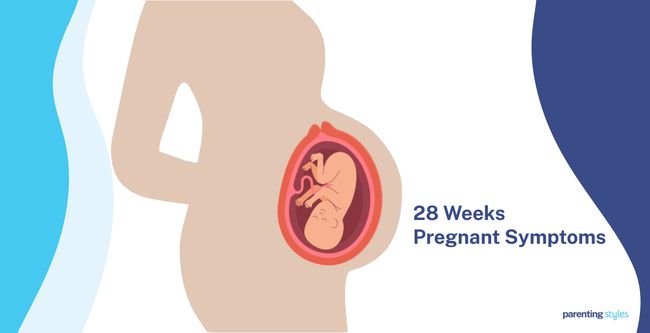
28 Weeks Pregnant Symptoms: Week 28 Of Pregnancy And Prenatal Care
28 weeks pregnant symptoms include overactive bladder (frequent urination or micturition), lower back pain (lumbar pain), pregnancy brain (forgetfulness), quickening (flutters), and constiption. 28 weeks pregnancy symptoms are often caused by the growing uterus and hormonal shifts. The 28-week baby is about the size of a large eggplant, weighing approximately 1,189 grams (2.62 pounds).
The baby’s brain is rapidly maturing, forming stable neural circuits that improve communication between brain structures. This development allows the fetus to regulate body temperature and practice rhythmic breathing. The baby’s sensory systems are advancing, with heightened responses to sound, particularly the mother’s voice.
The mother’s body undergoes significant changes at 28 weeks. The uterus rises above the belly button, and the circumference of the belly increases. Practice contractions, known as Braxton-Hicks contractions, often become more noticeable. The irregular, painless contractions prepare the body for labor.
Prenatal care is crucial at during week twenty-eight. Regular check-ups, including ultrasounds and tests like the Oral Glucose Tolerance Test (OGTT), help monitor maternal and fetal health. The OGTT screens for gestational diabetes, which affectsthe mother and baby if left untreated.
A healthy diet is essential during this time. Foods rich in folic acid, calcium, iron, and other vital nutrients support fetal growth and maternal health. Exercise is beneficial, and activities like walking, swimming, and gentle stretching are recommended.
Monitoring fetal movements at 28 weeks is essential. Counting kicks helps detect potential issues, but it’s important to understand that variations in fetal movement are normal. Contacting a healthcare provider is advised if there’s a significant decrease in movement.
Potential complications at 28 weeks include preeclampsia (high blood pressure and protein in urine), premature labor, and placenta previa (where the placenta covers part or all of the cervical opening). Any signs of these conditions must be reported to a healthcare provider immediately.
Support pregnant women by providing emotional and physical support, sharing responsibilities, encouraging healthy habits, and communicating effectively. Partner support significantly improves the pregnancy experience and outcomes for the mother and baby.
What is 28 weeks pregnant in months? 28 weeks pregnant is 7 months of pregnancy. 28 weeks is the last week in the second trimester. You have finished the seventh month of pregnancy.
What Are The Pregnancy Symptoms During Week 28?
28 weeks pregnant symptoms include overactive bladder (frequent urination or micturition), lower back pain (lumbar pain), pregnancy brain (forgetfulness), quickening (flutters), and constipation. Below are common 28-week pregnancy symptoms.
- Overactive Bladder (Frequent Urination): An overactive bladder is characterized by a frequent, strong, and sudden urge to urinate, even when the bladder isn’t full. Bladder control issues stem from physiological changes typically starting in early pregnancy and peaking in the third trimester. An overactive bladder affects about 52.2% of pregnant women, causing discomfort and disrupting daily activities. An overactive bladder sometimes leads to incontinence, resulting in urine leaks when sneezing, coughing, laughing, or straining.
- Lower Back Pain (Lumbar Pain): Lower back pain is a dull pain in the lumbar area that worsens when the pelvis is tilted forward. Lower back pain is due to joint laxity (looseness) caused by hormonal changes, the growing uterus adding strain on the muscles, and the compression of blood vessels leading to decreased oxygenation. Pain is intermittent and usually occurs within 30 minutes of walking, sitting, or standing. Around 62% of pregnant women experience pain in the lumbar region and pelvic area, beginning in week 18 and peaking in weeks 24-36.
