growth issues, according to a 2018 study titled “A Low Cerebroplacental Ratio at 20–24 Weeks of Gestation Can Predict Reduced Fetal Size Later in Pregnancy or at Birth,” by Roberto Romero et al., published in Fetal diagnosis and therapy.
- Fetal Ear Length: The fetal ear length at week 24 is typically about 19.72 mm. Ear length is measured from the helix (top) to the earlobe (bottom). Fetal ear lengths significantly shorter than expected often indicate an increased risk for Down syndrome.
- Amniotic Fluid Index: An OBGYN monitors the Amniotic Fluid Index (AFI) to assess fetal health using a special formula to measure the amniotic fluid in the belly. An AFI ranges from 5 to 25 cm normally. An AFI below 5 cm indicates oligohydramnios (low fluid), while an AFI above 25 cm indicates polyhydramnios (excess fluid).
Does Your Baby’s Brain Development Finish at 24 Weeks Pregnant?
No, your baby’s brain development does not finish at 24 weeks pregnant. Some brain areas are present in the fetus, but complete development continues beyond 24 weeks. Brain structures, such as the basal nuclei and cerebellum, are still maturing at 24 weeks, and the fetal brain forms essential connections. Significant growth continues, especially in the brain’s circadian system, which regulates sleep and hormone release.
Preterm infants born at 24 weeks often face challenges, including lower brain volumes in crucial sensorimotor regions. Babies born at 24 weeks of gestation have a chance of survival, although brain development is incomplete, leading to potential cognitive and developmental issues. Exposure to consistent light-dark cycles in NICUs improves outcomes and supports brain development.
Can Your Baby Already Hear Externally From the Womb at 24 Weeks Pregnant?
Yes, your baby hears external sounds from the womb at 24 weeks pregnant. The fetus begins to detect and respond to sound stimuli around 23 weeks of gestation, particularly to lower frequencies. The cochlea, responsible for hearing, is fully formed with functional hair cells by 24 weeks of pregnancy. The presence of startle reflexes to sound indicates the auditory pathways between the ear and the brain are operational. Consistent responses to sounds such as music and speech are noted by 24 weeks.
Prenatal exposure to sound influences memory and learning, according to a 2023 study from Iran, titled “The impact of sound stimulations during pregnancy on fetal learning: a systematic review,” conducted by Morteza Ghojazadeh et al. at Tabriz University of Medical Sciences and published in BMC Pediatrics. The research discusses how babies learn and remember sound patterns in the womb, which affect behavior after birth.
Infants exposed to specific sounds in the womb display preferences for such sounds when tested neonatally. The quality and type of sound, such as music or maternal voice, significantly impact the baby’s learning. The intensity (loudness) and frequency (pitch) of sounds affect how the sound reaches the fetus. External sounds are less intense due to sound dampening by the abdomen and amniotic fluid, and low-frequency sounds like voices are heard better.
What Are The Changes In The Mother’s Body At 24 Weeks Pregnant?
The changes in the mother’s body at 24 weeks pregnant include having an overactive bladder, ligament stretching, and pregnancy brain. Mother’s body changes are influenced by hormonal shifts, the physical demands of pregnancy, and the baby’s development, as listed below.
- Bladder Changes (Frequent Urination): The expanding uterus puts pressure on the bladder, leading to frequent urination. Many women experience an overactive bladder at this stage, often accompanied by the need to urinate more frequently, including waking at night.
- Ligament Stretching: The body adjusts as the uterus grows. The round ligaments supporting the uterus stretch, causing sharp pains in the abdomen and hips.
- Cognitive Changes (Pregnancy Brain): Hormonal shifts lead to changes in cognitive function, commonly referred to as “pregnancy brain” or “baby brain.” Forgetfulness, confusion, and difficulty focusing are frequent complaints as the brain adapts to pregnancy.
- Fatigue: Tiredness is prevalent during pregnancy as the body expends energy supporting the growing baby. Hormonal changes and physical discomfort contribute to feelings of exhaustion. Sleeping problems (insomnia) are common at 24 weeks and compound the problem.
- Swelling and Edema: Many women experience swelling, particularly in the feet and legs, due to fluid retention and increased pressure on the veins. Edema is when the legs feel swollen, heavy, and uncomfortable. The increased blood flow lead to swollen and bleeding gums.
