26 Weeks Pregnant Symptoms: Week 26 Of Pregnancy And Prenatal Care
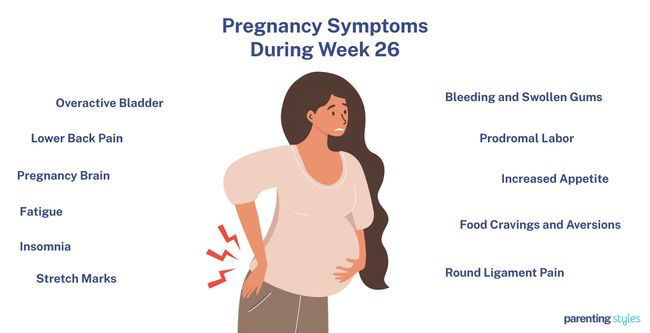
26 weeks pregnant symptoms include frequent micturition (urination), low back pain, forgetfulness (pregnancy brain), fatigue, insomnia, stretch marks, swollen gum, prodromal labor, and increased appetite. 26 weeks pregnancy symptoms that tend to worsen include tiredness, difficulty sleeping, stretch marks, and swollen and bleeding gums. Other symptoms at week 26 involve swollen ankles, stretch marks, headaches, Braxton-Hicks contractions, higher blood pressure, weight gain, an outie belly button, dry and itchy eyes, slight breast colostrum, stress, and anxiety.
Week 26 Pregnancy symptoms, while uncomfortable, are typical and often subside after childbirth. Many mothers experience increased appetite, food cravings, and aversions. Edema, leg cramps, heartburn, and constipation are prevalent due to hormonal shifts and the growing fetus putting pressure on the digestive system and circulatory systems.

The baby continues significant development at 26 weeks. The fetus’ brain activity intensifies, enabling more coordinated fetal movements and REM sleep, which is essential for brain maturation, according to a 2017 study titled “Eye movement activity in normal human fetuses between 24 and 39 weeks of gestation” by Yukuo Konishi et al., published in PLOS One.
The baby responds to external stimuli, such as sounds, with movements and heart rate changes. Lung development is progressing and preparing for breathing post-birth. The baby’s size at this stage is comparable to a scallion, weighing about 2 pounds, with measurements such as head circumference and femur length providing growth indicators.
Prenatal care at 26 weeks involves monitoring fetal movements, maintaining a healthy diet, staying hydrated, and attending regular check-ups. It’s crucial to track symptoms like sudden swelling, decreased fetal movements, and severe abdominal pain, which sometimes indicate complications like preeclampsia or preterm labor. Maintaining a regular sleep schedule, using a body pillow, and engaging in light exercises like walking or swimming improve sleep quality and manage physical discomforts.
The key to a healthy pregnancy during week 26 is monitoring physical symptoms, supporting the baby’s development through rest, nutrition, and hydration, and seeking medical advice when necessary to address any concerns.
What is 26 weeks pregnant in months? 26 weeks pregnant is 6 months and 2 weeks within the second trimester of pregnancy. You are in the middle of the seventh month of pregnancy.
What Are The Pregnancy Symptoms During Week 26?
26 weeks pregnant symptoms include frequent urination, lower backache, forgetfulness, fatigue, insomnia, stretch marks, swollen gum, prodromal labor, and increased appetite. Below are common 26 weeks pregnancy symptoms.
- Overactive Bladder (Frequent Urination): Many mothers experience an overactive bladder at week 26. This condition involves frequent urination, often accompanied by a sudden, urgent need to go, even at night. For some women, this symptom persists throughout pregnancy but usually subsides after childbirth.
- Lower Back Pain (Pelvic Girdle and Lumbar Pain): Lower back pain is prevalent during pregnancy, especially at 26 weeks. The pain often stems from the pelvic girdle or lumbar region, limiting physical activity or disrupting social interactions. Many women continue to experience discomfort even after giving birth.
- Pregnancy Brain (Forgetfulness): Often referred to as “baby brain,” cognitive declines, such as forgetfulness, confusion, and difficulty concentrating, are common during pregnancy. Forgetfulness impacts daily life, causing challenges at work or with routine tasks.
- Fatigue: Fatigue remains a common symptom during the second trimester, including at 26 weeks. This tiredness impacts both physical and mental energy levels, making daily activities more exhausting.
- Insomnia (Difficulty Sleeping): Difficulty sleeping is a common complaint at 26 weeks due to factors like nocturnal gastroesophageal reflux and frequent nighttime awakenings. Sleep disruption often continues into the postpartum period.
- Stretch Marks (Striae Gravidarum): Many women notice stretch marks at this stage. These marks, which often start as pink or purple and later become white and shiny, are sometimes itchy and uncomfortable.
- Bleeding and Swollen Gums: Some pregnant mothers experience swollen, bleeding gums at 26 weeks due to hormonal changes. Swollen gum growths, known as pyogenic granulomas or pregnancy tumors, usually resolve after birth.
- Prodromal Labor (Braxton-Hicks Contractions): Sporadic contractions, called Braxton-Hicks contractions, are common at 26 weeks. These “false labor” pains are your body’s way of preparing for childbirth, although they are typically not painful.
- Increased Appetite: Your appetite at 26 weeks likely increases as your body requires more energy to support the growing fetus. Hormonal changes, particularly rising progesterone levels, contribute to this heightened hunger.
- Food Cravings and Aversions: Cravings for certain foods, particularly sweets and high-calorie items, often intensify during the second trimester. Some women experience aversions to specific foods, especially proteins.
- Round Ligament Pain: Round ligament pain becomes more noticeable as your belly grows. The pain is often felt in the lower abdomen and groin, is typically triggered by movement ,and is more common in women who have had multiple pregnancies.
- Leg Cramps: Many women experience leg cramps at 26 weeks, especially at night. These painful muscle spasms disrupt sleep and contribute to daytime fatigue.
- Constipation: Constipation, characterized by infrequent and difficult bowel movements, is common at 26 weeks due to hormonal changes that slow gut motility.
- Heartburn (Gastroesophageal Reflux): Heartburn often intensifies in the second trimester as the growing baby puts pressure on the stomach, causing acid to flow back into the esophagus.
- Hemorrhoids: Hemorrhoids, or swollen veins in the rectum and anus, cause discomfort, itching, and pain during the second and third trimesters due to increased abdominal pressure.
- Headaches: Headaches persist at 26 weeks for some women, sometimes signaling more serious conditions like preeclampsia. While headaches usually subside later in pregnancy, severe headaches must be monitored.
- Vision Changes: Some women experience changes in their vision around this time, particularly a temporary increase in nearsightedness due to hormonal shifts that affect the cornea.
- Breast Changes: Your breasts feel fuller and more tender by the 26th week as the organs prepare for breastfeeding. Colostrum leakage is common.
- Edema (Swelling in the Ankles and Feet): Swelling in the lower extremities often worsens as pregnancy progresses. This fluid retention is caused by increased pressure on blood vessels and leads to discomfort.
- Drop in Blood Pressure and Anemia: Blood pressure tends to drop at week 26 due to hormonal changes that dilate blood vessels. Pregnancy-related anemia occurs as your body adjusts to increased blood volume.
- Hot Flashes: Many women report experiencing hot flashes around 26 weeks due to fluctuating hormone levels. These episodes often resemble those experienced during menopause.