- Pregnancy Brain (Forgetfulness): many expectant mothers experience what’s commonly known as “pregnancy brain” or “baby brain.” This phenomenon, affecting up to 81% of pregnant women, involves subtle changes in cognitive function. Women may notice increased forgetfulness, difficulty concentrating or maintaining focus, mild confusion or disorientation, challenges with reading comprehension, a slight decrease in verbal fluency, and reduced multitasking ability.
- Quickening: Fetal movement (quickening) is the first noticeable movement of the fetus as it presses against the maternal abdominal wall. Quickening occurs due to spontaneous brain activity and the development of neural circuits, allowing the fetus to produce rhythmic movements. Mothers feel rhythmic bursts of activity, such as kicks, stretches, and hiccups, starting between 14 and 22 weeks.
- Constipation: Constipation is characterized by infrequent bowel movements (less than three per week) and difficulty passing hard stools. Pregnant women experience elevations in progesterone, which reduces intestinal smooth muscle motility, leading to constipation. Constipation causes abdominal discomfort, pain during defecation, and straining, while severe cases cause fecal impaction and rectal bleeding. Around 35-39% of women experience constipation during the first two trimesters of pregnancy.
- Indigestion (Dyspepsia): Indigestion is a condition that causes a dull pain or burning sensation (heartburn) in the lower chest or upper abdomen, often accompanied by nausea and vomiting. Pregnancy-associated indigestion is caused by the slouched posture and relaxation of the lower esophageal sphincter, which usually prevents stomach contents from flowing back to the abdomen. Symptoms of indigestion worsen at night, often causing the mother to wake from sleep.
- Leg Cramps (Charley Horse): Leg cramps are sudden episodes of pain characterized by the involuntary spasm of the gastrocnemius muscle at the back of the lower leg. Leg cramps occur in pregnancy due to increased functional demand, joint laxity, and decreased bone mass. Approximately 41% of pregnant women report experiencing leg cramps.
- Insomnia (Trouble Sleeping): Insomnia is the impairment of sleep occurring thrice a week for at least three months, resulting in inadequate quantity and quality of sleep. Causes of insomnia include pregnancy-related changes in body temperature, pain, nasal congestion, decreased bladder capacity, anxiety, and stress. The prevalence of insomnia is 27.2% during the second trimester, rising to 39.7% in the third trimester.
- Breast Changes: Breast changes during pregnancy are characterized by growth and swelling caused by increased glandular tissue density. Breast changes are influenced by hormonal shifts, particularly elevated oestrogen levels, which increase milk production and ductal dilation. Blood flow to the breasts doubles from pre-pregnancy levels by 24 weeks. The areolar region thickens, and the milk ducts grow and expand.
- Prodromal Labor (Braxton-Hicks): Braxton-Hicks contractions are false labor pains characterized by intermittent contractions and relaxations of the uterine muscle. Braxton-Hicks indicates that the body is preparing for labor but does not suggest that labor has begun or is starting. Braxton-Hicks contractions are described as resembling mild menstrual cramps or abdominal tightening. Known triggers for Braxton-Hicks contractions include physical activity, a full bladder, and dehydration. Braxton-Hicks contractions start as early as week 6 of pregnancy, but mothers typically only start to feel the contractions during the second or third trimester.
- Skin Sensitivity: Skin sensitivity at 28 weeks pregnant involves various skin conditions, including a variant of PUPPP (pruritic urticarial papules and plaques of pregnancy) called prurigo of pregnancy (PP). PP is due to elevated estrogen and progesterone levels, which trigger an irregular immune response, resulting in itchy bumps and reddish patches on the abdomen and extremities. Skin changes affect 90% of pregnant women, with PP prevalent throughout, but especially in later stages of pregnancy, according to a 2012 study from India, titled “Pregnancy and Skin,” conducted by Kar Sumit et al. at Mahatma Gandhi Institute of Medical Sciences and published in The Journal of Obstetrics and Gynecology of India.
- Dizziness: Dizziness refers to unsteadiness and lightheadedness, influenced by weight gain and stress during pregnancy. Around 32% of pregnant mothers report feeling dizzy occasionally (1–2 times per week), while 4% experience frequent dizzy spells (3 or more times per week).
- Abdominal Cramping: Abdominal cramping is a painful sensation of tightness in the abdomen or stomach. Abdominal cramps present as dull or sharp pain in the midline, often accompanied by nausea and sweating. The expanding uterus causes cramping during pregnancy by altering the surrounding abdominal organs and stretching ligaments.
