25 Weeks Pregnant Symptoms: Week 25 Of Pregnancy & Prenatal Care
25 weeks pregnant symptoms involve physiological and psychological changes, including an increase in urination frequency and urgency, and forgetfulness. Other 25 weeks pregnancy symptoms are stress, lower blood pressure, backache, fatigue, insomnia, and stretch marks. Stress affects approximately 25% of pregnant women, driven by hormonal fluctuations such as increased cortisol and the pregnancy experience, negatively impacting the mother and fetus. Blood pressure tends to drop, leading to lightheadedness or dizziness due to the action of hormones like progesterone. Physical discomfort, including lower back pain, affects up to 90% of pregnant women as the baby grows. Fatigue becomes widespread, with 94.2% of pregnant women reporting exhaustion due to hormonal and physical demands, according to a 2021 study from Iran, titled “Fatigue and sleep quality in different trimesters of pregnancy,” conducted by Fatemeh Effati-Daryani et al. at Urmia University of Medical Sciences and published in Sleep Science.
Symptoms such as stretch marks, which appear between weeks 24 and 35, and constipation, experienced by 38% of pregnant women, arise from reduced intestinal motility linked to increased progesterone. Acid reflux worsens as pregnancy progresses, affecting up to 80% of pregnant women and further disrupting sleep. Braxton Hicks contractions, irregular and non-painful, become more noticeable during this period.

Fetal development at 25 weeks includes a weight of approximately 778 grams and the continued formation of critical structures such as neural circuits, sensory pathways, and fat tissue. These developments are essential for processing sensory information and regulating body temperature after birth. Ongoing prenatal care and symptom monitoring are important. Decreased fetal movements, persistent pain, or bleeding tend to indicate complications and require medical attention from your doctor or obstetrician. Balanced nutrition and safe physical activities like walking help manage symptoms and promote well-being.
What is 25 weeks pregnant in months?
25 weeks pregnant is 6 months and 1 week within the second trimester of pregnancy. You are in the first week of the seventh month of pregnancy.
What Are The Pregnancy Symptoms During 25 Weeks Pregnant?
25 weeks pregnancy symptoms include an increase in urination frequency and urgency, backache, forgetfulness, stress, lower blood pressure, fatigue, insomnia, and stretch marks. Below are common 25 weeks pregnant symptoms.
- Frequent Urination: Increased urinary frequency is characterized by the need to urinate more often and is usually accompanied by urgency (the feeling of needing to urinate immediately). Several factors contribute to frequent urination during pregnancy, including low levels of the reproductive hormone relaxin, pressure on the bladder from the enlarged uterus, reduced collagen strength, increased fluid and urine production, and changes in bladder capacity and sensitivity. Urinary frequency begins in early pregnancy and affects up to 95% of women.
- Lower Back Pain (Pelvic Girdle Pain or Lumbar Pain): Low back pain (LBP) is characterized by sharp, shooting pain, dull, aching pain, or pain radiating into the buttocks or legs. LBP can begin as early as the first trimester and often worsens as pregnancy progresses. The prevalence of LBP in pregnant women ranges from 25% to 90%. Most studies estimate that 50% of pregnant women experience LBP at some point during pregnancy or the postpartum period.
- Mom Brain (Forgetfulness): 25-week pregnant mothers often have a “pregnancy brain” or “baby brain.” Pregnancy brain refers to the subjective decline in cognition in up to 81% of pregnant women. Forgetfulness, reading difficulties, confusion, disorientation, poor concentration, increased absent-mindedness, and reduced motor coordination are manifestations of slowed cognition during pregnancy. Forgetfulness has significant real-world consequences, including impaired conversational fluency at work, frequent forgetting of appointments, and difficulties with reading comprehension, according to a 2018 study from Australia titled “Cognitive impairment during pregnancy: a meta-analysis,” conducted by Helen Skouteris et al. at Deakin University and published in Medical Journal of Australia (MJA).
- Stress: Stress is caused by various psychological, biomedical, environmental, psychosocial, and socioeconomic factors. Pregnancy presents unique changes leading to stress, such as increased cortisol levels. Higher cortisol levels negatively affect placental cortisol production and lead to adverse fetal outcomes. Around 25% of pregnant women experience prenatal stress overall. Prenatal stress is associated with an increased risk of cigarette smoking during pregnancy and depression (prenatal and postpartum). Maternal stress during pregnancy is linked to poorer obstetric outcomes, including low infant birth weight, shorter length of gestation, and an increased risk of preterm labor or birth.
- Drop in Blood Pressure: Hormones like progesterone, nitric oxide, endothelin, and estrogen dilate the blood vessels and decrease vascular resistance, reducing blood pressure during pregnancy. Decreased vascular resistance helps improve circulation in the placenta to support the growing fetus, and the blood pressure drop reduces the heart’s workload. Diastolic blood pressure starts decreasing from the first trimester, reaching the lowest point between weeks 24-26 of pregnancy, right around week 25.
- Fatigue (Tiredness): Fatigue is characterized by an overwhelming, sustained sense of exhaustion and a decreased capacity for physical and mental work interfering with daily living activities. Women experience higher levels of fatigue during the first trimester of pregnancy, which normally subsides during the second trimester. Hormonal changes, increased metabolic demands, and psychosocial factors such as stress and depression influence fatigue during pregnancy. Around 94.2% of pregnant women experience fatigue during pregnancy. Decreased ability to restore sleep often leads to preterm labor, prolonged labor, and postpartum depression.
- Insomnia: Women typically experience a decrease in total nighttime sleep during the second trimester of pregnancy compared to the first trimester. Insomnia is prevalent in all three trimesters, and women with pre-existing insomnia frequently have worse symptoms during pregnancy. Women in the second trimester often report interrupted sleep due to nighttime gastroesophageal reflux disease (GERD). Insomnia affected 30.3% of the participants in one study during the second trimester of pregnancy, including week 25.
- Stretch Marks: Stretch marks are pink, purple, or reddish streaks on the abdomen, breasts, thighs, and buttocks. Stretch marks are caused by the rapid stretching of the skin during pregnancy, which damages the underlying connective tissue. Stretch marks are common in pregnancy, affecting up to 90% of women. One study found, among the study cohort, that stretch marks appeared most frequently between weeks 24 and 35 of pregnancy. Stretch marks pose no health risks to the mother or baby, though they often cause cosmetic concerns for the mother.