Here are the studies and research on common week 26 pregnancy symptoms.
| Week 26 Pregnancy Symptoms | Description | Studies |
|---|---|---|
| Overactive Bladder (Increased Urination) | Overactive bladder syndrome (OAB) is a common urogenital issue during week 26, marked by frequent, urgent urination and often accompanied by urinary incontinence, which typically improves after childbirth. | According to a 2006 study from The Netherlands, titled “How Do the Prevalences of Urogenital Symptoms Change During Pregnancy?,” by H. Jorien van Brummen et al, published in Neurourology and Urodynamics: Official Journal of the International Continence Society. |
| Lower Back Pain (Pelvic Girdle Pain or Lumbar Pain) | Lower back pain during pregnancy often manifests as pelvic girdle pain (PGP) or lumbar pain (LP), with PGP being more common, characterized by deep, stabbing discomfort that limits physical activity and social interaction. | According to a 2006 study from The Netherlands, titled “How Do the Prevalences of Urogenital Symptoms Change During Pregnancy?” by H. Jorien van Brummen et al., published in Neurourology and Urodynamics: Official Journal of the International Continence Society. |
| Pregnancy Brain (Forgetfulness) | Many 26-week pregnant women experience “pregnancy brain,” which includes forgetfulness, confusion, and poor concentration. | A 2011 study from Greece, titled “Pregnancy-related low back pain,” was conducted by Kalliopi Alpantaki et al. at the University of Crete and published in Hippokratia. |
| Fatigue (Tiredness) | Fatigue causes physical and mental exhaustion, reducing energy and motivation. Tiredness impairs cognitive performance, self-care, muscle endurance, and sleep restoration and affects over 96.5% of pregnant women. | According to a 2017 study from The United States, titled “Fatigue in Pregnancy,” conducted by Kwaghdoo Atsor Bossuah at Tennessee State University and published in the International Journal of Childbirth Education. |
| Insomnia (Difficulty Sleeping) | Insomnia causes difficulty sleeping and disrupts nighttime rest. Difficulty sleeping is linked to nocturnal GERD throughout pregnancy and continues for up to six months after childbirth. | According to a 2018 study from Australia, titled “Cognitive impairment during pregnancy: a meta-analysis,” conducted by Helen Skouteris et al. at Deakin University and published in the Medical Journal of Australia (MJA). According to a 2016 study, titled “Insomnia during Pregnancy: Diagnosis and Rational Interventions,” by Imran S. Khawaja et al., published in Pak J Med Sci. |
| Stretch Marks (Striae Gravidarum or SG) | Stretch marks affect up to 90% of women during the second or third trimester. Stretch marks are skin lesions that begin as pink to purple marks. Over time, SG matures into white, shiny, crinkly, swollen, or itchy streaks. | According to a 2015 study from The United States, titled “Stretch marks during pregnancy: a review of topical prevention,” conducted by Frank Wang et al. at the University of Michigan and published in the British Journal of Dermatology. |
| Bleeding and Swollen Gum (Pyogenic Granulomas or Pregnancy Tumor) | A gingival pyogenic granuloma is a fast-growing, pink to purple lump on the gum. These lesions bleed easily and cause gum sensitivity. Bleeding and swollen gum often regresses after childbirth. | According to a 2016 study from China, titled “Initial periodontal therapy for the treatment of gingival pregnancy tumor,” conducted by C.Z. Li et al. at Wuhan University and published in Genetics and Molecular Research. |
| Prodromal Labor (Braxton-Hicks Contractions) | Braxton-Hicks contractions, or false labor, are sporadic uterine contractions that start as early as six weeks of pregnancy and are prevalent in the second or third trimester. Prodromal labor symptoms are normal, mildly uncomfortable parts of pregnancy, resembling mild menstrual cramps, but they are not true labor. | According to a 2020 study from Portugal, titled “Uterine contractions clustering based on electrohysterography,” conducted by Filipa Esgalhado et al. at NOVA University Lisbon and published in Computers in Biology and Medicine. |
| Increased Appetite | Increased appetite, or hyperphagia, during pregnancy is driven by the body’s need to nourish the growing fetus and prepare for lactation. Hormonal changes, especially the rise in progesterone, significantly stimulate food intake. | According to a 2021 study from USA, titled “The Importance of Nutrition in Pregnancy and Lactation: Lifelong Consequences,” by Nicole E. Marshall et al., published in The American Journal of Obstetrics and Gynecology. |
| Food Cravings and Aversion | Food cravings often peak around Week 26 of pregnancy. Typical desires are sweets, savory foods, fruits, and dairy. Many women experience food aversion, particularly to meat and other high-protein foods. | According to a 2014 study from The United States, titled “Pickles and ice cream! Food cravings in pregnancy: hypotheses, preliminary evidence, and directions for future research,” conducted by Natalia C. Orloff et al. at University at Albany – State University of New York and published in Frontiers in Psychology. |
| Round Ligament Pain | Round ligament pain causes abdominal discomfort during pregnancy due to the stretching of the round ligament. The cramp-like pain is usually felt in the lower abdomen and groin, intensifying with movement, and is more frequent in women with multiple pregnancies. | According to a 2017 study from Japan titled “Round ligament varicosities diagnosed as inguinal hernia during pregnancy: A case report and series from two regional hospitals in Japan,” by Yuka Mine et al., published in the International Journal of Surgery Case Reports. |
| Leg Cramps | Cramping at 26 weeks pregnant is prevalent, with up to 30% of mothers experiencing leg cramps. | According to a 2009 study from the United States, “Leg Cramps and Restless Legs Syndrome During Pregnancy,” by Jennifer G. Hensley at the University of Colorado Denver and published in The Journal of Midwifery & Women’s Health. |
| Constipation | Constipation affects up to 38% of women at 26 weeks and involves infrequent, hard, and painful bowel movements due to slowed gut motility from rising progesterone levels. Severe cases lead to issues like fecal impaction or rectal bleeding. | According to a 2015 study from the UK, titled “Constipation in Pregnancy,” by Pallavi Latthe et al., published in Constipation in Pregnancy. The Obstetrician & Gynaecologist. |
| Heartburn (Gastro-Esophageal Reflux) | Heartburn (a burning sensation in the chest or throat) occurs when stomach acid flows back into the esophagus due to pressure from the growing baby. Heartburn often begins in the first trimester and worsens in the second and third trimesters, affecting many women around 26 weeks pregnant. | According to a 2014 study from Turkey, titled “Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women,” by Gulsen Eryilmaz et al., published in the Journal of Clinical Nursing. |
| Piles (Hemorrhoids) | Piles, or hemorrhoids, are swollen veins in the rectum and anus, causing bleeding, pain, itching, and irritation during the second and third trimesters. Piles are linked to increased abdominal pressure from the growing uterus and constipation. | According to a 2014 study from the United States, “Physiologic and pharmacokinetic changes in pregnancy,” conducted by Maged M. Constantine at the University of Texas Medical Branch and published in Frontiers in Pharmacology. |
| Headaches | Headaches during pregnancy cause discomfort in the head, neck, or scalp and sometimes signal serious conditions like preeclampsia after the 20th week. Headache patterns often improve later in pregnancy. | According to a 2017 study from Italy, titled “Headache and pregnancy: a systematic,” conducted by Andre Negro et al. at Sant’Andrea Hospital and published in The Journal of Headache and Pain. |
| Vision Changes | Vision changes during pregnancy, like blurred distance vision, are caused by hormonal shifts that alter the cornea’s shape and thickness. These changes typically begin in the first trimester, with 54% of women experiencing reduced distance vision in the second trimester. | According to a 2014 study from Iran, titled “Visual Acuity Changes during Pregnancy and Postpartum: A Cross-Sectional Study in Iran,” by Abolfazl Mehdizadehkashi et al., published in Journal of Pregnancy. |
| Breast Changes | Breast changes at 26 weeks include swelling, tenderness, and a feeling of fullness due to increased glandular tissue and fat in preparation for lactation. Blood flow to the mammary glands significantly increases, often leading to colostrum leakage before full milk production starts. | According to a 2009 study from Australia, titled “Ultrasound imaging of the lactating breast: methodology and application,” conducted by Donna T. Geddes at The University of Western Australia and published in the International Breastfeeding Journal. |
| Edema (Swollen Ankles and Feet) | Edema, or fluid retention, causes swelling in the ankles and feet during pregnancy due to pressure from the growing uterus on blood vessels. Swollen ankles and feet affect about 87% of pregnant women, with 44% noticing an increase in shoe size by the third trimester. | According to a 2014 study from Turkey, titled “Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women,” by Gulsen Eryilmaz et al., published in the Journal of Clinical Nursing. |
| Drop in Blood Pressure and Anemia | Pregnancy hormones cause blood vessels to relax, leading to a natural drop in blood pressure, which is at its lowest between 20 and 24 weeks, often causing hypotension by week 26. Physiologic anemia develops as plasma volume increases faster than red blood cell mass, resulting in lower hemoglobin concentration and thinner blood. | According to a 2010 study from The United States, titled “Lower Extremity Changes Experienced During Pregnancy,” conducted by Priya Ponnapula et al. at SSM DePaul Health Center, Bridgeton, MO, and published in The Journal of Foot and Ankle Surgery. |
| Hot Flashes | Hot flashes, characterized by sudden warmth and sweating, are caused by hormonal fluctuations during early pregnancy, similar to menopause. Around 62% of pregnant women experience mild, weekly hot flashes. | A 2005 study from The United States, titled “Hot flashes during pregnancy: a comparative study,” was conducted by James C. Coyne et al. at the University of Pennsylvania and published in the European Journal of Obstetrics & Gynecology and Reproductive Biology. |
What Is The Importance Of Understanding Being 26 Weeks Pregnant?