- Headache: Headaches are severe, throbbing sensations that start suddenly on one side of the head, above the ear. Headaches are caused by altered blood flow and increased pressure within blood vessels. Headaches result in stress, sleep deprivation, and depression. Most mothers notice improvement in headaches in the second and third trimesters of pregnancy.
- Restless Legs Syndrome (Willis-Ekbom Syndrome or Wittmaack–Ekbom Syndrome): Restless legs syndrome involves paresthesia (tingling) or unpleasant sensations accompanied by an urge to move the legs to achieve temporary relief. Low hemoglobin levels and maternal iron or folic acid deficiencies often cause restless legs. Around 27.1% of pregnant women are affected by restless legs syndrome during the second trimester, leading to increased fatigue, sleep disturbances, and daytime sleepiness.
- Piles (Hemorrhoids): Hemorrhoids are painful and itchy varicose veins in the rectal area. Hemorrhoids are caused by increased intra-abdominal pressure, constipation, and hormonal changes, contributing to compressing blood vessels as the uterus grows. Hemorrhoids are typically asymptomatic but often manifest as rectal bleeding and prolapse. Approximately 85% of pregnant women experience hemorrhoids during the second and third trimesters.
- Edema (Swollen Ankles and Feet): Edema, known as fluid retention, affects the lower extremities during pregnancy, causing swelling and discomfort. Swelling manifests as extra weight and a puffed-out feeling. Edema occurs when the growing uterus pressures blood vessels, hindering blood return from the legs to the heart. Approximately 87% of pregnant women experience swollen ankles and feet, with around 44% noticing an increase in shoe size by the third trimester due to swelling.
- Tingling (Sciatica): Sciatica refers to a sharp, shooting pain in the lower back that radiates to the buttocks and legs. Sciatic nerve compression during pregnancy leads to tingling, numbness, and leg weakness. Sciatica was reported at its highest in pregnant women at week 28 in a 2002 study from Sweden, titled “Symptoms across pregnancy in relation to psychosocial and biomedical factors,” conducted by Alina Rodriguez et al. at Uppsala University and published in Acta Obstetricia et Gynecologica Scandinavica.
- Vivid Dreams: Pregnant women often report experiencing vivid or unusual dreams, particularly about labor or the baby, becoming more common as pregnancy progresses. The dreams reflect conscious and unconscious emotions and are sometimes distressing, involving conflict with the baby’s father or fears of harm to the baby or themselves. Dreaming intensifies and becomes emotionally charged, with 67% of pregnant women reporting pregnancy-related dreams and 37% experiencing at least one frightening dream in a study conducted at the University of Missouri-Columbia Family Medical Care Center.
- GERD or Gastro-Esophageal Reflux (Heartburn): Gastro-esophageal reflux occurs when stomach acid flows back into the esophagus, causing discomfort and symptoms like heartburn. Severe complications of GERD, such as erosive esophagitis (erosion of the esophageal lining), bleeding, or strictures (narrowing of the esophageal lumen) are rare. GERD affects 40-85% of pregnant women, usually starting at the end of the first trimester and persisting throughout pregnancy.
- Itching: Itching in pregnancy typically occurs on the hands and feet but appears all over the body, usually without a rash. Intrahepatic cholestasis of pregnancy is a rashless itching at night. Cytokine shifts during pregnancy cause increased susceptibility to skin diseases in pregnant mothers by promoting autoimmunity, where the body attacks its tissues. Itching affects 20% of women with normal pregnancies.
- Shortness of Breath (Dyspnea): Dyspnea is the sensation of running out of air or difficulty breathing. The growing uterus pushes further into the ribcage during pregnancy, reducing lung capacity and leading to shortness of breath. Around 60% to 70% of healthy mothers feel shortness of breath during pregnancy.
- Bleeding and Swollen Gum (Pyogenic Granulomas or Pregnancy Tumor): Bleeding and swollen gums in pregnancy are characterized by smooth or raised lesions often covered with red bumps on the mouth. Pathogens, local irritants, and increased estrogen and progesterone trigger an excessive inflammatory response, leading to lesions. Approximately 94.9% of the lesions occur during the second and third trimesters of pregnancy.
- Bloating: Bloating is the sensation of fullness or abdominal tightness due to gas, often accompanying constipation. Bloating and constipation are caused by increased progesterone levels, changes in water absorption, dietary habits, and reduced physical activity. Food takes longer than usual to move through the bowels during the second and third trimesters, contributing to bloating. Around 25-40% of pregnant women in Western countries experience bloating.