- Skin Changes and Stretch Marks: The skin on the abdomen, breasts, hips, and thighs stretches to accommodate the growing baby, often resulting in stretch marks. The skin stretching causes itchiness as the skin adjusts to the rapid changes.
- Sleep Disruptions: Hormonal fluctuations, physical discomfort, and the need for frequent urination often disrupt sleep. Many pregnant women find it difficult to fall asleep or stay asleep due to back pain, baby movements, and the increasing size of the uterus.
- Digestive Changes: Hormonal changes slow digestion, leading to indigestion, heartburn, bloating, and constipation. Digestive issues are common at 24 weeks as the growing uterus puts pressure on the stomach and intestines.
- Muscle Cramps and Leg Pain: Many women experience leg cramps at night, often due to changes in circulation and pressure on nerves caused by the growing uterus. Leg cramps are painful and disrupt sleep.
- Breast Changes (Colostrum Production): The breasts sometimes start producing colostrum, the first form of milk at the twenty-fourth week. This signals the body’s preparation for breastfeeding after birth.
- Temperature Regulation (Feeling Hot and Sweating): Hormonal changes cause pregnant women to feel warmer than usual. Excessive sweating (hyperhidrosis) is common as the body works harder to regulate temperature.
- Cardiovascular Adjustments: The heart works harder during pregnancy, with increased blood flow and a higher heart rate to support the baby. Many women experience low blood pressure (hypotension), especially between weeks 20 and 24, due to relaxed blood vessels.
- Muscle Changes: Pregnancy hormones continue to loosen ligaments and muscles, contributing to discomfort in various body parts, including the ribs, back, breasts, and bottom. Muscle loosening helps prepare the body for labor but leads to aches and pains.
The changes in the mother’s body are a natural part of pregnancy as the body adjusts to support the mother and the baby. Understanding these symptoms helps expectant mothers manage their pregnancy with greater awareness and care.
How Big is a 24-Weeks Pregnant Belly?
A 24-week pregnant belly has a fundal height of around 24 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 24-week-pregnant belly measures around 24 centimeters, between 22 to 26 centimeters. The expanding uterus grows to accommodate the growing fetus. The 24-week pregnant uterus has grown enough to be palpated above the navel level.
Several factors affect uterine size and growth rate, such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than those with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth in the past. However, the 2016 World Health Organization (WHO) ANC Guidelines concluded that there was inadequate evidence of using the SFH to predict fetal health.
Are Carpal Tunnel Syndrome Common at 24 Weeks Pregnant?
Yes, Carpal Tunnel Syndrome (CTS) is common at 24 weeks pregnant. Hormonal changes, weight gain, and fluid retention contribute to CTS development. Carpal Tunnel Syndrome is characterized by pain and tingling in the hands, which disrupt daily activities and sleep.
CTS onset in pregnant women occurs around 18.1 weeks, with approximately 2.8% affected. A CTS diagnosis is commonly given before the third trimester, although symptoms often peak later. Risk factors for Carpal Tunnel Syndrome include obesity, excessive weight gain, and higher parity (number of previous births).
Signs of CTS include numbness, tingling, and wrist pain, which often worsen with pregnancy progression. Fluid buildup and changes in body weight cause compression of the median nerve in the wrist. Most pregnancy-related CTS cases are mild and self-limiting, resolving after childbirth and managed with non-surgical treatments.
Can You Feel Contractions as Early as 24 Weeks Pregnant?
Yes, you can feel “practice” contractions, called Braxton Hicks contractions, as early as 24 weeks pregnant. The frequency of Braxton Hicks contractions often varies at 24 weeks, with some women experiencing them more frequently than others. Braxton Hicks contractions are often not painful, and the intensity changes with different positions or activities. Monitoring contractions is important, as a higher frequency often indicates potential complications.
What Are The Tips for Prenatal Care During Week 24?
Tips for prenatal care during week 24 include taking prenatal vitamins, tracking fetal movement, and maintaining a healthy lifestyle. Here are 8 tips for prenatal care during week 24.
- Take Prenatal Vitamins: Taking prenatal vitamins during week 24 and throughout your pregnancy provides you and your baby with the necessary nourishment for healthy growth. Essential nutrients include folic acid, iron, calcium, vitamin D, choline, omega-3 fatty acids, and B vitamins. Folic acid prevents birth defects in the baby’s brain and spine, while iron supports blood production. Calcium is vital as it supports your baby’s bone development, while vitamin D aids calcium absorption. Be sure to include iron-rich foods like lean meat, green vegetables, dried fruit, and lentils, as well as calcium-rich foods such as dairy products, oranges, nuts, pulses, and broccoli to supplement your diet.