- Constipation: Constipation is characterized by infrequent bowel movements and difficulty passing stool. Increased levels of progesterone during pregnancy inhibit intestinal smooth muscle motility, leading to hardening of the stool, which is most likely to develop in the first two trimesters. Pregnant mothers with constipation experience discomfort, pain, and straining. The prevalence of functional constipation in the first and second trimesters is between 35% and 39%, affecting up to 38% of pregnancies.
- Acid Reflux: Gastroesophageal reflux disease (GERD) occurs when stomach acid flows back up into the esophagus, causing heartburn (a burning sensation in the chest). GERD is caused by a decrease in the pressure of the lower esophageal sphincter (LES), which usually helps keep stomach acid flowing back up. GERD symptoms begin late in the first trimester or during the second trimester, often worsening as the pregnancy progresses and affecting up to 80% of pregnant women.
- Braxton Hicks: Braxton Hicks contractions are called “false labor” contractions, mimicking actual labor but not leading to childbirth. False labor pains are described as irregular, unpredictable contractions resembling the feeling of mild menstrual cramps or a tightening in the abdomen. However, Braxton Hicks contractions do not cause cervix dilation and are typically painless. Braxton Hicks contractions start around 6 weeks gestation but are often not felt until the second or third trimester.
- Skin Pigmentation: Hyperpigmentation is a darkening of the skin and is the most common alteration in pigmentation during pregnancy, affecting up to 90% of pregnant women. Skin pigmentation in pregnancy is attributed to increased levels of melanocyte-stimulating hormone (MSH), estrogen, and progesterone. Hyperpigmentation typically occurs in areas like the nipples, areola, and genitals. Linea nigra is a dark line running down the abdomen, normally appearing in the second trimester. Chloasma or melasma (the “mask of pregnancy”) is a patchy brown discoloration on the face affecting between 45-75% of pregnant women.
- Body Aches and Pains: Body aches and pains during pregnancy are characterized by muscle and joint soreness. Body aches are caused by hormonal changes, leading to increased weight, joint laxity, and physical demands on the body. The changing center of gravity stresses the back and hips, and the growing uterus compresses nerves and blood vessels. Body aches and pains occur at any time during pregnancy, with around 70% of women experiencing lower back pain and 32% experiencing hip pain during pregnancy.
- Swollen Ankles (Edema): Edema often manifests as swelling in the feet, ankles, or the entire leg. Increased blood volume, higher body weight, hormonal shifts, water and sodium retention, and pressure on the inferior vena cava cause lower limb edema during pregnancy. Pregnant women experiencing edema feel heaviness and pain or a bursting sensation in the legs. Symptoms of edema are more common in women who do not engage in regular physical activity. Lower limb edema occurs as early as the first trimester but is more prevalent in the second and third trimesters, affecting an estimated 50% to 80% of pregnant women.
- Hemorrhoids (Piles): Hemorrhoids are varicose veins of the rectum covered by mucosa in the anal canal. The expanding uterus increases abdominal pressure in the second trimester, which places mechanical stress on the rectum and major veins, causing venous dilation and engorgement in the anal region. The prevalence of hemorrhoids during pregnancy is as high as 40%, often accompanied by bleeding, pain, and itching.
- Indigestion: Digestion problem comes from fullness, discomfort, or pain in the stomach area associated with gastroesophageal reflux disease (GERD). GERD symptoms often begin in the first three months of gestation and persist until delivery, affecting 80% of pregnant women. Indigestion, like other GERD symptoms, is more common during pregnancy due to a decrease in lower esophageal sphincter pressure caused by progesterone.
- Thicker Hair: Thicker hair growth (hirsutism) is attributed to a prolonged anagen phase (period of hair growth in the hair cycle) caused by increased estrogen and androgen levels. Thicker hair growth is most pronounced on the face (upper lip, chin, and cheeks), but the arms, legs, back, and suprapubic areas are commonly affected. Thicker hair is not considered a pathological change, and most hairs disappear after birth.
- Itching: Pregnancy hormones cause increased skin sensitivity, potentially leading to generalized itching (pruritus) without a specific rash. Pregnancy-related skin conditions, like Pruritic Urticarial Papules and Plaques of Pregnancy (PUPPP) and Prurigo of Pregnancy, are characterized by itchy rashes. Skin sensitivity conditions and itching typically emerge in the second or third trimesters. Itching causes discomfort and distress for pregnant women, affecting sleep and quality of life.
- Bleeding Gums: Gingivitis is an oral health issue characterized by inflammation of the superficial gum tissues. Gum inflammation worsens during pregnancy due to fluctuating estrogen and progesterone levels, shifts in oral bacteria, and a weakened immune response, causing the gums to become swollen, red, and more sensitive. Gingivitis affects about 60-75% of pregnant women, typically starting in the second month of pregnancy and reaching peak severity in the eighth month.
- Feeling Hot: Hot flashes are sudden chills or sweats (cold sweats). Most women who experience hot flashes during pregnancy start to experience symptoms before week 28. The onset and frequency of hot flashes vary, but episodes typically occur weekly. Around 54.5% of pregnant women reported experiencing hot flashes, but most do not find them severe or bothersome.
- Carpal Tunnel: Carpal tunnel syndrome (CTS) is a condition occurring when the median nerve running through the wrist is compressed, causing numbness, tingling, and pain in the hand and fingers, especially at night. The prevalence of CTS in pregnancy is higher than in the general population, with studies indicating 31% to 62% of pregnant women having self-reported CTS symptoms. CTS is often present in the second trimester. Factors contributing to CTS development during pregnancy include pre-pregnancy obesity, excessive gestational weight gain, a higher number of previous live births, and certain medical conditions like gestational hypertension and diabetes.
- Prurigo: Prurigo of pregnancy is a skin condition causing extreme dryness and small, red, itchy bumps (papules and nodules). Prurigo typically develops on the outside surfaces of the arms and legs and the abdomen. The skin condition affects approximately 1 in 300 pregnancies. Prurigo appears between weeks 25 and 30 of pregnancy, sometimes persisting for up to 3 months after delivery.