- Nausea and Vomiting (Morning Sickness): Morning sickness is the feeling and act of throwing up in pregnancy. The severity of nausea correlates with hormones involved in the stress response, such as ACTH (adrenocorticotrophic hormone) and cortisol. Morning sickness occurs at any time of day, with the typical onset early in the morning.

What Is The Importance Of Understanding Being 28 Weeks Pregnant?
The importance of understanding being 28 weeks pregnant is to know that you have arrived at the end of the second trimester. Fetal movements, such as kicks and rolls, become more pronounced and are a vital indicator of the baby’s well-being. Tracking fetal movements to know that the baby is developing normally and that decreased movements alert the mother to potential issues.
The baby’s brain is rapidly maturing, forming stable neural circuits that improve communication between brain structures. Neural development is essential for your baby to start regulating body temperature and practicing rhythmic breathing, which is critical for survival outside the womb. The baby’s sensory systems are advancing, with heightened responses to sound, particularly the mother’s voice. Sensory developments are essential for the baby’s physical health, bonding, and emotional connections after birth.
Understanding the changes in her body at 28 weeks is equally vital for the mother. Common symptoms such as back pain, leg cramps, and indigestion tend to intensify due to the growing uterus and hormonal shifts. Recognizing and managing these symptoms during pregnancy week by week with appropriate prenatal care, such as proper posture, light exercises, and a balanced diet, significantly improves comfort and well-being during the remainder of the pregnancy.
Regular prenatal check-ups become increasingly important at this stage. Tests such as the Oral Glucose Tolerance Test (OGTT) are typically conducted around this time to screen for gestational diabetes, which affects mother and baby if left untreated. Monitoring blood pressure and checking for signs of preeclampsia, a potentially dangerous pregnancy complication, is crucial during these visits.
What To Expect At 28 Weeks Pregnant?
A 28-week pregnant mother should expect significant changes and developments as she arrives at the end of the second trimester. The fetus is now about the size of a large eggplant, weighing approximately 1,189 grams (2.6 pounds) and measuring almost 15 inches long. Fetal movements at week 28 become more pronounced, with the baby frequently kicking, stretching, and somersaulting. These movements are essential for muscle development and indicate healthy neural activity.
The baby’s brain is rapidly maturing, with stable neural circuits forming, which improves communication between brain structures. This development allows the fetus to regulate body temperature and practice rhythmic breathing. The fetal heart rate, typically between 110 and 160 beats per minute, continues to be a crucial indicator of the baby’s health.
The sensory system is advancing, with the baby responding to sounds, particularly the mother’s voice. The baby’s eyes now open and close voluntarily, and the lacrimal puncta, tiny openings for tear drainage, are beginning to function. Smell and taste receptors are active, allowing the baby to start experiencing the amniotic fluid’s unique odor and flavor profile.
The fetus’s skin is developing its unique patterns, and the vernix caseosa—a protective, creamy layer—covers the skin to protect it from the surrounding amniotic fluid. Male fetuses are likely experiencing testicular descent, which is part of their sexual development.
Mothers tend to experience increased discomfort, such as back pain, leg cramps, and indigestion, as the uterus expands and hormonal changes continue. Swelling in the ankles and feet, known as edema, is common due to fluid retention and pressure from the growing uterus. Second-trimester symptoms, such as insomnia or sleeping difficulties, tend to be more prevalent due to physical discomfort and hormonal shifts.
Prenatal care at this stage includes monitoring through ultrasounds and other tests, such as the Oral Glucose Tolerance Test (OGTT), to assess the risk of gestational diabetes. Regular check-ups will ensure that the mother and baby progress healthily as the pregnancy progresses into its final stages.
How Is The Baby Developing At 28 Weeks Pregnant?
Your baby is developing rapidly at 28 weeks of pregnancy, reaching the size of a large eggplant. The baby weighs approximately 1,189 grams (2.6 pounds) and measures almost 15 inches from head to toe. Growth is best monitored using ultrasound measurements, including biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and humerus length (HL). These measurements assess whether the baby is growing as expected.
Movements such as kicking, stretching, rolling, or tumbling become more common. These movements indicate good health and demonstrate that muscles and the nervous system are developing well.