- Track Fetal Movement: Maternal perception of fetal movements remains the oldest and most common method for assessing fetal well-being. A noticeable decrease in fetal movements sometimes indicates complications, such as stillbirth or fetal growth restriction. At 24 weeks pregnant, it’s important to remain attentive to your baby’s daily activity and promptly alert your OB-GYN if you notice any drastic changes in movement.
- Maintain a Healthy Diet and Lifestyle: Eat a varied diet that includes all food groups to support their health and their baby’s growth. A healthy diet helps prevent anemia. Stay hydrated by drinking plenty of liquids and incorporating fiber-rich foods into your meals to maintain digestive health. Modifying your daily routine, such as adjusting your work posture and avoiding heavy lifting by bending your knees and keeping your back straight, helps ease pregnancy-related discomforts.
- Engage in Physical Activity: Regular physical activity, such as walking and swimming, helps manage pregnancy-related discomforts. Physical activity (PA) positively impacts physical and psychological well-being during the second and third trimesters. Moderate physical activities improve overall health, boost energy levels, enhance mood, and help reduce common pregnancy issues, such as backaches. Following a routine at week 24 that includes physical activity helps promote a more enjoyable pregnancy experience.
- Attend Prenatal Care Visits: Regular consultations with your OBGYN ensure consistent maternal and fetal health monitoring through tailored advice and prenatal screening. This is a great time to discuss childbirth preferences with your OBGYN and birth partner and ensure you’re prepared for upcoming tests and appointments.
- Prepare for Parenting: Seek realistic information on parenting skills and attend antenatal classes focusing on infant care, breastfeeding, and the roles and responsibilities of new parents. Consider discussing your childbirth preferences and engage in pelvic floor exercises recommended to support childbirth and postpartum recovery. Educate yourselves about managing relationship changes and adjusting to new responsibilities together to help ease your transition into parenthood.
- Practice Relaxation Techniques: Relaxation exercises such as mindfulness or walking help improve heart rate, blood pressure, stress, and emotional health. Avoid stress to maintain emotional well-being. Ask for help with heavy housework. Maternal relaxation practices contribute to a calmer in-utero environment.
- Prepare for Labor and Delivery: Active participation in antenatal education classes as part of prenatal care provides realistic insights into parenting. Access information on newborn care and resources to help navigate the changes ahead. Maintain healthy eating habits and limit caffeine intake to less than 200 mg per day.

What Types of Foods are Beneficial to Eat During Week 24 of Pregnancy?
Nutrition is more important than ever during week 24 of pregnancy, as it supports your health and your baby’s development. A well-balanced diet rich in key nutrients like folate, protein, iron, and calcium is essential. Here are examples of beneficial foods to include.
- Calcium: For strong bones and teeth, try sardines, cheese, and dark green leafy vegetables.
- Iron: To help deliver oxygen to your fetus, include prune juice, lean red meat, and iron-fortified cereals.
- Iodine: Important for brain development; consider seafood, dairy products, and eggs, the gold standard of prenatal protein (fried, scrambled, or hard-boiled).
- Choline: Crucial for brain and spinal cord development. Eat peanuts, beef liver, and milk.
- Vitamin A: To help with red blood cells, including sweet potatoes, carrots, and green leafy vegetables.
- Vitamin C: For healthy gums and bones, have strawberries, broccoli, and tomatoes.
- Vitamin D: To build bones and teeth, consume fatty fish such as salmon, sunlight, and fortified milk.
- Vitamin B6: For red blood cell formation, enjoy whole-grain cereals, bananas, and pork.
- Vitamin B12: Essential for the nervous system, including fish, poultry, and milk.
- Folic Acid: To prevent birth defects and support growth, try fortified cereal, dark green leafy vegetables, and orange juice.
- Whole Grain: Include plenty of whole grains like quinoa, oats, and brown rice, and healthy fats from sources such as avocados, nuts, and olive oil.
- Dairy: Choose fat-free or low-fat options like yogurt and pasteurized milk.
- Fruits: Choose fresh, frozen, or dried fruit, with whole fruit better than juice.