The importance of being 26 weeks pregnant is to monitor fetal development and changes in the mother’s body for the health of both the mother and the baby. The 26-week-old baby has more refined brain activity, sensory development, and continued lung maturation. The mother’s body undergoes notable changes, including increased uterine size, weight gain, and potential discomforts like back pain or swelling. Awareness of these changes helps expectant mothers monitor their health and promptly address concerns.
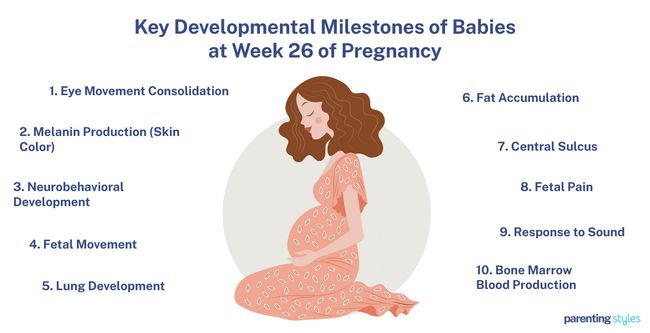
Expectant mothers notice more frequent and coordinated fetal movements during week 26 as the baby’s central nervous system and muscle development mature. The baby’s eyes become more efficient in movement, and REM sleep begins, essential for brain development. Melanin production stabilizes, influencing the baby’s skin color. Lung development reaches the canalicular stage, preparing the baby for breathing after birth, according to a 2013 study from the United Kingdom, titled “Early lung development: lifelong effect on respiratory health and disease,” conducted by Janet Stocks et al. at University College London and published in The Lancet Respiratory Medicine.
Prenatal care during the twenty-sixth week includes tracking fetal movements, attending regular prenatal appointments, and maintaining a healthy lifestyle. Staying hydrated, eating a balanced diet rich in essential vitamins and minerals, and monitoring any unusual symptoms like contractions, bleeding, or decreased fetal movements are vital for ensuring a safe pregnancy journey.
Understanding pregnancy week by week fosters proactive care, allowing the mother to better manage physical changes, support the baby’s development, and prepare for the third trimester and eventual birth.
What To Expect At 26 Weeks Pregnant?
26 weeks pregnant mothers should expect significant developments in their baby’s growth and behavior. The baby’s eyes move more efficiently with the consolidation of eye movements, which is associated with REM sleep. REM sleep is important for brain development. Eye movements become more regular by week 26, although they start as early as 14 weeks.
Melanin production stabilizes around this time. Melanin gives skin its color as the baby’s skin develops its natural pigmentation. Lung development continues in the canalicular stage, where the respiratory airways mature, and the crucial alveolar cells form. Gas exchange and surfactant production are processes essential for breathing after birth.
The baby’s brain continues to mature neurobehaviorally, with most neurons settling into place and forming early connections. The neuron connections allow the baby to begin processing sounds, including their mother’s voice. Fetal movements, like kicking and rolling, become more coordinated and noticeable to the mother, indicating a healthy central nervous system and muscle development. Fat accumulation continues, helping to prepare the baby for energy storage and temperature regulation after birth, according to a 2021 study titled “Adipose tissue development and lipid metabolism in the human fetus: The 2020 perspective focusing on maternal diabetes and obesity,” by Gernot Desoye et al., published in Progress in Lipid Research.
An important structural brain milestone is the deepening of the central sulcus, a groove that helps separate different brain regions, making advanced brain folding and development. The baby is likely able to experience rudimentary pain, as their brain has developed enough to process such stimuli at week 26.
The baby’s hearing becomes more refined in auditory development, and begin to respond more distinctly to sounds. The liver previously handled blood production. The blood production has now entirely shifted to the bone marrow, establishing a critical function for life after birth.
The uterus expands further in week 26, pushing up into the abdomen. Weight gain continues steadily, driven by the baby’s growth and the mother’s increasing blood volume and fluid retention. Many mothers notice breast enlargement due to hormonal changes, with some experiencing tenderness and sensitivity. Skin changes, including darkening of certain areas, stretch marks, and possibly varicose veins, are common during this stage due to increased hormone levels and blood flow.
Other physical changes and second-trimester symptoms include hair thickening and a slight increase in heart rate as the body works harder to support the growing baby. Swollen feet and ankles are typical due to fluid retention and increased blood vessel pressure. Vaginal discharge often increases as the body prepares for labor. Many women find their belly button becoming more prominent as the abdomen stretches.
Monitoring fetal movements, attending prenatal appointments, and maintaining a healthy diet and lifestyle are essential at this stage to ensure both mother and baby are thriving.
How Is The Baby Developing At 26 Weeks Pregnant?
Your 26-week-old baby is about the size of a scallion and weighs approximately 902 grams (around 2 pounds). Measurements, such as the biparietal diameter (66 mm), head circumference (244 mm), abdominal circumference (219 mm), femur length (48 mm), and humerus length (44 mm), offer more precise growth indicators at this stage.
Your baby’s eyes are more coordinated, and eye movement during fetal sleep is similar to REM, signaling brain development at week 26. Melanin production began earlier and has largely stabilized, contributing to your baby’s skin color.
The fetus is in the canalicular stage of lung development, where respiratory airways form and type 1 and type 2 alveolar cells differentiate, preparing the lungs for future breathing. Sensory and motor skills are advancing, with your baby responding to sounds, including your voice, as neurons establish critical synaptic connections.
Fetal movements, such as rhythmic kicks and rolling, are more distinct, reflecting the maturing central nervous system. Fat accumulation ramps up, providing your baby with energy reserves. The brain actively develops, marked by the deepening of the central sulcus, according to a 2001 study from France, titled “Fetal Brain MR Imaging,” conducted by Nadine Girard, MD et al. at Université de La Mediterranée, and published in Magnetic Resonance Imaging Clinics of North America.
Your baby’s bone marrow has become the primary producer of blood cells. There’s emerging evidence that the new blood cells are able to sense rudimentary pain. The detection and response to sounds are more refined as the ear’s structures mature, preparing your baby for the auditory world after birth.
How Big Is Your Baby At Week 26 Of Pregnancy?
A 26-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 26-week-old fetus is about the size of a scallion. The 50th percentile measurements for 26-week fetal growth are as follows: the biparietal diameter (BPD) is 66 millimeters, the head circumference (HC) is 244 millimeters, the abdominal circumference (AC) is 219 millimeters, the femur length (FL) is 48 millimeters, and the humerus length (HL) is 44 millimeters. The 26-week-old fetus weighs 902 grams (31.82 ounces or 1.99 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 26 Of Pregnancy?
The key developmental milestones of babies at week 26 of pregnancy include eye movement consolidation, melanin production, and neurobehavioral development. The 10 key developmental milestones of 26 weeks babies are below.
- Eye Movement Consolidation: Consolidation of fetal eye movements is when your baby’s eyes start working together more efficiently and consistently. Eye movements are recorded from as early as 14 weeks, and during fetal sleep, movements resembling REM indicate healthy brain development, according to a 2017 study titled “Eye movement activity in normal human fetuses between 24 and 39 weeks of gestation” by Yukuo Konishi et al., published in PLOS One. Fetal eye movements consolidate between weeks 24-26 of pregnancy and become more frequent in the coming weeks.
- Melanin Production (Skin Color): Melanin is the pigment substance that gives fetal skin its color. Melanin production in the fetal skin begins when immature melanocytes first appear in the dermis around 10-11 weeks of pregnancy, reaching the epidermis by 12 weeks. As these melanocytes multiply, the skin gradually develops noticeable pigmentation. Melanin production stabilizes by the fifth month (around 17-22 weeks), a few weeks before week 26, leading to unique variations in skin color.