The nervous system’s maturation allows the baby to regulate body temperature and start making rhythmic breathing movements. The brain forms more complex connections, preparing the baby for life outside the womb. REM sleep, crucial for brain development, becomes more established, and the baby begins to dream.
The rooting reflex, which helps babies instinctively seek nourishment after birth, starts developing at 28 weeks. Eye development continues, and the muscles controlling eyelid movement become more refined. Senses, including hearing, smell, and taste, develop, allowing the baby to start recognizing the mother’s voice and the unique smell and taste of the amniotic fluid.
Externally, the skin develops unique patterns that remain throughout life, and the vernix caseosa, a protective coating, continues to form. For male babies, the testes begin descending into the scrotum. All these developments are critical as the baby prepares for life outside the womb.
How Big Is Your Baby At Week 28 Of Pregnancy?
Your 28-week-old baby is about the size of a large eggplant. The 28-week-old fetus is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 50th percentile measurements for 28-week fetal growth are as follows: the biparietal diameter (BPD) is 72 millimeters, the head circumference (HC) is 264 millimeters, the abdominal circumference (AC) is 240 millimeters, the femur length (FL) is 52 millimeters, and the humerus length (HL) is 48 millimeters. The 28-week-old fetus weighs 1189 grams (41.94 ounces or 2.62 pounds), according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 28 Of Pregnancy?
- Rooting Reflex: The rooting reflex is an automatic response in which a baby turns its head toward a touch on the face, mouth, or cheek. The rooting reflex is an involuntary, instinctive action that helps babies seek nourishment by guiding them to locate and latch onto the nipple, which is essential for early feeding. The rooting reflex develops in fetuses at 28 weeks and becomes fully functional by 34 weeks of gestation.
- Fetal Movement: Fetal movement is felt by 28-week pregnant mothers with increasing strength, frequency, and diversity. Your baby moves around often, and hand movements are felt and visible underneath the skin. Movements include kicking, stretching, and grasping. Many mothers feel complex fetal movements like rolling, tumbling, and somersaulting at 28-32 weeks.
- Size and Weight: Ultrasound biometry helps monitor normal fetal growth and calculate size and weight at 28 weeks. The fetus is almost 15 inches long when measured head to toe and weighs approximately 1,189 grams (2.6 pounds). Male fetuses often weigh more than female fetuses. Your baby is about the size of an eggplant as the third trimester approaches.
- Fetal Position: Fetal position refers to the baby’s orientation in the uterus, with many starting to turn head-down in preparation for delivery, influencing the labor process. Around 76% of babies positioned themselves head-down (cephalic), 19% were breech, and 6% in other positions between weeks 25-28 in a 1985 study from The United States, titled “Fetal position during pregnancy,” conducted by Michael John Hughey, M.D. at Northwestern University School of Medicine and Evanston Hospital and published in American Journal of Obstetrics and Gynecology.
- Eye Development: The eyelids formed around the 9th week are nearly fully differentiated. Eye development at week 28 involves the differentiation of the orbicularis oculi muscle, which facilitates the eyelids’ voluntary closure. The lacrimal puncta, drainage ports for tears, opens around the 28th week after the eyelids separate. Eye development began in the 9th week when eyelids first started to form. The orbicularis oculi muscle is developing, which allows the baby to close its eyes voluntarily. The small openings that help drain tears (lacrimal puncta) begin to open as the eyelids separate.
- Sleep/Wake: Dreaming is facilitated by REM (Rapid Eye Movement) sleep, characterized by atonia (loss of muscle tone) in the spine or muscles. REM sleep is vital for your baby’s sensory system development, memory formation, and brain plasticity. REM sleep phases and dreaming start at 26-28 weeks of pregnancy, when distinct electrical patterns associated with the different sleep states emerge.
- Nervous System: Nervous system development involves refining brain connections during week 28. The brain transitions from temporary neural circuits to stable ones, helping different brain structures to communicate better. The central nervous system has developed enough for fetuses to start regulating body temperature and making rhythmic breathing movements. The brain’s outer layer (the cortical plate) begins to look more like a mature brain, and the connections between brain cells are refined for better neural function.
- Heartbeat: The fetal heartbeat is detected using a stethoscope, typically from 110 to 160 beats per minute (bpm). The overall pattern of the fHR is a vital indicator of normal fetal health and development, with variations in heart rate indicating fetal distress. The fetal heart starts developing at week 5, reaching approximately 170 bpm at 10 weeks before gradually slowing down as the pregnancy progresses.