- Vegetables: Add raw, frozen, or dried vegetables for essential nutrients like calcium and protein.
- Protein: Include seafood, beans, and eggs to ensure you get enough protein, iron, and omega-3s.
Hygiene during pregnancy is important to reduce the risk of listeriosis and salmonella, especially when consuming eggs, dairy, and seafood. Monitor your weight and prevent nutritional imbalances. Maintaining proper nutrition to support a healthy pregnancy is especially beneficial to overweight mothers.
Be mindful that a diet deficient in iron or essential vitamins does not provide sufficient nutrients for you or your baby. Nutrient-rich foods meet your increased demands during pregnancy.
Is Eating More Small Meals Better than Eating Three Big Meals at 24 Weeks Pregnant?
Yes, eating more small meals is better than eating three big meals at 24 weeks pregnant. Smaller, more frequent meals reduce stress on the body compared to fewer large meals. Women who ate regular meals with snacks were less likely to experience complications like preterm delivery.
Skipping meals and eating less frequently negatively impact pregnancy outcomes. Women who skipped meals are often heavier before pregnancy and at a higher risk of preterm birth, according to a 2001 study titled “Frequency of Eating During Pregnancy and Its Effect on Preterm Delivery” conducted by Siega-Riz et al. at the University of North Carolina and published in the American Journal of Epidemiology.
Prolonged periods without food cause stress on the body and affect fetal health.
Maintaining a regular eating schedule with more small meals aligns with health recommendations for pregnancy, supports better maternal nutrition, and reduces the risk of complications for healthier pregnancy outcomes.
What Exercises Can You Do during Week 24 of Pregnancy?
Safe and moderate exercises benefit you and your baby. The 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour and the Centers for Disease Control and Prevention (CDC) suggest that pregnant women aim for 30 minutes/day, 5 days/week of moderate activity, such as walking or swimming, for overall health benefits.
- Walking: A great way to stay active, walking keeps your body moving without putting too much stress on your joints. This brisk, low-impact activity is often considered one of the safest exercises during pregnancy.
- Swimming: Exercising in water supports your body while helping improve your cardiovascular fitness and strength. It prevents overheating and relieves pressure on the back and legs, making it a therapeutic and effective way to stay fit.
- Stationary Bicycling: Biking helps build endurance and is a safe way to get your heart rate up without the risk of falls. Cycling outdoors tends to be riskier due to the high-risk falling potential, so opting for stationary bikes is advised.
- Stretching: Gentle stretches help improve flexibility, reduce stress, and ease common pregnancy discomforts. Practicing low-impact yoga is a safe way to stay active during pregnancy.
- Pelvic Floor Muscle Training (Kegels): Strengthening your pelvic floor muscles is essential during pregnancy to help prevent urinary incontinence and prepare for childbirth. Kegel exercises are particularly beneficial and are recommended as safe throughout pregnancy.
Physical activities, especially during the 24th week, help boost cardiovascular health, improve muscular fitness, and maintain flexibility. Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, according to the WHO recommendations. Don’t forget to drink plenty of water, avoid overheating, and steer clear of activities that involve high risks of falling or excessive physical contact. Search for free online prenatal workout videos for safe exercise routines and suggestions tailored for pregnancy.
What Are The Things To Avoid At 24 Weeks Pregnant?
Things to avoid at 24 weeks pregnant include alcohol, smoking, and recreational drugs. Here are 18 things to avoid at 24 weeks pregnant.
- Alcohol: It’s essential to avoid alcohol during pregnancy. Alcohol often leads to severe developmental problems and birth defects like fetal alcohol spectrum disorders (FASD). Even small amounts have negative impacts on the baby’s development, according to the 2020 study “Alcohol Use in Pregnancy” by Oregon Health and Science University, published in Clinical Obstetrics and Gynecology. Alcohol passes through the placenta, making it dangerous for the baby.
- Smoking and Secondhand Smoke: Smoking poses risks such as miscarriage, premature birth, and low birth weight. A 2020 study titled “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy” highlights the dangers of smoking and exposure to secondhand smoke during pregnancy. Tobacco passes through the placenta, leading to harmful effects on the baby’s development.
- Recreational Drugs: Recreational drugs harm the developing baby, leading to health issues like low birth weight, birth defects, and developmental delays. Similarly, drugs cross the placenta and negatively affect the baby’s growth and health.