- Neurobehavioral Development: Your baby starts to develop sensory and motor skills as their central nervous system matures. Most neurons have reached their final locations in the brain by weeks 26-29 and start to connect with other neurons, forming the first synaptic connections. Fetuses react to low-frequency sounds, like their mother’s voice, around week 26 and exhibit coordinated movements in response to these sounds.
- Fetal Movement: Fetal movements like rhythmic kicks and rolling motions become more pronounced and distinct at week 26. Many expectant mothers begin feeling these movements, known as quickening, as early as 14 weeks, marking the development of the central nervous system and muscle coordination. Fetal movements at 26 weeks range from general actions like arm and head movements to more complex gestures, like grasping and practicing breathing movements.
- Lung Development: The fetal lungs are in the canalicular stage of development at week 26 of pregnancy. During this stage, respiratory airways form, and epithelial cells differentiate into type 1 and type 2 alveolar cells, which are essential for gas exchange and surfactant production. The blood-gas barrier thins for more efficient oxygen and carbon dioxide exchange.
- Fat Accumulation: Your baby accumulates fat as adipocytes (fat-storing cells) build up within the body. The fetus uses glucose supplied by the mother to synthesize fatty acids, the building blocks of fat, storing this fat for growth and energy. Your baby’s adipose tissue grows between weeks 23 and 29 of pregnancy as fat lobules enlarge and the necessary blood supply and fat cells within those lobules develop.
- Central Sulcus: Human brain development involves the formation of sulci (grooves) and gyri (bumps), which separate brain regions and increase the brain’s surface area. An essential structure called the central sulcus separates the brain’s frontal and parietal lobes. The brain’s central sulcus folds and deepens at 24 weeks and, by 26 weeks, is visible on MRI, indicating active brain development.
- Fetal Pain: Fetal pain reception refers to the fetus’s ability to perceive and respond to painful stimuli. The fetal brainstem and diencephalon mature significantly from week 15 of pregnancy, allowing the fetus to manage essential functions like sensory processing and simple environmental interactions. The development of these brain structures suggests that the fetus begins to experience rudimentary pain starting at week 15, indicating that by 26 weeks of gestation, the fetus is likely capable of feeling pain.
- Response to Sound: Your baby starts to detect and respond to auditory stimuli, such as noises and voices. The major ear structures of the fetus are mostly formed by 25 weeks, laying the groundwork for auditory perception one week before now. Hair cells in the inner ear start to fine-tune their ability to recognize different sound frequencies around week 26, allowing your baby to distinguish between various sounds.
- Bone Marrow Blood Production: Bone marrow is the spongy, soft tissue inside bones that produces blood cells in adults. In early pregnancy, blood cell production begins in the yolk sac, which is taken over by the liver between weeks 6 and 22. The bone marrow becomes the primary site of blood cell production after week 22, taking over this role for the remainder of the pregnancy and beyond.
How To Know If Your Baby Is Healthy During Week 26 Of Pregnancy?
To know if your baby is healthy during week 26 of pregnancy, use the following 6 ways.
- Keep Track of Fetal Movement: Your baby moves frequently by week 26 with kicks, rolls, and stretches. Most babies establish regular movement patterns. A significant decrease in movement requires contacting your healthcare provider for evaluation.
- Perform an Ultrasound Test: Many women have already had a detailed ultrasound by week 26. An ultrasound checks the fetal anatomy and placenta position.
- Listen for Fetal Heartbeat: The fetal heart rate ranges from 120 to 160 beats per minute when you’re 26 weeks pregnant. Your doctor will use a Doppler device to listen to the heartbeat during your prenatal visit.
- Measure Amniotic Fluid Levels: An ultrasound assesses whether your amniotic fluid levels are within a normal range. Too little or too much amniotic fluid indicates a potential issue, and your OBGYN (obstetrician-gynecologist or OB-GYN) or midwife will monitor this.
- Report Suspicious Complication Symptoms: Be alert for symptoms such as severe abdominal pain, vaginal bleeding, contractions, or reduced fetal movements. Complications are less likely in the second trimester, but you must inform your OBGYN if anything feels off.
- Monitor High-Risk Pregnancy: Women who are at risk of preterm birth must contact their OBGYN if they experience signs of preterm labor, such as regular contractions or a feeling of pressure in the pelvis.
Regular prenatal check-ups help address any concerns or complications early. Speak to your OBGYN if you have concerns.
Does Your Baby’s Eyes Start To Open At 26 Weeks Pregnant?
Yes, some babies’ eyes open at 26 weeks pregnant. Most fetuses do not open their eyes until around week 28, according to a 2021 study from India, titled “Advantages of Screening for Glucose Tolerance in the Sequential Weeks of Gestation,” by N. Bhavatharani et al., published in the Journal of Social Health and Diabetes.
How Can Your Baby Respond More During Week 26 Of Pregnancy?
Your baby’s brain activity increases significantly at week 26, allowing for more pronounced responses to external stimuli. The 26th week marks the beginning of a maturation phase. The baby’s central nervous system is developing new neural connections. Such neural developments enhance the baby’s ability to respond to stimuli, such as sounds or vibrations, with movements and changes in their heart rate.
Babies often respond to vibroacoustic stimulation (VAS) by increasing their movements during week 26, according to a 2011 study from The United States, titled “Development of fetal movement between 26 and 36-weeks’ gestation in response to vibroacoustic stimulation,” by Laura Glynn et al., published in Frontiers in Psychology. This includes head movements, limb movements, and even mouthing actions. The stimulation triggers large, sometimes jerky movements, reflecting the ongoing sensorimotor development. The baby’s responses are part of the baby’s neurological maturation as the baby practices controlling the muscles and adjusting to sensory inputs.
The baby’s pulse rate increases following stimulation due to the development of the autonomic nervous system, which controls involuntary functions like heart rate. The pulse rate increase suggests that the baby is beginning to interact more with the environment, even from within the womb. The baby’s movements become smoother and more coordinated as the brain develops. The baby’s growing capacity for movement and sensory perception lays the groundwork for more complex behaviors as they approach birth.
What Are The Changes In The Mother’s Body At 26 Weeks Pregnant?
The changes in the mother’s body at 26 weeks pregnant include uterus size and position changes, weight gain, and enlarged breasts. Here are 9 key changes in the mother’s body at week 26 of pregnancy.
- Uterus Size and Position Changes: The uterus expands to allow the baby’s growth throughout pregnancy, rising higher into the abdomen and placing pressure on surrounding organs by 26 weeks. The top of the uterus, called the fundus, now sits several centimeters above the umbilicus and typically matches the week of gestation. This means your uterine height measures around 26cm at 26 weeks pregnant.
- Weight Gain: Weight gain at 26 weeks pregnant is driven by your baby’s growth and the body’s gradual storage of additional water for amniotic fluid and fetal circulation. Pregnant women with an average pre-pregnancy weight and BMI typically gain between 11.5 and 16 kg throughout pregnancy. Rapid weight gain of more than 0.5 kg per week is unusual and requires attention from a medical professional.
- Enlarged Breasts: Elevated levels of estrogen and progesterone during pregnancy often lead to breast enlargement, resulting in tenderness, increased sensitivity, and areola growth. Increased sebaceous gland activity causes small bumps on the areola, called Montgomery tubercles, to enlarge. Montgomery tubercles help prepare the mother for breastfeeding by lubricating and protecting the nipple and areola.
- Skin Changes: Pregnant women often experience skin changes due to heightened sensitivity to hormones like estrogen and progesterone, believed to stimulate melanin production. Hyperpigmentation, the darkening of the skin, is the most commonly reported skin condition in the second half of pregnancy, affecting 85-90% of pregnant women, according to a 2017 study from The United States, titled “Physiologic changes of pregnancy: A review of the literature,” by Amy Kalowitz Bieber, MD et al., published in International Journal of Women’s Dermatology. Hyperpigmentation typically affects areas like the areolas, nipples, and inner thighs. The linea nigra, a dark line running down the abdomen, are common forms of hyperpigmentation. Melasma, characterized by brown patches on the face, is more prevalent among women with darker skin tones. Increased blood flow during pregnancy causes skin changes like spider veins, varicose veins, and stretch marks on the abdomen and thighs.