- Survival Rate: The survival rate for premature babies increases from 0-33% at 24 weeks, with the survival rate increasing as pregnancy progresses. The introduction of surfactant therapy in June 1988 improved survival rates for infants delivered before term.
- Fat Development (Adipogenesis): Fat development begins in the fetus’s head and neck regions, progressively spreading through the trunk and limbs. Adipogenesis starts between the 14th and 24th weeks of gestation. Fat tissue is present in the six principal body areas (head, neck, thorax, abdomen, upper limb, lower limb) by around 28 weeks, contributing to noticeable weight gain in the fetus.
- Ears: Hearing is the fetus’s ability to detect and respond to sound, starting around 26 weeks of fetal life. The fetus recognizes and responds to the sound of the mother’s voice and develops eye blinking and startle reflexes in response to sounds, even in noisy surroundings. Most hearing and ear development in utero occurs between weeks 26 and 28.
- Sensory: Smell and taste development involves detecting odors and flavors through inhaling and swallowing the surrounding amniotic fluid. Taste receptors start developing between 7 and 8 weeks and are fully formed by the middle of the second trimester. Olfactory marker protein (important for the sense of smell) is expressed in the nasal mucosa, which detects smells, at week 28. This allows the baby to start experiencing smell (olfaction) and taste (gustation), which the baby recognizes through the unique odor profile of the amniotic fluid. The baby is swallowing about 750 mL of amniotic fluid daily.
- Skin: Skin development at 28 weeks pregnant involves the development of dermatoglyphics (skin patterns) for the unique identification of your baby throughout life. Epidermal ridges grow, enhancing the grip and functionality of the fetal hands. Skin features like palmar creases start forming by the end of the second trimester, around week 28.
- Vernix Development: Vernix caseosa is a white, creamy substance covering fetal skin in later pregnancy. Vernix protects the skin from amniotic fluid and has antimicrobial properties that assist in thermal regulation and hydration. Vernix caseosa forms when the skin’s periderm cells are shed and mixed with sebum secretions at week 21.
- Sexual Functions: Male sex organ development involves testicular descent, where the testes move from the abdomen through the inguinal canal into the scrotum. Descent begins around 24 weeks of gestation, with 75% of male fetuses having descended testes by week 28.

How To Know If Your Baby Is Healthy During Week 28 Of Pregnancy?
To know if your baby is healthy during week 28 of pregnancy, monitor the fetal movement closely and attend regular antenatal checkups.
- Monitor Fetal Movement: Monitor fetal movement through kick counts to assess the baby’s health. Fetal movement refers to the baby’s kicks, rolls, or other movements felt by the mother. Counting at least ten movements within 2-3 hours indicates normal development. Talk to your OBGYNs about kick counting and fetal movement monitoring at 28 weeks gestation.
- Schedule Regular Checkups: Schedule regular checkups to detect complications at week 28 of pregnancy. Routine screenings include assessing maternal blood pressure, weight, urine, belly size and ultrasounds to evaluate fetal growth and development. The WHO (World Health Organization) recommends a minimum of eight antenatal visits. Two visits are done in the second trimester, occurring every two weeks until 36 weeks, and then weekly visits.
Is Your Baby Settling Into The Proper Position For Labor At 28 Weeks Pregnant?
Yes, your baby likely has settled into the proper position for labor. The percentage of babies 25 to 28 weeks old who have settled into the cephalic (head down and bottom up) position is 76% in a 1985 study from the United States, titled “Fetal position during pregnancy,” conducted by Michael John Hughey, M.D. at Northwestern University School of Medicine and Evanston Hospital and published in American Journal of Obstetrics and Gynecology. Babies in breech (head up and bottom down) positions are around 19%, and 6% of 25-28 weeks babies are in other positions.
Do Babies Start to Dream While In The Womb At 28 Weeks Pregnant?
Babies start to dream while in the womb at 28 weeks pregnant through the development of rapid eye movement (REM) sleep. Distinct electrical patterns linked to different sleep states are observed in the fetal brain between 26 and 28 weeks, according to a 2008 study from The United States titled “Sleep and Brain Development: The Critical Role of Sleep in Fetal and Early Neonatal Brain Development,” conducted by Stanley N. Graven, MD et al. at the University of South Florida and published in Newborn and Infant Nursing Reviews.