- Cannabis: Cannabis use during pregnancy is linked to low birth weight and other complications. It’s best to avoid it to protect your baby’s development.
- Caffeine: Keep caffeine intake under 200mg daily to reduce the risks of miscarriage and low birth weight. Excessive caffeine consumption sometimes causes complications. Caffeine is commonly found in soda, tea, and coffee and needs to be minimized during pregnancy.
- Certain Medications and Supplements: Consult your healthcare provider before taking any medications, supplements, or herbal remedies, as some are harmful during pregnancy. Always check if they are safe to use during pregnancy.
- High Mercury Fish: Fish like swordfish, king mackerel, and sharks contain high levels of mercury and must be limited to protect the baby’s developing nervous system. Sushi and other fish high in mercury must be avoided during pregnancy.
- Undercooked or Raw Meat: Consuming raw or undercooked meats exposes you to harmful bacteria, increasing the risk of foodborne illnesses like toxoplasmosis. Raw or undercooked meat must be avoided during pregnancy to reduce this risk.
- Unwashed Vegetables and Fruits: Thoroughly wash all produce to avoid exposure to toxoplasmosis and other harmful bacteria. Pre-prepared fruits and vegetables that are unwashed pose a similar risk.
- Deli Meats: Deli meats harbor harmful bacteria unless thoroughly heated. It’s safest to avoid them unless they are reheated to steaming hot. Deli meats have been associated with risks such as listeria, which are particularly harmful during pregnancy.
- Unpasteurized Foods: Avoid unpasteurized dairy products and soft cheeses (like brie and feta) as they risk listeria infection, which harms your pregnancy. Soft cheeses and unpasteurized milk are especially risky if they haven’t undergone pasteurization.
- Bagged Salads: Pre-packaged salads tend to contain bacteria, so it’s better to avoid them. Foods sitting out too long often harbor bacteria.
- Strenuous Activities or Contact Sports: Engage in moderate exercise, but avoid high-risk activities that are more likely to lead to falls or abdominal trauma. Contact sports and activities like heavy lifting must be avoided during pregnancy to minimize risks.
- Exposure to Chemicals and Toxins: Be cautious about exposure to household cleaners, pesticides, and other chemicals. Always use protective gear when necessary, as exposure to hazardous chemicals is harmful during pregnancy.
- Hot Tubs and Saunas: Avoid hot tubs and saunas as the heat harms the developing fetus. Scuba diving is risky due to pressure changes that likely affect the baby.
- Cat Litter: Wear gloves when changing cat litter and practice proper hygiene to avoid toxoplasmosis, a parasitic infection that is harmful during pregnancy. Kitty litter exposure carries risks due to harmful fumes and bacteria.
- Stress: It is important to find ways to manage stress. Incorporate relaxation techniques to combat chronic stress that negatively affects your baby’s development.
- Pregnancy symptoms, such as Braxton-Hicks contractions and dry eyes, contribute to stress during this time.
- Hair Dye: While evidence is inconclusive, some studies suggest hair dye poses risks during pregnancy. A 2018 study published in BMC Pregnancy and Childbirth raised concerns about pre-pregnancy hair dye exposure and birth weight. Consult your doctor if you have concerns.
By staying informed and avoiding these things at 24 weeks pregnant, you help ensure a safer and healthier pregnancy. Always check with your healthcare provider for any specific guidance.
What are the Possible Complications that Can Happen at 24 Weeks Pregnant?
Possible complications that can happen at 24 weeks pregnant include vaginal bleeding, hyperemesis gravidarum, and preterm labor. 11 possible complications in week 24 are listed below.
- Vaginal Bleeding: Heavy or prolonged bleeding during pregnancy increases the risk of low birth weight and perinatal death, particularly when multiple episodes occur. Vaginal bleeding is experienced in about 25% of pregnancies and triples the risk of preterm delivery. Severe complications like this require prompt medical advice, as they potentially indicate dangers to mother and baby.
- Hyperemesis Gravidarum (HG): Hyperemesis gravidarum (HG) is a condition characterized by severe nausea and vomiting during pregnancy, leading to maternal dehydration, weight loss, and electrolyte imbalances. HG affects up to 10.8% of pregnant women and increases the risk of serious complications such as kidney failure or liver damage. For the fetus, HG is associated with risks like low birth weight, developmental delays, preterm birth, and intrauterine growth restriction. Maternal complications such as anemia arise due to HG, further increasing risks.