- Hair Changes: Increased estrogen levels often prolong the anagen or active growth phase of hair in pregnant women. About 60% of women experience hair changes in the second trimester, with about 5.2% experiencing hirsutism (unwanted hair growth on the face and abdomen), according to a 2014 study from Turkey titled “The physiological changes in pregnancy and their distribution according to trimester,” conducted by Ayse Neslin Akkoca et al. at University Faculty of Medicine and Research Hospital and published in Journal of Gynecology and Obstetrics. Many women notice their hair is thicker by week 26, with reports of a bushier appearance, particularly in the second and third trimesters.
- Blood Volume and Heart Rate: Maternal blood volume increases during pregnancy to support the growing fetus, increasing cardiac output as more blood returns to the heart. A regular heart rate for pregnant women at 26 weeks is around 90 beats per minute, according to a 1996 study from the Netherlands, titled “A longitudinal study of maternal hemodynamics during normal pregnancy,” by A. Carla C. van Oppen et al., published in Obstetrics & Gynecology. The maternal heart rate continues to rise until term, although some women experience a decrease in cardiac output in the third trimester.
- Swollen Feet and Ankles: Swollen feet and ankles, known as edema, occur due to hormonal changes, increased blood volume, and fluid retention during pregnancy. The uterus compresses blood vessels as it grows, increasing pressure in the veins and contributing to this swelling. Around 87% of mothers reported experiencing swollen feet and ankles during pregnancy, with many even noticing an increase in shoe size, according to a 2010 study from The United States titled “Lower Extremity Changes Experienced During Pregnancy,” conducted by Priya Ponnapula et al. at SSM DePaul Health Center, Bridgeton, MO, and published in The Journal of Foot and Ankle Surgery.
- Increased Vaginal Discharge: Normal vaginal discharge is a watery, odorless fluid that usually presents during pregnancy and appears as a slight stain. Pathological discharge is typically due to infection and appears yellowish with a foul smell. Symptoms like itching, irritation, and pain generally accompany discharge from a vaginal infection. Increased vaginal discharge affects about 89% of pregnant women, according to a 2021 study titled “Vaginal discharge during pregnancy and associated adverse maternal and perinatal outcomes,” by Meharunnissa Khaskheli et al., published in Pakistan Journal of Medical Sciences.
- Protruding Navel: The expanding uterus pushing against the abdominal wall, causing the belly button, or umbilicus, to pop out or become more prominent. The protruding belly button is primarily due to the stretching and thinning of the abdominal skin and muscles as the baby grows. The navel, normally a slightly recessed scar, becomes more visible or “outie” as the pregnancy progresses. This is a common and harmless effect of the body’s physical adaptations during week 26.
How Big Is A 26 Weeks Pregnant Belly?
A 26-week pregnant belly has a fundal height of around 26 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 26-week-pregnant belly measures around 26 centimeters, between 24 to 28 centimeters. The expanding uterus grows to accommodate the growing fetus. The 26-week-pregnant uterus has grown enough to be palpated above the navel level.
The uterine’s size and growth rate are affected by factors such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, and the different sizes of the fetus. Women with higher BMI tend to have a slightly larger fundal height measurement than those with lower BMI.
The fundal height measurement was often used in clinical practice to monitor fetal growth in the past. The 2016 World Health Organization (WHO) ANC Guidelines recommended against using the SFH as an indicator of fetal health, concluding that evidence of benefits for using the SFH was inadequate.
Is Protruding Navel Common at 26 Weeks Pregnant?
Yes, a protruding navel is common at 26 weeks pregnant. The mother’s abdominal skin stretches significantly as the baby grows, often changing the appearance of the umbilicus (belly button). The pressure from the expanding abdomen causes the navel to shift from its usual inward position to a more protruding one, according to a 2018 study from Colombia, titled “Omphaloplasty: X-Shaped Flap Technique,” conducted by Alfredo Hoyos at Elysium Aesthetics and published in A Surgical Guide of the Umbilicus.
Is It Normal to Have Contractions At 26 Weeks Pregnant?
Yes, it is normal to have contractions at 26 weeks pregnant. Some women begin to experience contractions, known as Braxton-Hicks contractions, around the 20th week of pregnancy. Braxton-Hicks contractions vary in intensity and frequency, occurring irregularly every few hours or more and typically becoming stronger and more frequent as the pregnancy progresses. Braxton-Hicks are not a sign of labor, but these contractions help prepare the body for true labor by toning the uterine muscles.
Feeling contractions at this stage feels alarming, but Braxton-Hicks contractions are normal and not a cause for concern unless they become regular and painful, which sometimes indicates preterm labor. It’s essential to consult with a healthcare provider for personalized advice and reassurance regarding any concerns during pregnancy.
Is it Common to be More Forgetful at 26 Weeks Pregnant?
Yes, it is common to be more forgetful at 26 weeks pregnant. Many pregnant women report cognitive changes such as brain fog, absentmindedness, and disorientation, a phenomenon often referred to as “baby brain.” Up to 81% of women report experiencing memory issues, which tend to become more pronounced as pregnancy progresses, according to a 2018 study from Australia, titled “Cognitive impairment during pregnancy: a meta‐analysis,” by Helen Skouteris et al., published in Medical Journal of Australia.
The brain’s primary energy source is typically glucose, but during pregnancy, a significant portion of this glucose is redirected to support fetal growth and development. More glucose is allocated to ensure fetal survival as the fetus’ energy requirements increase. This glucose allocation results in an “energy trade-off” between the pregnant mother and the fetus, causing noticeable cognitive challenges for the mother, according to a 2019 study from Poland titled “Cognitive costs of reproduction: life-history trade-offs explain cognitive decline during pregnancy in women,” by Anna Ziomkiewicz et al., published in Biological Reviews.
Why does Pregnancy Insomnia Occur?
Pregnancy insomnia occurs due to factors including hormonal changes, nocturia, lower back pain, heartburn, restless leg syndrome, anxiety and stress, leg cramps, physical discomfort, and morning sickness.
Hormonal changes include the rise in progesterone levels. Progesterone relaxes muscles, including those in the digestive tract, leading to discomforts such as heartburn and indigestion, which can sometimes disrupt sleep. Hormonal fluctuations directly affect the body’s sleep-wake cycle, making it harder to maintain restful sleep.
Nocturia (frequent urination at night) often interrupts sleep. The expanding uterus presses on the bladder, causing frequent bathroom trips.
Back pain results when the growing belly strains the back muscles, making it difficult to find a comfortable sleeping position and resulting in frequent awakenings.
Hormonal changes and the pressure of the growing uterus exacerbate heartburn. Heartburn tends to worsen when lying down, making it harder to fall or stay asleep.
Restless leg syndrome (RLS), which causes an uncontrollable urge to move the legs, is another common issue that disturbs sleep. RLS is linked to iron or folate deficiencies.
Psychological factors such as anxiety and stress about the baby’s health, labor, and life changes often contribute to insomnia. Emotional fluctuations are typical during pregnancy and contribute to nighttime awakenings. Fetal movement, which becomes more noticeable as the baby grows, usually peaks at night when the mother rests.
Leg cramps, often caused by changes in circulation and pressure from the growing uterus, wake pregnant women during the night.
Other physical discomforts, such as breast tenderness caused by hormonal changes and the body’s preparations for breastfeeding, make lying on the side or stomach uncomfortable.
Persistent nausea and vomiting, even in the later stages of pregnancy, continue to disturb sleep, particularly if the symptoms intensify at night.
All of these factors combine to make restful sleep more difficult as pregnancy progresses at week 26.
What Are The Tips For Prenatal Care During Week 26?
Prenatal care tips during week 26 include attending regular OBGYN appointments, monitoring symptoms, and taking prenatal vitamins. The 8 main tips for prenatal care at the 26th week are below.
- Attend Prenatal/OBGYN Appointments: Prenatal care involves regular visits to an OBGYN to monitor maternal and fetal health. Prenatal appointments assess growth and identify potential risks early. Effective counsel during these visits educates mothers on avoiding alcohol and preventing severe conditions like fetal alcohol spectrum disorders. Prioritizing these check-ups promotes a healthy pregnancy and better outcomes for both mother and child.