What is the Importance of Understanding being 25 weeks pregnant?
The importance of understanding being 25 weeks pregnant is to recognize the significant changes in the mother’s body and the critical developmental milestones the fetus undergoes.
Week 25 marks the ongoing development of critical neural structures, including the thalamocortical pathways that facilitate sensory processing and the myelination of nerve fibers that enhance signal transmission. These fetal developments contribute to the baby’s ability to respond to external stimuli, such as sounds and light, indicating progress in auditory and visual systems. Adipose tissue development, crucial for regulating the baby’s body temperature and energy reserves, accelerates during this period. Fetal movements, including blinking and the grasp reflex, are more pronounced, showcasing advanced motor development.
Understanding physiological and psychological changes during pregnancy week by week is vital for managing symptoms and promoting well-being. Common symptoms include insomnia, stress, lower back pain, and swelling, which impact daily life and require proactive management. Recognizing these symptoms enables expectant mothers to seek appropriate care, such as adjusting sleep positions, engaging in light physical activities, and implementing stress-reducing practices. Proper nutrition, hydration, and prenatal care are necessary. Complications like gestational diabetes and anemia, often screened for at 25 weeks, need to be addressed with the help of healthcare providers (OBGYN).
What to Expect at 25 weeks pregnant?
25-week pregnant mothers should expect a range of physical and emotional changes, including a growing belly and feelings of tightness and itchiness, as the skin stretches to accommodate the baby. Discomfort in the rib area is common at week 25 of pregnancy. Braxton-Hicks contractions, which are practice contractions, start to occur more frequently for some women, causing sensations of tightening in the abdomen. Fatigue and sleeping problems, such as insomnia, are common second-trimester symptoms in the 25th week. Sleeping difficulty is often caused by discomfort from the growing belly and conditions like acid reflux (GERD), which interrupts sleep. The hormone progesterone relaxes smooth muscle tissue and slows down digestion, contributing to constipation and acid reflux. Some women notice changes like thicker hair during pregnancy due to hormonal fluctuations.
Many women experience stress during pregnancy due to hormonal fluctuations and the physical changes occurring in their bodies. Elevated cortisol levels, the body’s primary stress hormone, tend to have adverse effects on the pregnancy, contributing to issues like preterm labor and lower birth weight. Stress management through relaxation techniques or support systems is essential.
Blood pressure is typically lower because hormones like progesterone and nitric oxide dilate blood vessels. This decrease in blood pressure tends to result in feelings of lightheadedness or dizziness, a condition known as hypotension. Lower back pain and pelvic discomfort tend to become more pronounced as the baby’s weight increases, putting pressure on the lower back and pelvis.
Fatigue reappears or persists for some women due to the physical demands of supporting a growing fetus. Some women notice stretch marks as the skin stretches to accommodate the expanding belly and breasts. These are common and appear as pink, red, or purple streaks. Tightness and itchiness of the skin often accompany these stretch marks as the body expands.
Body aches, including lower back and hip pain, are frequent as the baby grows. This happens because the expanding uterus shifts the body’s center of gravity, putting pressure on the joints, muscles, and nerves. Swelling in the ankles (edema) is noticeable due to fluid retention and increased blood volume, particularly after standing or sitting for extended periods.
Fetal development at this stage is significant. The baby is about the size of a rutabaga (or eggplant) and weighs around 778 grams (1.7 pounds). The brain is becoming more sophisticated, with sensory systems actively developing. The fetus is gaining fat, essential for regulating body temperature after birth. The baby is busy practicing breathing movements and hears and responds to external sounds, including the mother’s voice. Your fetus is often active, moving frequently in response to touch and sound. The grasp reflex is emerging, allowing the fetus to clench its hands.
Routine prenatal tests, including glucose tolerance testing for gestational diabetes, are conducted around this time. Ultrasounds are often used to assess fetal development, and tests like amniocentesis are performed if genetic screening is required. It’s essential to stay connected with healthcare providers to monitor maternal and fetal health during this critical period.
How Is The Baby Developing At 25 Weeks Pregnant?
Your 25-week fetus is about the size of a rutabaga, weighing around 778 grams (1.72 pounds). OBGYNs often measure a baby’s development through key markers like biparietal diameter (63 mm), head circumference (233 mm), abdominal circumference (208 mm), femur length (46 mm), and humerus length (42 mm) instead of using crown-rump length at this stage.
Your baby’s lungs, brain, and digestive system have formed but haven’t finished developing. The brain is completing the thalamocortical pathways, critical for processing sensory information and higher thinking. Neural circuits become more sophisticated, and synapses form in preparation for future brain activity. The myelination process, essential for efficient nerve signal transmission, continues within critical motor pathways. The fetus’ senses are awakening, with blinking movements becoming more frequent and responsive to light stimuli, indicating growing visual and motor coordination.
Adipogenesis (Fat development) is well underway, contributing to your baby’s energy reserves and helping regulate blood sugar. More hair grows on your baby’s head. Auditory development allows your baby to hear and respond to sounds, including your voice. Hair cells in the cochlea fine-tune the ability to detect frequencies, allowing voice recognition.
Your baby’s grasp reflex becomes more refined, increasing hand coordination and body awareness. The baby’s movements become more noticeable as the pregnancy continues. The skin matures with elongated hair follicles, an outer skin layer, and sweat glands. With organ maturation, your baby moves closer to life outside the womb.
How Big Is Your Baby At 25 Weeks Pregnant?
Your 25-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 25-week-old fetus is about the size of a rutabaga. The 50th percentile measurements for 25-week fetal growth are as follows: the biparietal diameter (BPD) is 63 millimeters, the head circumference (HC) is 233 millimeters, the abdominal circumference (AC) is 208 millimeters, the femur length (FL) is 46 millimeters, and the humerus length (HL) is 42 millimeters.
The 25-week-old fetus weighs 778 grams (27.44 ounces or 1.72 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
What Are The Key Developmental Milestones of Babies At 25 Weeks Pregnant?