- True Contractions/Preterm Labor: True contractions pose significant risks to the fetus if they lead to preterm delivery between 22 and 37 weeks. These risks include respiratory distress, infections, and developmental delays. Preterm labor is believed to be triggered by an infection that causes inflammation, leading to contractions, membrane rupture, and cervical changes that ultimately result in early delivery. Babies born at 24 weeks face an increased risk of disability, including problems with movement, talking, hearing, and learning.
- Hypertension and Pre-eclampsia: Pre-eclampsia is a serious condition that causes an increase in maternal blood pressure after the 20th week of pregnancy. Pre-eclampsia typically occurs in the second half of pregnancy, affecting approximately 4.6% of pregnancies, while hypertension affects around 2.1%. These complications increase the risk of placental abruption, growth problems, and preterm birth. Pre-eclampsia results in decreased amniotic fluid (oligohydramnios), leading to cord compression and decreased oxygen supply to the fetus.
- Bloating: Elevated progesterone levels during pregnancy relax smooth muscles, slow digestion, and lead to bloating and constipation. The expanding uterus further adds pressure on the intestines, exacerbating discomfort. However, bloating accompanied by severe pain indicates complications such as pre-eclampsia, and medical attention must be sought. Hormonal changes during pregnancy lead to physical effects, such as darker patches of skin on the face and body.
- Constipation: Constipation, characterized by difficulty or pain when passing stool, affects up to 38% of pregnant women. The increase in progesterone levels during pregnancy slows gut movement, leading to less frequent bowel movements and harder stools. Severe constipation leads to complications like fecal impaction, abdominal pain, rectal bleeding, and even rectal prolapse. Physical demands like carrying extra weight for nine months and abdominal pain due to strained ligaments are common at 24 weeks.
- Stillbirth: Miscarriage refers to pregnancy loss before 20 weeks, while losses after 20 weeks are termed stillbirths. Key factors contributing to miscarriage include fetal abnormalities (chromosome issues), maternal health problems (incompetent cervix, hormonal imbalances, chronic conditions), and infections (bacterial). Although the likelihood of miscarriage decreases as pregnancy progresses, babies born at 24 weeks have a higher chance of survival but are still at risk for disabilities like cognitive or sensory impairments.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) is a type of diabetes that develops during pregnancy, leading to elevated blood sugar levels. GDM typically starts between 24 and 32 weeks and increases maternal risks for conditions such as gestational hypertension, pre-eclampsia, cesarean section, and delivery complications. The mother and child face an increased risk of developing type 2 diabetes and cardiovascular problems later in life. Poor control of blood sugar increases the risk of birth complications.
- Anemia: Anemia is a condition characterized by insufficient hemoglobin, the protein that carries oxygen in the blood. During pregnancy, the body’s need for iron increases to support the expanded blood volume and fetal growth. Iron deficiency during this time is likely to lead to low birth weight, preterm birth, and long-term cognitive issues in the baby, such as impaired memory and learning abilities. Anemia at 24 weeks is often caused by the dilution of blood due to the increased volume, requiring careful monitoring and treatment as a midwife recommends.
- Placenta Previa: Placenta previa is a condition where the placenta is located near or over the cervix, leading to usually painless bleeding as the lower uterine segment (LUS) and cervix develop. The risk of major bleeding increases with a low-lying placenta. In cases of significant bleeding, an emergency cesarean delivery is often required to ensure the safety of the mother and baby. Prolonged complications from placenta previa after 41 weeks reduce the effectiveness of the placenta, decreasing amniotic fluid and increasing the risk of oxygen deprivation for the baby.
- Preterm Premature Rupture of Membranes (PPROM): Preterm Premature Rupture of Membranes occurs when the amniotic sac breaks before 37 weeks of pregnancy. Babies face higher risks of respiratory distress syndrome, sepsis, and brain hemorrhages when PPROM happens before 24 weeks. Common maternal risks associated with PPROM include infection in the amniotic sac and emergency C-sections. Monitoring by an OBGYN and timely interventions improve maternal and fetal outcomes.
How can a Partner Support the Mother at 24 Weeks Pregnant?
Partners can support the mother at 24 weeks pregnant with lifestyle changes, emotional support, and physical support. Below are 6 ways partners can support a 24-week pregnant mother.