- Observe Swelling: Swelling (edema) is fluid accumulation causing enlargement in the feet and legs. Edema develops due to increased venous pressure and hormonal changes. Compression therapy helps manage swelling by improving blood flow. Engaging in regular, safe physical activity enhances venous return and reduces discomfort. If swelling becomes severe or painful, consult your OBGYN to rule out serious conditions such as venous thrombosis.
- Continue Taking Prerenal Vitamins: Prenatal vitamins provide essential nutrients to support your health and the development of your fetus. Vitamins include folic acid, iron, and calcium, which are crucial for preventing birth defects and efficient oxygen delivery to the fetus. Take your prenatal vitamins to meet your nutritional needs without consuming unhealthy foods. Always check the serving size on the label to avoid exceeding the recommended dosage, as excessive vitamin A leads to birth defects.
- Track Fetal Movement: Awareness of usual fetal movement patterns helps ensure a healthy pregnancy and improves perinatal outcomes. Regularly feeling your baby move at week 26 is essential for detecting potential issues. Tracking daily fetal activity aids in maintaining a healthy pregnancy and allows for timely intervention if problems arise.
- Continue Eating a Healthy Diet: Eating a healthy diet at week 26 of pregnancy is crucial for maternal and fetal health. Focus on consuming various nutrient-dense foods, including fruits, vegetables, whole grains, legumes, nuts, seeds, and healthy fats with omega-3 fatty acids. Avoid processed foods high in sugars and unhealthy fats, as processed foods increase the risk of pregnancy complications. Refrain from restrictive diets, such as ketogenic or Paleo, which often lead to nutrient deficiencies.
- Hydrate Often: Hydrate often during pregnancy to sustain increased water needs. Insufficient hydration leads to dehydration, negatively impacting maternal health and birth outcomes. Pregnant women drink approximately 2.7-4.8 liters of water daily. Monitoring fluid intake helps maintain balance, supports various bodily functions, prevents complications like urinary tract infections, and promotes healthy fetal growth.
- Attend Childbirth Classes: Attending childbirth classes provides essential knowledge about labor and delivery. Regular class attendance significantly reduces anxiety and increases confidence in natural childbirth. Classes cover pain management, warning signs, and preparation for breastfeeding and parenting. Consistent participation in these classes at week 26 of pregnancy helps meet informational needs and fosters a supportive relationship with healthcare providers.
- Monitor Blood Pressure: High blood pressure during pregnancy leads to pre-eclampsia (sudden hypertension after 20 weeks). Regular blood pressure monitoring helps in early detection, aiming for readings under 140/90 mmHg to minimize risks. Pre-eclampsia causes strokes or growth restrictions for babies. Maintaining a healthy lifestyle with nutritious food and regular exercise supports blood pressure control.
What Types Of Foods Are Beneficial To Eat During Week 26 Of Pregnancy?
Here are 15 types of foods rich in vitamins and minerals and essential that are beneficial to eat during week 26 of pregnancy, according to the American College of Obstetricians and Gynecologists (ACOG):
| Nutrient | Benefit | Best Sources |
|---|---|---|
| Vitamin A (770 mcg) | Helps form red blood cells and helps the body use protein, fat, and carbohydrates. | Pumpkin, mustard greens, red bell peppers, dried apricots, turnip greens |
| Vitamin C (85 mg) | Promotes healthy gums, teeth, and bones. | Pineapple, raspberries, snap peas, bell peppers, strawberries |
| Vitamin D (600 IU) | Builds bones and teeth and helps promote healthy eyesight and skin. | Fortified soy milk, mackerel, canned tuna, portobello mushrooms, fortified cereals |
| Vitamin B6 (1.9 mg) | Helps form red blood cells and helps the body use protein, fat, and carbohydrates. | Avocado, tuna, sunflower seeds, walnuts, whole-grain oatmeal |
| Vitamin B12 (2.6 mcg) | Maintains the nervous system and helps form red blood cells. Supplements are recommended for vegetarians. | Yogurt, haddock, blue cheese, mackerel, sardines |
| Folic Acid (600 mcg) | Helps prevent birth defects of the brain and spine and supports general growth and development. | Lentils, split peas, romaine lettuce, beets, sunflower seeds |
| Calcium (1,000 mg) | Builds strong bones and teeth. | Cottage cheese, collard greens, bok choy, ricotta, fortified rice milk |
| Iron (27 mg) | Makes red blood cells and helps deliver oxygen to your fetus. | Lean pork, clams, trout, chickpeas, dried figs |
| Iodine (220 mcg) | Essential for healthy brain development. | Mussels, plain yogurt, baked cod, turkey, scrambled eggs |
| Choline (450 mg) | Essential for developing your fetus’s brain and spinal cord. | Chicken breast, navy beans, lentils, cauliflower, sunflower seeds |
| Grains | Sources of folic acid, fiber, iron, and B vitamins. | Millet, spelt, kamut, teff, whole-grain cornmeal |
| Fruits | Sources of vitamins and minerals, antioxidants, and fiber. | Mangos, apricots, papayas, blueberries, cantaloupes |
| Vegetables | Sources of calcium, vitamin D, and protein. | Artichokes, green beans, parsnips, leeks, red cabbage |
| Protein | Sources of protein, iron, zinc, and omega-3 fatty acids. | Tempeh, black beans, hazelnuts, chickpeas, salmon |
| Dairy | Sources of calcium, vitamin D, and protein. | Cottage cheese, cheddar cheese, yogurt, feta cheese, mozzarella |
What Exercises Can You Do during Week 26 of Pregnancy?
Exercises you can do during week 26 of pregnancy include walking, swimming, pelvic floor exercises, cycling, and stretching. The exercises for week 26 of pregnancy are below based on the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour:
| Exercise Type at Week 26 of Pregnancy | Description |
|---|---|
| Walking | Gentle, low-impact aerobic exercise that helps with endurance and overall fitness. |
| Swimming | Full-body workout, easing joint pressure while improving cardiovascular fitness. |
| Pelvic Floor Exercises | Strengthens muscles that support the bladder and uterus, reducing the risk of incontinence. |
| Stationary Cycling | A low-impact cardio workout that builds leg strength without stressing the joints. |
| Stretching | Enhances flexibility, relieves muscle tension, and helps improve posture and circulation. |
This set of exercises helps maintain overall health, strengthens muscles, and improves cardiovascular fitness. Keep your activity moderate, avoid overexertion, and remember to stay hydrated.
What Are The Things To Avoid At 26 Weeks Pregnant?
The things to avoid at 26 weeks pregnant are the following:
- Alcohol: Completely avoid alcohol during pregnancy, as it leads to birth defects and cognitive or behavioral issues in your baby, such as fetal alcohol spectrum disorders (FASD). A 2020 study titled “Alcohol Use in Pregnancy,” published in Clinical Obstetrics and Gynecology, highlights these risks.
- Smoking and Secondhand Smoke: Smoking increases the likelihood of preterm birth, low birth weight, and miscarriage. A 2020 study, “Exposure to Tobacco, Environmental Tobacco Smoke, and Nicotine in Pregnancy,” published in the International Journal of Environmental Research and Public Health, emphasizes the importance of quitting smoking as soon as possible.
- Recreational Drugs and Cannabis: These substances harm your baby’s development and lead to complications such as low birth weight and developmental delays.
- Caffeine: To reduce the risk of miscarriage or low birth weight, limit your caffeine intake to 200mg daily (about one 12-ounce cup of coffee).
- Certain Medications and Supplements: Check with your healthcare provider before taking any new medications, supplements, or herbal remedies, as some are dangerous during pregnancy.
- High Mercury Fish: Avoid fish high in mercury, like swordfish, king mackerel, and shark, as mercury harms your baby’s developing nervous system.
- Undercooked or Raw Meat: Consuming raw or undercooked meat increases the risk of toxoplasmosis, a parasitic infection that harms your baby.
- Unwashed Vegetables and Fruits: Always wash produce thoroughly to avoid harmful bacteria like listeria or toxoplasmosis.
- Deli Meats: Avoid deli meats unless fully heated to eliminate bacteria.
- Unpasteurized Foods: Refrain from consuming unpasteurized dairy products and soft cheeses containing harmful bacteria such as listeria.