25-week developmental milestones include neural structure and circuitry development, blinking movements, and adipose (fat) cell development. Below are six 25-week pregnant milestones of your baby.
- Neural Structure and Circuitry Development: Neural circuits develop as early as 8 weeks gestation. The thalamocortical pathways, which connect the thalamus (the brain’s relay center) to the cortex (responsible for higher-order functions), are fully established at week 25, including areas involved in processing sensory information and developing thinking skills. Synapses (the junctions between neurons) form in the subplate zone—a temporary waiting area for axons before migration to the cortical plate. Myelination, the process of insulating nerve fibers to enhance signal transmission, is ongoing at week 25, particularly within the corticospinal tract — a pathway crucial for voluntary movement. Neural development is transitional at week 25 as your baby’s brain becomes sensory-driven.
- Blinking Movements: Eye-blinking involves the fetus’s ability to open and close the eyelids. Blinking movements typically occur between 23 and 26 weeks of gestation and are well established by week 25. Studies show that external stimuli, such as light, induce fetal blinking, suggesting a developing connection between the fetus’s visual system and motor responses.
- Adipose (Fat) Cell Development: Your baby is undergoing adipogenesis—the formation and growth of fat cells, at week 25. Adipose tissue stores fat and helps manage blood sugar levels through insulin signaling. Fat development begins around week 14, and by week 25, the fetus has developed definitive fat lobules resembling fat found in newborns. Fat lobules are now filled with lipids, the building blocks of fat.
- Auditory System Development: Auditory development refers to the ability of the fetus to hear and respond to sounds. The cochlea, the organ responsible for hearing, is fully formed, and hearing begins around 23 to 25 weeks of gestation. Hair cells in the cochlea are being fine-tuned to specific frequencies at week 25, helping the cochlea convert acoustic vibrations into electrical signals, which are then transmitted to the brain, allowing the fetus to react to sounds (including the mother’s voice).
- Hands: The grasp reflex is the fetus’s automatic, involuntary response to grasping an object placed in the hand. The primitive grasp reflex starts to develop between 19 and 22 weeks of gestation and is usually present by week 25. Fetuses sometimes touch one hand with the other and cross hands, indicating a growing awareness of the body.
- Keratinization: Hair and skin keratinization is when the skin starts forming a protective outer layer. Keratinization begins at 9 weeks of gestation, with hair follicles continuing to elongate by week 25. At the same time, the skin’s outer layer is developing, and eccrine sweat glands, responsible for sweat production, start to form in the skin.

How to Know if Your Baby is Healthy During 25 Weeks Pregnant?
To know if your baby is healthy during 25 weeks pregnant, keep track of fetal movement, perform an ultrasound test, have your OBGYN listen for fetal heartbeat, and test the fetus’ response to stimuli. The 4 ways to know if your baby is healthy during the 25 weeks of pregnancy are outlined below.
- Count Fetal Movement: Some women count regular fetal movement to monitor potential problems early on, as reduced fetal movements often imply adverse fetal outcomes. Babies exhibit varying movement patterns, but regular fetal movements generally indicate a healthy baby. Decreased fetal movement (DFM), on the other hand, is linked to fetal growth restriction and other complications.
- Perform Ultrasound Test: An ultrasound uses high-frequency sound waves to assess fetal growth and anatomy by providing a clear view of your baby in the womb. At 25 weeks, a second-trimester ultrasound offers reassurance about your baby’s health and helps identify multiple pregnancies or fetal abnormalities, allowing for timely intervention if needed.
- Listen for Fetal Heartbeat: A typical fetal heart rate ranges from 120 to 160 beats per minute. A regular heartbeat is observed during an ultrasound scan at 25 weeks, indicating a healthy fetus.
- Test Fetal Response to Stimuli: Ultrasound helps observe fetal responses to the mother’s touch, voice, and other external stimuli, offering insight into the baby’s well-being. Typical fetal behaviors at 25 weeks include babies moving their hands to touch the body or crossing their arms when the mother touches her abdomen. An increased movement in response to touch and voice indicates that your baby is engaging in normal developmental behaviors.
How Does Stress Negatively Impact the Baby’s Development at Week 25 of Pregnancy?
Stress negatively impacts the baby’s development at week 25 of pregnancy by reducing fetal heart rate variability, increasing cortisol levels, and altering the fetal stress response.
Maternal stress affects neurobehavioral development by reducing the baby’s heart rate variability (HRV), according to a 1996 study from The United States, titled “Fetal Neurobehavioral Development,” by Janet A. DiPietro et al., published in Child Development. Reduced HRV affects the baby’s parasympathetic (“rest and digest”) control. The mother’s experience of psychological stress, anxiety, and trauma disrupts the baby’s brain development, often leading to poor brain connectivity, difficulties in attention regulation, and altered sound reactivity.
High levels of maternal stress lead to elevated cortisol levels, which contribute to low birth weight and increase the risk of miscarriage by 42%. Low birth weight is often associated with preterm birth and subsequent health complications. Stress-induced low birth weight has long-term effects on the baby’s health, increasing the risk of heart disease and obesity in adulthood.
Maternal stress alters the hypothalamic-pituitary-adrenal (HPA) axis; the system regulates the body’s stress response. Elevated cortisol levels cross the placenta, affecting the baby’s stress response and disrupting the immune system and gut microbiome development.
What Are The Changes In The Mother’s Body At 25 Weeks Pregnant?
Week 25 Changes in the mother’s body include growing baby bump, stretch marks, skin pigmentation, and body aches and pains. Here are the 12 changes in the mother’s body at 25 weeks pregnant.
- Stretch Marks: Pink or purplish streaks on the abdomen, breasts, thighs, and buttocks caused by skin stretching.
- Skin Pigmentation: Darkening of areas like the nipples, areola, and a line down the abdomen due to increased hormone levels.
- Body Aches and Pains: Muscle and joint soreness due to weight gain, hormonal changes, and the growing uterus compressing nerves.
- Swollen Ankles (Edema): Swelling in the legs and feet is caused by increased blood volume and blood pressure on veins.
- Hemorrhoids: Swollen veins in the rectum due to increased abdominal pressure and hormonal changes.