- Lifestyle Changes: Encourage and participate in healthy habits together, such as avoiding smoking and adopting a balanced diet, to positively influence the mother’s well-being and support the baby’s healthy growth. Ensure that smoking happens outside the home or consider joining a quit program to protect the health of the mother and baby.
- Emotional Support: Support your partner by actively listening, showing affection, empathy, and understanding, and being present during stressful times. Asking how to best support them and offering consistent emotional support is key. Celebrating milestones like reaching 24 weeks likely helps reduce prenatal anxiety and strengthens your relationship. Affectionate gestures like holding hands and giving hugs help foster emotional well-being.
- Physical Support: Take on household chores, grocery shopping, and meal preparation to relieve your partner of daily burdens. Assist with heavy lifting, cleaning, and other physical work to make life easier for the pregnant woman. Engage in stress-relief activities, such as gentle exercises, to reduce anxiety and contribute to a positive pregnancy experience. Attending doctor’s appointments or childbirth classes together enhances support and connection.
- Physical Affection: Plan date nights and show affection through small gestures of intimacy. These acts of affection reduce partner stress and anxiety, encourage relaxation, and enhance emotional security. Acts like holding hands or planning date nights promote well-being. Encouraging your partner to rest or take naps provides much-needed relaxation.
- Open Communication: Engage in open dialogue with your partner by sharing your fears, concerns, needs, and insecurities while actively listening to theirs. Open communication deepens mutual understanding and fosters trust, helping partners navigate pregnancy’s physical and emotional changes. Encouraging your partner to communicate with their midwife about baby movement changes ensures that you stay informed and proactive about health concerns. This approach strengthens your bond and helps you feel more supported and connected throughout this journey.
- Mental Support: Offer your partner mental security by being present and maintaining a stable, safe environment. Consistent support significantly reduces maternal distress during pregnancy, helping your partner feel more secure and confident. Partners play a crucial role in empowering the pregnant woman, helping her deal with the challenges of pregnancy, and contributing to improved health outcomes for mother and baby.
What Prenatal Tests Are Needed At 24 Weeks Pregnant?
Prenatal tests needed at 24 weeks pregnant include a glucose challenge test (GTT), blood test, blood pressure measurement, urine test, and weight check. The list of tests needed at 24 weeks pregnant is below.
- Glucose Challenge Test (GTT): Gestational diabetes is a condition that tends to develop during pregnancy. GTT measures blood sugar level and is usually performed between 24 and 28 weeks. The test is done earlier for pregnant women with risk factors of developing gestational diabetes. You drink a sugary liquid in GTT, and your blood sugar levels are tested after an hour.
- Weight Check: Monitoring your weight gain to ensure it’s within healthy limits for your pregnancy. In some cases, abnormal weight gain tends to indicate underlying issues such as gestational diabetes or preeclampsia, so it’s closely watched during routine checkups.
- Blood Test: A complete blood count (CBC) is often performed during week 24 to check for iron deficiency (anemia) and ensure the mother has sufficient iron to support her pregnancy.
- Blood Pressure: Monitoring for signs of preeclampsia.
- Urine Test: Checking for proteins (which sometimes indicates preeclampsia) and signs of infection.
- Ultrasound (if needed): A follow-up ultrasound is done if the 20-week anatomy scan was not completed or if there are concerns about your baby’s development. Nuchal translucency screening measures the fetus’s neck thickness and screens for chromosomal and neural tube defects.
Tests that check the blood, urine, and fluid samples are part of routine prenatal care to detect conditions that increase the risk of complications and ensure your pregnancy is progressing healthily. Additional tests are recommended, such as the RPR test, to screen for syphilis, STI tests, or bacterial vaginosis tests if you have any specific medical conditions. Screening tests are commonly performed in the second trimester. A depression screening is sometimes done to evaluate maternal mental health at week 24. Your healthcare provider will explain the reasons for screening tests, risks, and benefits to help you understand their importance and your results.
Should You Be Admitted As Early As 24 Weeks If You’re Having Signs Of Preterm Labor?
Yes, you should be admitted as early as 24 weeks if you experience signs of preterm labor. Preterm labor is defined as labor occurring before 37 weeks of gestation. Deliveries done at 24-27 weeks demonstrated a 77% chance of complications, according to a 2014 study from the Netherlands titled “Preterm labor: current pharmacotherapy options for tocolysis,” by Ben W. Mol et al., published in the Expert Opinion on Pharmacotherapy.