- Hot Tubs and Saunas: Avoid hot tubs, saunas, and other high-temperature environments, as they raise your body temperature and potentially harm your baby.
- Strenuous Activities or Contact Sports: Avoid activities with a high risk of falling or abdominal injury, such as skiing, horseback riding, or contact sports.
- Exposure to Chemicals and Toxins: To safeguard your pregnancy, limit exposure to harsh cleaning chemicals, pesticides, and other environmental toxins.
- Cat Litter: If you have a cat, avoid handling cat litter to prevent toxoplasmosis, a dangerous disease for your baby.
- Hair Dye: Avoid using hair dye, particularly during the first and second trimesters, due to potential chemical risks. A 2018 study published in BMC Pregnancy and Childbirth noted that pre-pregnancy hair dye exposure is associated with an increase the risk of low birth weight, mainly in mothers with irregular menstruation before pregnancy.
By avoiding these risks and following your healthcare provider’s advice, you help ensure a healthy pregnancy at 26 weeks. Always consult your OBGYN for any specific concerns or questions.
How To Have Better Sleep At 26 Weeks Pregnant?
To sleep better at 26 weeks pregnant, follow the following strategies.
- Establish a Sleep Schedule: Going to bed and waking up at the same time daily helps regulate your body’s internal clock, improving sleep quality. Consistency reinforces your natural sleep-wake cycle.
- Create a Bedtime Routine: Engage in relaxing activities like reading or taking a warm bath before bed. Relaxing activities signal to your body that it is time to wind down, helping reduce stress and anxiety, which are common during pregnancy.
- Remove Disruptions Close to Bedtime: Avoiding caffeine, heavy meals, and screen time close to bedtime helps prevent sleep disruptions. These habits reduce sleep disturbances like heartburn and difficulty falling asleep.
- Sleep on Your Left Side: Sleeping on your left side improves circulation, alleviates pressure on your back, and reduces the risk of stillbirth, according to a 2017 study titled “Going to sleep in the supine position is a modifiable risk factor for late pregnancy stillbirth; Findings from the New Zealand multicentre stillbirth case-control study,” by Lesley M. E. McCowan et al., published in PLOS ONE. Sleeping on the left side promotes better blood flow to the fetus and kidneys, which helps manage swelling.
- Use a Body/Pregnancy Pillow: A body pillow supports your growing belly and relieve pressure on your back, hips, and knees. Body pillows promote comfort and stability, making it easier to find a comfortable position, according to a 2011 study from Turkey, titled “Pregnancy and Sleep Quality,” conducted by Nihal Taşkiran at the University of Adnan Mendere and published in the Turkish Society of Obstetrics and Gynecology.
- Exercise Regularly: Regular physical activity, such as walking or prenatal yoga, helps reduce insomnia and improve sleep quality. Exercise helps reduce pregnancy-related discomfort, such as back pain and leg cramps.
- Use Relaxation Exercises: Techniques like deep breathing, meditation, or progressive muscle relaxation calm your mind and body, aiding in faster sleep. Relaxation exercises reduce stress and anxiety, contributing to better sleep.
Adopting practices such as establishing a sleep schedule enhances sleep quality during pregnancy and manages the common sleep disruptions associated with week 26.
What Are The Possible Complications That Can Happen At 26 Weeks Pregnant?
Possible complications that can happen at 26 weeks pregnant include preterm labor, preeclampsia, gestational diabetes, placenta previa, placental abruption, and intrauterine growth restriction (IUGR). The possible 26-week complications are below.
- Preterm Labor: Preterm labor happens when contractions and cervical changes start before 37 weeks of pregnancy. Risk factors include stress, infections or abnormalities of the uterus or placenta, and experiencing hemorrhage.
- Preeclampsia: Preeclampsia is characterized by high blood pressure and protein in the urine after 20 weeks of pregnancy. Complications include poor placenta function, which causes intrauterine growth restriction and higher mortality rates for the baby. Signs of preeclampsia include increased syncytial knots and infarcts in the placenta, which indicate impaired blood flow. Monitoring for these signs is crucial during pregnancy to prevent serious complications for both the mother and baby.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) is a condition where high blood sugar levels occur during pregnancy. Risk factors include being older or obese. Signs of GDM at 26 weeks include fetal abdominal overgrowth. GDM increases the risk of macrosomia, where a baby weighs over 4 kilograms (about 8.8 pounds). Managing GDM before 24-28 weeks helps prevent complications like macrosomia and reduces delivery difficulties.
- Placenta Previa: Placenta previa occurs when the placenta partially or completely covers the cervix. Risk factors include previous cesarean sections, which increase the likelihood of complications such as severe bleeding. Signs of placenta previa include unexpected bleeding (antepartum hemorrhage). Management involves careful monitoring and often requires hospitalization.
- Placental Abruption: Placental abruption is a condition where the placenta detaches from the uterus before delivery, leading to significant vaginal bleeding and risks. Placental abruption accounts for about 11% of preterm deliveries before 28 weeks. Symptoms include abdominal pain and heavy bleeding. If unmanaged, placental abruption causes complications such as preterm delivery, low birth weight, and neonatal mortality. Monitoring for signs of this condition is crucial, especially for women with risk factors like high blood pressure or previous pregnancy complications.
- Intrauterine Growth Restriction (IUGR): IUGR is a condition in which the baby does not grow properly inside the womb. It results from issues like poor blood flow or placental problems. Complications of IUGR include lower birth weight and higher risks of health problems and neonatal death. Managing these risks is critical to ensuring support during and after delivery.
How Can A Partner Support The Mother At 26 Weeks Pregnant?
A partner can support the mother at 26 weeks pregnant emotionally and physically. Here are 7 ways a partner can support the 26-week pregnant mother.
- Emotional Support: Provide emotional support during pregnancy to enhance mental health. Partners listen, show care, and understand the mother’s feelings to reduce anxiety. Offer physical, emotional, and practical support, such as attending OB-GYN visits, asking questions, and giving reassurance. Practice patience and offer words of affirmation, compliments, and support to strengthen the relationship, decrease stress, and improve outcomes for mother and baby.
- Physical Affection: Physical affection includes hugs, kisses, holding hands, and gentle touches. This intimacy alleviates anxiety during pregnancy and enhances feelings of being cared for. Adequate partner support fulfills emotional needs, contributing to psychological well-being and fostering trust.
- Active Listening and Communication: Support through active listening involves focusing on the mother’s words helping your partner feel understood and valued. This support is crucial during pregnancy, especially as hormonal changes and stress lead to emotional fluctuations. Partners practice constructive communication, including sharing thoughts and feelings openly, to address concerns and foster teamwork. Positive dialogue helps alleviate stress and reinforces relationship dynamics, benefiting the mother and the couple during pregnancy.
- Shared Responsibilities: Support mothers by effectively sharing responsibilities. Show a positive attitude by taking on household chores or attending prenatal appointments to ease the mother’s burden. Offer instrumental support by physically helping with daily tasks and emotional support by showing empathy and reassurance. Responding builds trust while attending OBGYN visits and improves communication.
- Attend Prenatal Appointments: Attend prenatal appointments together to provide crucial support for expectant mothers. Maternal and child health outcomes are enhanced when fathers participate in prenatal care, according to a 2021 study from The United States, titled “Present as a partner and a parent: Mothers’ and fathers’ perspectives on father participation in prenatal care” by Tova B. Walsh PhD, MSW, et al., published in Infant Mental Health Journal. The father’s presence during ultrasounds reassures mothers and offers essential emotional support. Being present allows fathers to share critical experiences and gain information directly from healthcare providers.
- Physical Support: Physically supporting your partner at week 26 involves aiding with daily tasks such as household chores and grocery shopping. The partner’s involvement in daily tasks helps alleviate the mother’s physical burden. Supporting tasks include sharing housework, assisting with heavy lifting, and finding comfortable sleeping positions. Responsive support meets the mother’s needs and lowers prenatal anxiety.
- Encourage Healthy Habits: Encourage healthy habits by participating in a balanced diet and regular physical activity together. Partners positively influence each other’s behaviors, leading to more nutritious choices like increased fruit and vegetable intake. Joint efforts in meal planning and physical activities create a supportive environment. Exercise alongside her and provide emotional and practical support to enhance outcomes for both mother and baby.