- Indigestion: A sense of fullness and discomfort in the stomach, often linked with acid reflux.
- Thicker Hair: Prolonged hair growth, especially on the face and body, due to increased estrogen and androgen levels.
- Itching: Generalized skin itching due to hormonal sensitivity, with some developing skin conditions like PUPPP.
- Bleeding Gums: Inflamed, sensitive gums due to hormonal changes and shifts in oral bacteria.
- Feeling Hot (Hot Flashes): Sudden episodes of chills or sweats occur in about half of pregnant women.
- Carpal Tunnel Syndrome: Numbness, tingling, and pain in the hand due to pressure on the median nerve.
- Prurigo: Small, red, itchy bumps on the arms, legs, and abdomen, appearing between weeks 25 and 30 of pregnancy.

How Big is a Pregnant Belly at 25 Weeks Pregnant?
A 25-week pregnant belly has a fundal height of around 25 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 25-week-pregnant belly measures around 25 centimeters, between 23 to 27 centimeters. The expanding uterus grows to accommodate the growing fetus. The 25-week pregnant uterus has grown enough to be palpated above the navel level.
The uterine size and growth rate are affected by several factors, such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than those with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth in the past. The 2016 World Health Organization (WHO) ANC Guidelines concluded that there was inadequate evidence of using the SFH to predict fetal health.
Is it Normal to Have Contractions at 25 Weeks Pregnant?
Yes, it is normal to have contractions at 25 weeks pregnant. Contractions starting in the second trimester are likely Braxton Hicks contractions (false labor pains), according to a 2023 study from The United States, titled “Braxton Hicks Contractions,” by Deborah A. Raines et al., published in StatPearls. Braxton Hicks contractions are a normal part of pregnancy, helping the mother’s body prepare for true labor. The contractions usually feel irregular and uncomfortable but do not cause changes in the cervix or indicate the start of labor.
However, frequent contractions indicate an increased risk of preterm birth, especially when experiencing 4 or more contractions per hour. Seek immediate medical evaluation if contractions increase in frequency or intensity or are accompanied by bleeding.
What Factors Affect a Mother’s Sleeping Pattern At 25 Weeks Pregnant?
The following 5 factors affect the mother’s sleeping pattern at 25 weeks pregnant.
- Body Aches and Pains: Discomfort and pain caused by the expanding uterus affect the sleep quality of pregnant women. Discomfort often leads to wakefulness and difficulty falling back asleep, disrupting sleep. Sleep disruption causes daytime sleepiness and fatigue, negatively impacting the mother’s overall well-being. Maternal perceived sleep quality decreased in pregnancy in one study, with 67.1% of women reporting discomfort and 35.8% citing pain as the primary cause of disturbed sleep, according to a 2012 study from New Zealand titled “A postal survey of maternal sleep in late pregnancy,” conducted by B Lynne Hutchison et al. at The University of Auckland and published in BMC Pregnancy and Childbirth.
- Overactive Bladder (Frequent Urination): Nocturia (frequent nighttime urination) is caused by pregnancy-related increases in blood volume and pressure, which compress the bladder and reduce bladder capacity. The frequent need to urinate disrupts a mother’s sleeping pattern, leading to poor sleep quality. Nocturia often begins during the first trimester and typically peaks in the third trimester. Poor sleep quality is generally reported in approximately 86% of pregnant women.
- Lower Back Pain (Lumbar Pain, Pelvic Girdle Pain, or Lumbopelvic Pain): Back pain during pregnancy is commonly associated with mechanical changes due to weight gain, which causes a shift in the woman’s center of gravity. Additional factors contributing to back pain include hormonal changes and pressure from the expanding uterus on the vena cava. Discomfort caused by back pain often disrupts sleep patterns, causing difficulty finding a comfortable sleeping position. Approximately 50% of pregnant women experience back pain, with symptoms typically beginning between the 20th and 28th week of pregnancy.
- Leg Cramps (Charley Horse): Leg cramps are intense, painful muscle contractions, while Restless Leg Syndrome (RLS) disrupts sleep due to an irresistible urge to move the legs. Leg cramps in pregnancy are caused by dehydration, electrolyte imbalances, and physical activity. Leg cramps are experienced by up to 30% of pregnant women, while 26% deal with RLS.
- Hormone Changes: The most significant hormonal changes are increasing levels of progesterone and estrogen during pregnancy. Hormonal fluctuations lead to nighttime awakenings, difficulty falling asleep, and insomnia. Insomnia is experienced by 73.5% of pregnant women, which worsens in the later weeks of pregnancy.

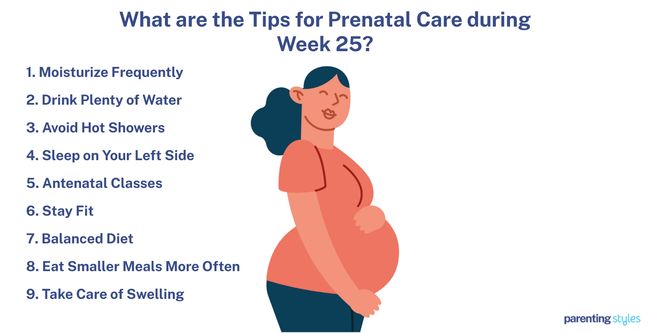
What Are The Tips For Prenatal Care During 25 Weeks Pregnant?
Here are the 9 tips for prenatal care during 25 weeks of pregnancy.
- Avoid Hot Tubs and Saunas: Avoid hot tubs and places that elevate core body temperature to protect the developing fetus.
- Avoid Lying Flat On Back (Supine Sleep Position): Avoid the supine position to prevent decreased blood flow.
- Make a Birth Plan: Antenatal classes improve knowledge and reduce anxiety about childbirth. Attend antenatal classes covering nutritional needs, safe exercises, pain relief techniques, and relaxation methods to aid labor. Attending regular prenatal classes boosts confidence, aids labor pain management, and enhances post-birth breastfeeding success.
- Do Physical Activity: Staying fit during pregnancy enhances maternal physical and psychological well-being. More energy spent on exercise is associated with better health outcomes for the mother and the baby.