REM sleep develops in the fetus around week 28 of pregnancy, vital for the growth of sensory systems, supporting brain plasticity (the brain’s ability to adapt and change), and forming long-term memory. Your baby spends most sleep time at 28 weeks in the REM stage, when dreaming is likely to occur.
What Are The Changes In The Mother’s Body At 28 Weeks Pregnant?
Changes in the mother’s body at 28 weeks pregnant include varicose veins, hormone changes, breast changes, body aches, stretch marks, and shortness of breath. Here are 10 main body changes in 28-week pregnant mothers.
- Varicose Veins (Spider Telangiectasia): Varicose veins are painful areas beneath the skin that appear as swollen, bluish veins. Increased blood volume and hormonal shifts dilate blood vessels, leading to congestion of blood in the veins. New-onset varicose veins mostly appear in the fifth and sixth month of pregnancy, including week 28.
- Hormone Changes: Hormonal changes during pregnancy mainly involve increased levels of estrogen and progesterone. The hormones cause lower esophageal sphincter (LES) pressure changes, leading to acid reflux into the esophagus and causing symptoms such as heartburn and indigestion. Stomach muscle relaxation, caused by increased progesterone, further aggravates symptoms. Hormonal effects contribute to various maternal symptoms and body changes as pregnancy progresses, such as mood swings, irritability, vivid dreams, fatigue, and changes in skin and hair.
- Breast Changes: The breasts grow and leak fluid as pregnancy progresses, caused by increased levels of prolactin (a hormone stimulating milk production). Prolactin causes the breasts to become fuller and supports the development of the mammary glands. Mammary glands start to leak colostrum (the baby’s first milk after birth) around week 20, and the mammary glands continue to grow, sometimes causing spontaneous fluid leakage.
- Body Aches and Pains: Body aches and pains often occur in the back, abdomen, groin, and thighs. The enlarging uterus adds extra weight, leading to posture and center of gravity shifts. Hormonal fluctuations loosen joints and ligaments simultaneously. Body aches and pains occur at any time during pregnancy, with around 70% of women experiencing lower back pain during pregnancy.
- Stretch Marks (Striae Gravidarum or SG): Stretch marks (striae gravidarum or SG) are pink and purple lesions that develop on the breasts, belly, and sometimes the buttocks, hips, and thighs. Hormones like relaxin, estrogen, and adrenocortical hormones contribute to the development of stretch marks. SG leads to the development of permanent white, crinkly streaks on the skin. The prevalence of SG in pregnant women ranges from 50-90% and often appears during the second or third trimester.
- Shortness of Breath (Dyspnea): Shortness of breath is the feeling of running out of air or difficulty breathing. The growing uterus puts pressure on the lungs as pregnancy progresses by pushing further into the ribcage, reducing lung capacity and leading to dyspnea. Approximately 60% to 70% of healthy mothers experience shortness of breath during pregnancy.
- Symphysis Fundal Height (SFH): Symphysis fundal height (SFH) is the distance between the top of the uterus and the top of the pubic symphysis, a joint in the pelvis. The uterus rises above the belly button by week 28. The circumference of your belly increases with each week of pregnancy. The mean abdominal circumference of 28 weeks pregnant women measured 241.2 mm in a 1996 study from London, titled “Charts of fetal size: 3. Abdominal measurements,” by Lyn S. Chitty et al., published in BJOG: An International Journal of Obstetrics & Gynaecology.
- Practice (Braxton-Hicks) Contractions: Braxton-Hicks contractions are irregular, painless contractions that prepare the body for labor. Practice contractions involve tightening of the uterine muscles without cervical dilation. The contractions start around week 6, but pregnant mothers only notice them in the second or third trimester. Braxton-Hicks are triggered by physical activity, a full bladder, dehydration, and sexual activity.
- Urinary Incontinence (Involuntary Urination): Urinary incontinence refers to unintentional urine leakage. Urinary incontinence is associated with maternal body weight, body mass index, and parity (number of pregnancies). Weakened pelvic floor muscles cause pregnancy-related pelvic pain and occasional episodes of incontinence. Urinary incontinence and pelvic girdle pain (PGP) affect up to 50% of pregnant mothers.
- Weight Gain: Weight gain is a natural and essential part of pregnancy as the baby grows and the body changes to support your developing baby and bump. A feeling of heaviness occurs due to the extra weight as the body stores more water for circulation, amniotic fluid, and the placenta. Weight gain during pregnancy varies depending on pre-pregnancy BMI (body mass index). Typical weight gain throughout pregnancy ranges from 11.5 to 16 kg for a mother with an average pre-pregnancy weight (BMI 18.5-24.9). Sudden weight gain exceeding 0.5 kg per week indicates potential health concerns requiring close monitoring.