What Prenatal Tests Are Needed At 26 Weeks Pregnant?
Two main prenatal tests are typically recommended at 26 weeks pregnant.
Glucose Tolerance Test (GTT): Gestational diabetes mellitus (GDM) is a condition in which women develop high blood sugar during pregnancy. GDM typically occurs between 26 and 30 weeks of gestation. The GTT process involves drinking a glucose solution followed by blood tests to measure how the body processes sugar. GDM poses risks like higher birth weight, delivery complications, and future health risks, such as childhood obesity and diabetes for the offspring.
Fetal Anatomy Scan: A detailed ultrasound (fetal anatomy scan) is revisited around this time if concerns or further detailed views are needed. This scan examines the baby’s major organs, bones, and overall growth, ensuring normal development.
When To Call For Your Doctor If Something Feels Wrong At Week 26 Of Pregnancy?
Call for your doctor at week 26 of pregnancy if there is vaginal bleeding, leaking fluid, severe abdominal pain, serious cramping, fever, severe lower back pain, regular contractions, decreased fetal movement, sudden swelling, persistent headaches, or intense itchiness in palms or soles. Below are 11 situations in which you must call your OBGYN immediately.
- Decreased Fetal Movement: Decreased Fetal Movement (DFM) is when a noticeable reduction in your baby’s movements occurs. Studies show that delays in reporting DFM lead to stillbirth and growth issues in the baby. If you feel fewer than ten movements in two hours when your baby is typically active at week 26 of pregnancy, contact your OBGYN immediately. Don’t wait longer than 24 hours if you notice an absence of movements.
- Vaginal Bleeding: Vaginal bleeding occurs in about 25% of pregnancies and leads to complications such as preterm labor (delivery before 37 weeks) in some cases. Heavier bleeding or multiple episodes of bleeding increase the risk of preterm labor. Unexpected bleeding often indicates low birth weight or delivery complications. Remember to always consult your OBGYN if you experience any vaginal bleeding.
- Vagina Leaking Fluid: Vagina leaking fluid at 26 weeks pregnant often indicates spontaneous previable rupture of membranes (SPROM), leading to complications. Early rupture of membranes causes low amniotic fluid (oligohydramnios), which affects fetal development. Contact your OBGYN immediately if the leakage increases, appears clear or straw-colored, or if you have contractions or discomfort.
- Severe Abdominal Pain/Cramping: Severe abdominal pain at 26 weeks pregnant signals serious conditions requiring immediate attention. Acute abdominal pain is often due to ectopic pregnancy or uterine complications. Severe pain, heavy bleeding, or fainting warrants urgent evaluation. Contact your OBGYN immediately, as experiencing these symptoms indicates miscarriage or premature labor.
- Fever Above 100.4°F: A fever above 100.4°F (38°C) is a high body temperature requiring medical attention. High fever harms the developing fetus at week 26 of pregnancy. Fever interferes with normal bodily functions and increases the risk of birth defects. 26-week pregnant mothers must contact an OBGYN if experiencing a high fever, as it leads to congenital heart defects and neural tube defects in the baby.
- Severe Lower-Back Pain: Lower back pain is intense discomfort caused by joint laxity from hormonal changes or increased weight at week 26 of pregnancy. About half of pregnant mothers report this pain, usually starting in the second trimester. Watch out for symptoms like intense pain, pain radiating down the legs, or pain disrupting daily activities. Immediate medical attention is necessary if leg numbness or bowel and bladder issues occur at week 26 of pregnancy.
- Regular Contractions: Regular contractions are rhythmic tightenings of the uterus. Normal contractions before 28 weeks are low-intensity and typically do not exceed three per hour. If contractions occur more than three times per hour at week 26 of pregnancy, it often signals a risk of preterm labor. Contact your OBGYN if contractions increase in frequency or intensity or are accompanied by discomfort, as this indicates preterm labor.
- Sudden Swelling in Hands, Face, or Feet: Sudden swelling in hands, face, or feet at 26 weeks pregnant often indicates preeclampsia. Preeclampsia involves high blood pressure and possible organ damage. If sudden swelling occurs alongside persistent headache, confusion, or visual disturbances, contact your OBGYN immediately. Prompt attention is crucial to prevent severe complications such as eclampsia, stroke, or kidney failure.
- Persistent Headaches with Vision Changes: Persistent headaches with vision changes involve recurring head pain accompanied by altered vision, often seen in 26-week pregnant mothers. While headaches are common at week 26 of pregnancy, paired vision changes like blurred sight or difficulty focusing indicate preeclampsia (high blood pressure). Hormonal fluctuations and weight gain cause these symptoms. Contact an OBGYN immediately if you experience sudden or severe symptoms, such as blurred vision, flashes of light, or spots.
- Intense Itching on Palms or Soles: Intense itching on the palms or soles during week 26 of pregnancy indicates intrahepatic cholestasis of pregnancy (ICP). This liver condition disrupts normal bile flow. Nighttime itching worsens without a visible rash and requires immediate attention from an OBGYN to assess the severity.
What are the 26 weeks pregnant symptoms not to ignore? 26 weeks pregnant symptoms not to ignore include decreased fetal movement, heavy vaginal bleeding, leaking fluid, severe belly pain, fever, severe backache, regular contractions, sudden swelling, persistent headaches with vision changes, and intense itching. Always trust your instincts during pregnancy. If something feels off at week twenty-six, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins That Need To Be Taken During Week 26 Of Pregnancy?
Yes, key vitamins and minerals are important to take during week 26 of pregnancy to ensure the mother’s and baby’s health and well-being, according to the American College of Obstetricians and Gynecologists (ACOG).
Calcium remains vital at week 26, with a recommended daily intake of 1,000 milligrams for women aged 19 to 50. Calcium is essential for developing the baby’s bones and teeth while maintaining the mother’s bone health.
Iron, recommended at 27 milligrams, continues to be necessary to support the increased blood volume and to ensure sufficient oxygen supply to both the baby and the mother. Proper iron intake at week 26 helps prevent anemia and boosts energy levels.
Iodine, at 220 micrograms per day, plays a crucial role in fetal brain development and the regulation of the mother’s thyroid function. Ensuring adequate iodine intake during this period supports healthy brain and nervous system growth in the fetus.
Choline, needed at 450 milligrams daily, is crucial for the ongoing development of the fetal brain and spinal cord at week 26. Choline helps reduce the risk of neural tube defects and supports cognitive development.
Vitamin A, at 770 micrograms for women in this age range, remains necessary for fetal growth and the development of vital organs such as the heart, lungs, and kidneys. This vitamin supports the mother’s skin health and vision.
Vitamin C, at 85 milligrams per day, aids in strengthening the immune system and maintaining healthy skin, gums, and connective tissue. Vitamin C enhances iron absorption, making it particularly beneficial during week 26.
Vitamin D, required at 600 international units, supports the baby’s bones and teeth development by facilitating calcium absorption. Vitamin D promotes healthy eyesight and immune function for both the mother and baby.
Vitamin B6, with a recommended intake of 1.9 milligrams, plays a key role in forming red blood cells and supporting the baby’s brain development. Vitamin B6 helps alleviate pregnancy-related nausea, which still occurs in week 26.
Vitamin B12, at 2.6 micrograms, is essential for maintaining the nervous system and red blood cell production. Sufficient B12 intake helps ensure proper fetal growth and prevents certain birth defects.
Folic acid remains critical at 400 micrograms per day during week 26. This nutrient supports the continued development of the baby’s brain and spine, reducing the risk of neural tube defects and aiding overall fetal development.
These nutrients are often found in high-quality prenatal vitamins, and taking the recommended daily dosage is essential for optimal health. Always consult with a healthcare provider to ensure you’re receiving the right vitamins and supplements tailored to your needs during pregnancy.
What Does Parenting Styles Suggest About 26 Weeks Pregnant?
Parenting Styles suggests expectant mothers prioritize self-care at 26 weeks pregnant.
“Self-care isn’t selfish; it’s nourishment for the soul. Fill your cup so you can abundantly pour into the life you’re creating,” advises Pamela Li, writer, Founder, and Editor-in-Chief of Parenting Styles.
Congratulations on being 26 weeks pregnant!