- Eat Nutritious Meals: A balanced diet involves eating various foods from the five food groups. Maintain a healthy and balanced diet of essential nutrients for mother and baby. Hydrate regularly and take prenatal vitamins with folic acid to support fetal development.
- Have Small Meals: Eating smaller meals more often, such as several meals plus snacks, helps meet increased nutritional needs and lowers the risk of preterm delivery.
What Types Of Foods Are Beneficial To Eat During 25 Weeks Pregnant?
Foods beneficial to eat during the 25 weeks of pregnancy include a balanced diet, essential vitamins, and nutrients to meet the physical demands of pregnancy and support fetal development. Here are some examples of beneficial foods to include.
- Calcium: Helps build strong bones and teeth as the baby’s skeletal system develops. Try yogurt, dark green leafy vegetables, or cheese.
- Iron: Iron is Important for making red blood cells and delivering oxygen to your baby. Include lean red meat, iron-fortified cereals, or dried beans.
- Iodine: Vital for healthy brain development. Opt for eggs, dairy products, or iodized table salt.
- Choline: Supports the development of your baby’s brain and spinal cord. Consider peanuts, beef liver, or soy products.
- Vitamin A: Helps form red blood cells and supports the use of protein, fat, and carbohydrates. Enjoy carrots, green leafy vegetables, or sweet potatoes.
- Vitamin C: Promotes healthy gums, teeth, and bones. Add broccoli, tomatoes, or strawberries to your meals.
- Vitamin D: Important for bone and teeth health, healthy eyesight, and skin health. Get sunlight, and include fortified milk and salmon in your diet.
- Vitamin B6: Helps form red blood cells and process proteins, fats, and carbohydrates. Try bananas, pork, or whole-grain cereals.
- Vitamin B12: Essential for maintaining the nervous system and forming red blood cells. Include fish, poultry, or milk.
- Folic Acid (Folate): Helps prevent neural tube defects and supports the development of the fetus. Choose enriched bread, dark green leafy vegetables, or orange juice.
- Grains: Provide folic acid, fiber, iron, and B vitamins. Enjoy brown rice, quinoa, or oats. Whole grains are full of pregnancy nutrients like B vitamins and iron.
- Fruits: Offer essential vitamins, minerals, and antioxidants. Snack on fresh, dried, or frozen fruit.
- Vegetables: Rich sources of calcium, vitamin D, and protein. Include raw vegetables, frozen vegetables, or 100 percent vegetable juice. Eating five or more servings daily of fruits and vegetables is recommended.
- Protein: Important for providing iron, zinc, and omega-3 fatty acids. Opt for seafood, beans, or nuts. Try to include protein with every meal and snack.
- Dairy: Provides calcium, vitamin D, and protein. Incorporate milk, cheese, or yogurt into your diet. Increasing calcium intake is particularly important as the baby’s skeletal system develops.
Drink plenty of water to stay hydrated, take prenatal vitamins to ensure you get all the necessary nutrients, and follow the above food recommendations.
What Exercises Can You Do During 25 Weeks Pregnant?
You can do several safe and beneficial exercises during 25 weeks pregnant to support your health and your baby’s development. The 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour recommend engaging at least 150 minutes per week of moderate-intensity aerobic activities combined with muscle-strengthening exercises, including the following activities.
- Walking: A low-impact exercise that fits your daily routine easily. Walking is perfect for pregnancy. Some women carry light dumbbells during walks to enhance the benefits.
- Swimming: Provides full-body conditioning, reduces strain on your joints, and carries little risk of falling.
- Stationary Bicycling: A safer way to increase your heart rate, stationary bicycling offers the benefits of cycling without the risk of falls compared to riding a regular bike.
- Stretching: Regular stretches keep your muscles flexible and help alleviate pregnancy-related discomfort.
- Pelvic Floor Muscle Training: Exercises like Kegels strengthen the pelvic floor to reduce the risk of urinary incontinence.
Stay hydrated, avoid exercising in extreme heat or humidity, and avoid activities with a high risk of falling or injury. Always consult your OBGYN (obstetrician-gynecologist or OB-GYN) or midwife for personalized advice on exercising safely during pregnancy.
What Are The Things To Avoid At 25 Weeks Pregnant?
Here are the key things to avoid at 25 weeks pregnant to ensure your health and safety and that of your baby.
- Alcohol: Continue to avoid alcohol entirely. Consuming alcohol during pregnancy causes severe developmental issues and birth defects, including fetal alcohol spectrum disorders (FASD). Even small amounts of alcohol have adverse effects on a developing baby, according to a 2020 study titled “Alcohol Use in Pregnancy,” published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Smoking or exposure to secondhand smoke leads to severe complications like low birth weight, premature birth, and an increased risk of miscarriage, as supported by a 2020 study published in the International Journal of Environmental Research and Public Health. Move away from anyone who is smoking to avoid the risks.
- Recreational Drugs: Avoid all recreational drugs, including cannabis, which are causes of low birth weight, developmental delays, and other complications.
- Caffeine: Avoid caffeinated drinks like tea, coffee, and energy drinks, limiting your caffeine intake to 200mg daily. Excessive caffeine consumption increases the risk of miscarriage and low birth weight.
- Certain Medications and Supplements: Consult your OBGYN before taking any medications, supplements, or herbal remedies to ensure use safety during pregnancy.
- High Mercury Fish: Avoid fish high in mercury, such as swordfish, king mackerel, tilefish, and shark, as mercury harms your baby’s developing nervous system.
- Undercooked or Raw Meat: Refrain from eating undercooked or raw meat, which leads to foodborne illnesses that are particularly dangerous for pregnancy. Be aware of foods that risk infection, such as toxoplasmosis or listeriosis.
- Unwashed Vegetables and Fruits: Always wash vegetables and fruits thoroughly to reduce the risk of toxoplasmosis, a harmful parasitic infection for the baby.
- Deli Meats: Avoid deli meats unless thoroughly heated to kill harmful bacteria.
- Unpasteurized Foods: Avoid unpasteurized dairy products, soft cheeses, and other foods containing harmful bacteria.
- Exposure to Chemicals and Toxins: Limit exposure to harmful chemicals in household cleaners, pesticides, and other toxic substances.