Early medical attention is crucial if signs of preterm labor occur at 24 weeks. Symptoms like regular contractions, pelvic pressure, and changes in vaginal discharge need prompt evaluation. Early diagnosis enables healthcare providers to assess symptoms and administer treatments to delay labor and allow the baby’s lungs time to mature.
When To Call For Your Doctor If Something Feels Wrong At Week 24 Of Pregnancy?
- Decreased Fetal Movement: Unusual changes in your baby’s movement call for immediate attention. A noticeable decrease in fetal movement in the twenty-fourth week sometimes signals complications, such as fetal growth restriction or stillbirth. Monitor your baby’s movements daily, and call your OBGYN or healthcare provider if you observe fewer than ten movements in an hour.
- Vaginal Bleeding: Vaginal bleeding occurs in approximately 25% of pregnancies and indicates potential issues such as preterm labor. The risk of preterm labor increases threefold with vaginal bleeding. Contact your OBGYN immediately if bleeding is more than spotting or lasts longer than 2 days.
- Excessive Vomiting: Excessive vomiting often indicates a condition called hyperemesis gravidarum, which leads to dehydration and weight loss. Even less severe vomiting is associated with a higher risk of having a low birth weight baby (less than 2.5 kg), according to a 2018 study from the UK titled “Vomiting in pregnancy is associated with a higher risk of low birth weight: a cohort study,” conducted by Ken K. Ong et al. at Cambridge Biomedical Campus and published in BMC Pregnancy and Childbirth. Reach out to your OBGYN if you notice you are vomiting frequently or are unable to keep food or fluids down.
- Sudden or Extreme Swelling: Sudden, severe swelling is often a symptom of preeclampsia, a hypertensive disorder developing after 20 weeks of gestation. Call your OBGYN immediately if you notice sudden or extreme puffiness and swelling in your hands, feet, or face, especially if accompanied by symptoms like headaches and vision changes. Severe or persistent swelling typically indicates a more serious issue.
What are the 24 weeks pregnant symptoms not to ignore? 24 weeks pregnant symptoms not to ignore include decreased fetal movement, heavy vaginal bleeding, excessive vomiting, and extreme swelling. Always trust your instincts during pregnancy. If something feels off at week twenty-four, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins That Need to be Taken during Week 24 of Pregnancy?
Yes, essential prenatal vitamins need to be taken during week 24 of pregnancy to support healthy pregnancy and fetal development. The American College of Obstetricians and Gynecologists (ACOG) emphasizes the importance of vitamins and minerals during pregnancy. ACOG guides obstetrics and gynecology and recommends the following nutrients based on thorough research.
Calcium, recommended at 1,000 milligrams, is vital for strong bones and teeth in both mother and baby. Iron, needed at 27 milligrams, supports red blood cell production and prevents anemia. Iodine, at 220 micrograms, ensures proper thyroid function and brain development, while choline, at 450 milligrams, aids brain and spinal cord development.
Vitamin A, at 770 micrograms, supports eye, skin, and organ development but should be consumed in moderation to avoid toxicity. Vitamin C, at 85 milligrams, boosts immunity and enhances iron absorption. Vitamin D, at 600 international units, aids in bone development, while vitamin B6, at 1.9 milligrams, supports red blood cell formation and relieves nausea. Vitamin B12, at 2.6 micrograms, is crucial for nervous system development, and folic acid, at 400 micrograms, prevents neural tube defects.
These essential nutrients are typically included in a high-quality prenatal vitamin. Take only the recommended dosage of each nutrient to avoid complications, as overconsumption of certain vitamins, like vitamin A, leads to birth defects. Maintaining a balanced diet rich in fruits, vegetables, lean proteins, and whole grains alongside prenatal vitamins is crucial to support the health of mother and baby.
What Does Parenting Styles Suggest About 24 Weeks Pregnant?
Parenting Styles suggests expecting mothers start packing their hospital bags early. Packing your hospital bag early is a weight off your shoulders.
“Having your hospital bag ready well in advice so you’re not scrambling when the moment comes. I remember feeling so much more at ease knowing everything was packed and ready to go—it’s one less thing to worry about,” advises Pamela Li, writer, Founder, and Editor-in-Chief of Parenting Styles.
Congratulations on being 24 weeks pregnant!