- Hot Tubs and Saunas: Avoid hot tubs and saunas, as high temperatures sometimes negatively affect the developing baby. Avoid activities that lead to overheating, such as vigorous exercise and hot baths.
- Tight Shoes and Heavy Lifting: Avoid activities that pose risks for falls or overheating, including wearing tight shoes or engaging in heavy lifting.
- Spicy, Fatty, and Rich Foods: Try eating smaller, more frequent meals to minimize digestive discomfort.
- Lying Flat on Your Back: Get into the habit of sleeping on your left side. Lying flat on your back causes discomfort and reduces blood flow to the baby.
Avoiding the above risks carefully at 25 weeks will ensure a healthier pregnancy. Always consult with your healthcare provider for personalized advice. Contact your OBGYN or midwife immediately if you notice any unusual symptoms, such as swelling in your face or hands, or concerns about your baby’s movements.
Is it Safe to Walk Long Distances at 25 Weeks Pregnant?
Yes, it is safe to walk at 25 weeks pregnant. Walking long distances at 25 weeks pregnant aligns with WHO Guidelines on physical activity during pregnancy. The guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week, which includes walking.
Walking during pregnancy provides health benefits, including reducing the risk of gestational diabetes and excessive weight gain, according to a 2019 study from the United States titled “Walking for health during pregnancy: A literature review and considerations for future research” by Sylvia E. Badon et al., published in the Journal of Sport and Health Science. Incorporating walking into daily activities helps maintain physical activity levels during pregnancy.
Physical and psychosocial barriers make long-distance walking challenging during pregnancy. It’s important to listen to your body and adjust your walking intensity and duration according to your comfort.
Consult with your healthcare providers to ensure you follow a safe and appropriate walking regimen. Stay hydrated, avoid overexertion and excessive heat, and gradually increase walking duration to ensure the exercise remains beneficial and comfortable.
What Are The Possible Complications That Can Happen At 25 Weeks Pregnant?
The following are 5 possible complications that can happen at 25 weeks pregnant.
- Placental Abruption: Placental abruption is the premature separation of the placenta from the wall of the uterus, causing bleeding and depriving the baby of oxygen. Risk factors for placental abruption include high blood pressure, smoking, prior placental abruption, and multiple pregnancies. Signs of placental abruption include vaginal bleeding, abdominal pain, and a hard, tender uterus.
- Swelling: Edema is swelling when excess fluid builds up in the lower limbs, particularly the feet, ankles, and legs. Risk factors for edema include venous insufficiency, venous thrombosis, arterial hypertension, diabetes, and a lack of physical activity during pregnancy. Signs of edema include a feeling of heaviness in the limbs, pain, and a bursting sensation.
- Preterm Labor: Preterm labor is characterized by regular contractions before 37 weeks of pregnancy, which cause the cervix to shorten and open. Risk factors associated with preterm labor include cervical insufficiency, short cervical length, ethnicity, maternal age, and prior preterm birth, according to a 2020 study from The United States, titled “Preterm Labor and Birth,” by Kellie M Griggs et al., published in the American Journal of Maternal/Child Nursing. Signs of preterm labor include pelvic pain, vaginal discharge, back pain, menstrual-like cramps, vaginal bleeding, amniotic fluid leakage, abdominal cramping or tightening, and lower back pain or pelvic pressure.
- Hypertension: Hypertension (high blood pressure) at 25 weeks pregnant is considered early-onset preeclampsia. Preeclampsia is a serious complication characterized by high blood pressure, precisely, a blood pressure reading of 140/90 or higher. Signs of preeclampsia include swelling of the face and hands, persistent headaches, confusion, visual distortions, abdominal discomfort, nausea/vomiting in the second half of pregnancy, sudden weight gain, and shortness of breath.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) is a condition characterized by high blood sugar levels that sometimes occur during pregnancy. Risk factors for GDM include a family history of diabetes, a previous history of GDM, age over 30, obesity, and a history of polycystic ovary syndrome. Signs of GDM include increased thirst, frequent urination, increased hunger, blurry vision, and fatigue.
It is essential to note the above is not an exhaustive list, and you must consult your OBGYN for advice regarding any complications or symptoms you feel unsure about. Early diagnosis and management of severe pregnancy complications are crucial for the health of you and your baby.
How can a Partner Support the Mother at 25 Weeks Pregnant?
A partner can support the mother at 25 weeks in the following ways.
- Emotional Support: Emotional support positively affects a 25-week pregnant mother’s mental and emotional health. Listen to the mother, spend quality time together, and plan stress-reducing activities to comfort, reassure, and validate her.
- Physical Support: Demonstrate physical support by taking on household chores and helping the mother with daily tasks so that she can rest and relax.
- Shower Her with Compliments: Affirm the mother’s feelings and experiences by expressing appreciation for her changing body and reminding her of her strengths and beauty.
- Join Her Exercise Routine: Choose safe activities that are not too strenuous at 25 weeks pregnant for the mother. Spend time with the mother by participating in gentle physical activities like walking or swimming.
What Prenatal Tests Are Needed At 25 Weeks Pregnant?
Prenatal tests often needed at 25 weeks pregnant include a Complete Blood Count (CBC), Rh antibody test (if you previously tested negative), glucose tolerance testing, amniocentesis, Chorionic Villus Sampling (CVS), and an ultrasound. However, the specific prenatal tests required vary for each pregnancy, and not every woman undergoes all tests. The choice of tests depends on individual health circumstances and any particular concerns arising during the pregnancy.
A complete blood count checks for anemia or infection, while the Rh antibody test determines whether an Rh immunoglobulin shot is necessary to prevent future complications.
Testing for gestational diabetes typically takes place between 24 and 28 weeks as the mother’s insulin resistance rises, according to a 2019 study from the United States titled “The Complete Guide to Prenatal Testing,” conducted by Kiefer, A. et al. at the University of Wisconsin Hospital and published in Bloomlife. The glucose tolerance test involves drinking a glucose solution and measuring blood glucose levels after 2 hours.
Amniocentesis provides information about potential genetic conditions. Amniocentesis is a procedure where amniotic fluid is extracted from the uterus using a needle for genetic testing. Amniocentesis is most accurate in the second trimester, including week 25.
Chorionic Villus Sampling (CVS) involves collecting placental tissue for genetic testing. CVS is typically performed earlier in pregnancy and carries higher risks of complications, including miscarriage, when compared to amniocentesis.
Ultrasound is widely used among healthcare providers in pregnancy management to monitor fetal development, assess overall pregnancy health, and identify potential birth defects. Most women receive at least one ultrasound during routine obstetric care, with many undergoing additional scans as needed.
When Should You Call For The Doctor If Something Feels Wrong At 25 Weeks Pregnant?
Call your doctor if you feel something feels wrong at 25 weeks pregnant or experience any of the 6 following symptoms.
- Decreased Fetal Movement: Decreased fetal movement (DFM) at 25 weeks pregnant often indicates potential issues like growth restriction, stillbirth, preterm birth, or the need for an emergency cesarean section. Immediately inform your OBGYN if the baby moves less than average or you feel fewer movements than usual.
- Abdominal Cramping: Severe pain in the abdomen often indicates acute appendicitis, which typically arises during the second and third trimesters.
- Bleeding: Vaginal spotting/bleeding at 25 weeks pregnant significantly increases the risk of preterm delivery, low birth weight, and perinatal mortality, according to a 2013 study from Iran titled “The relationship between vaginal bleeding in the first and second trimester of pregnancy and preterm labor,” conducted by Seyedeh Hajar Sharami, M.D. et al. at Guilan University of Medical Sciences and published in Iranian Journal of Reproductive Medicine. Call your OBGYN if vaginal bleeding occurs multiple times, lasts more than 2 days, or is heavier than a menstrual period.
- Fainting (Syncope): Syncope (a brief loss of consciousness) occurs due to decreased blood volume or pressure, which decreases blood flow to the brain. Palpitations, dizziness, lightheadedness, nausea, or sweating often accompany it.
- Mood and Anxiety Disorders: Psychiatric disorders like anxiety or depression are experienced by about 14.1% of pregnant women during the second trimester. Symptoms such as excess fatigue, significant changes in appetite, or profound mood swings indicate that the condition requires professional attention.
- Vision Changes: Vision changes and headaches indicate severe conditions such as stroke or eclampsia. Red flags like neurological symptoms, high blood pressure, seizures, or fever warrant a call to your OBGYN.
What are the 25 weeks pregnant symptoms not to ignore? 25 weeks pregnant symptoms not to ignore include decreased fetal movement, abdominal pain, fainting, symptoms of mood disorder, and vision changes. Always trust your instincts during pregnancy. If something feels off at week twenty-five, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins Needed To Be Taken During 25 Weeks Pregnant?
Yes, there are essential prenatal vitamins you need to take during week 25 of pregnancy to support your health and your baby’s development. The American College of Obstetricians and Gynecologists (ACOG) emphasizes the importance of maintaining a balanced intake of vitamins throughout pregnancy, including week 25, to ensure optimal outcomes. Medical experts recommend prenatal vitamins throughout pregnancy, as prenatal vitamins help prevent birth defects and fill nutritional gaps.
- Calcium: Essential for the continued development of your baby’s bones and teeth and maintaining your bone health as your body supports the growing fetus. The recommended intake for calcium is 1,000 milligrams for adults between the ages of 19 and 50.
- Iron: Helps produce the extra blood your body needs to carry oxygen to your baby, needed at 27 milligrams. Maintaining adequate iron levels helps prevent anemia, which is often more common as pregnancy progresses.
- Iodine: At a recommended 220 micrograms, proper iodine levels ensure the effective functioning of your thyroid, supporting your baby’s neurological growth.
- Choline: Essential for the proper formation of the neural tube and ongoing brain and spinal cord development, choline is necessary at 450 milligrams.
- Vitamin A: Supports your baby’s skin, eyesight, and overall organ development at 770 micrograms. Keep your intake within recommended limits, as excessive amounts sometimes cause birth defects.
- Vitamin C: Recommended at 85 milligrams, vitamin C supports your immune system, enhances iron absorption, and contributes to the health of your skin and connective tissues, benefiting you and your baby.
- Vitamin D: Essential for calcium absorption and supporting the growth of your baby’s bones and teeth, vitamin D is required at 600 international units. Vitamin D further plays a role in maintaining your bone health.
- Vitamin B6: Needed at 1.9 milligrams, vitamin B6 helps with red blood cell formation and the metabolism of proteins, fats, and carbohydrates. Vitamin B6 helps alleviate any lingering pregnancy-related nausea and supports your baby’s brain development.
- Vitamin B12: Helps with red blood cell formation and maintaining your nervous system at 2.6 micrograms. Adequate B12 ensures your baby’s nervous system develops properly during week 25.
- Folic Acid: Recommended at 400 micrograms, folic acid is important for preventing neural tube defects and supporting the development of the placenta and your baby’s overall growth at 25 weeks. Folic acid remains essential throughout pregnancy but is particularly vital in the first trimester, the most critical time for the baby’s organ and central nervous system development.
A daily prenatal vitamin of essential nutrients helps meet your nutritional needs at week 25. However, it’s essential to follow your healthcare provider’s advice on supplementation and not exceed the recommended amounts to avoid potential risks. A well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins complements the intake of vitamins and minerals, supporting your health and your baby’s development.
What does Parenting Styles Suggest About 25 Weeks Pregnant?
25 weeks of pregnancy is the perfect time to focus on stress management. Your body and mind are undergoing significant changes, and keeping stress in check is key to your health and your baby’s development. Managing stress now prepares you for the incredible journey of parenthood.
Many mothers manage stress effectively while dealing with the symptoms of being 25 weeks pregnant. Parenting Styles suggests relaxation exercises such as taking slow, deep breaths and practicing mindfulness.
“Make it a priority to take care of yourself. Calm and confident parenting starts before the baby is born,” says Pamela Li, writer and Founder and Editor-in-Chief of Parenting Styles. “Healthy habits you build now support you throughout the rest of your pregnancy and beyond.”
Engage in activities that bring you joy, connect with your support system, and remember—this is a beautiful time for you and your baby!
Congratulations on being 25 weeks pregnant!