How Big Is A 28 Weeks Pregnant Belly?
A 28-week pregnant belly has a fundal height of around 28 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 28-week-pregnant belly measures around 28 centimeters, between 26 to 30 centimeters. The expanding uterus grows to accommodate the growing fetus. The 28-week pregnant uterus has grown enough to be palpated above the navel level.
Several factors affect uterine size and growth rate, such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than those with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. The 2016 World Health Organization (WHO) ANC Guidelines concluded that there was inadequate evidence of using the SFH to predict fetal health.
Should You Expect Contractions On A Daily Basis At 28 Weeks Pregnant?
No, you should not expect regular contractions daily at 28 weeks pregnant. Daily regular contractions sometimes indicate potential preterm labor (PTL). PTL occurs with regular uterine contractions between the 20th and 37th week, causing early cervix opening, unlike Braxton-Hicks contractions. However, preterm contractions alone do not guarantee cervical opening. Signs of PTL include pelvic pressure, belly cramps, low backache, and frequent contractions.
Over 15 million babies experience preterm labor globally each year, with preterm birth rates reaching 10.23% in 2019 in the United States. Around 75% of PTL cases occur spontaneously with no known maternal and fetal risk factors, according to a 2020 study from The United States, titled “Preterm Labor and Birth,” by Kellie M Griggs et al., published in American Journal of Maternal/Child Nursing.
Consult your OBGYN if you experience regular daily contractions at 28 weeks pregnant. The American College of Obstetricians and Gynecologists (ACOG) advises monitoring these symptoms.
Why Does Your Skin Feel More Sensitive During Week 28 of Pregnancy?
Your skin likely feels more sensitive during week 28 of pregnancy due to changes in your body’s immune system and hormonal fluctuations. Your body shifts its immune response from one type (Th1) to another (Th2) to protect the fetus during pregnancy, according to a 2014 study titled “Skin disease in pregnancy,” by Catherine Nelson-Piercy et al., published in BMJ. The altered immune response affects the balance of specific immune system proteins, like cytokine, making your skin more prone to irritation and infection. Changes in cytokine production lead to further skin problems like dryness, itchiness, stretch marks, and breakouts. Pruritus gravidarum (intense generalized itching in pregnancy) affects 1 in 5 pregnant women, particularly in the first and second trimesters. Increased hormone levels during pregnancy heighten skin reactions and sensitivity to sunlight, heat, and some skincare products.
What Are The Tips For Prenatal Care During Week 28?
Tips for prenatal care during week 28 include tracking your baby’s movement, maintaining a healthy diet, keeping regular physical activities, practicing relaxation techniques, and staying in touch with your OBGYN. Here are 5 tips for prenatal care during week 28.
- Track Fetal Movement: Maternal perception of fetal movements remains the oldest and most common method for assessing fetal well-being. A noticeable decrease in fetal movements sometimes indicates complications, such as stillbirth or fetal growth restriction. Start doing kick counts at around 28 weeks of pregnancy to track your baby’s movement patterns. A healthy baby usually moves at least 10 times in 2 hours, and fetal movements are maximal between 28 and 34 weeks, according to a 2015 study, “Fetal movement counting for assessment of fetal wellbeing.” It’s essential to remain attentive to your baby’s daily activity and promptly alert your OBGYN if you notice any drastic changes in movement.
- Eat a Healthy Diet: Prioritize nutrition and food safety, as food-borne illnesses like listeriosis pose dangers during pregnancy. Ensure you consume sufficient protein, vegetables, and good fats to support your health and your baby’s development. Avoid high-risk foods like soft cheeses, cold seafood, sandwich meats, raw or undercooked meats, pre-prepared salads, uncooked bean sprouts, and raw eggs.
- Do Physical Activity: Staying fit during pregnancy, especially around week 28, enhances maternal physical and psychological well-being. However, avoid lifting heavy things as it poses risks. More energy spent on exercise is associated with better health outcomes for the mother and the baby.
- Practice Relaxation Techniques: Find a comfortable spot to sit with your hands on your abdomen. Techniques like mindfulness likely lower maternal heart rate, blood pressure, and stress hormones, improving emotional health during pregnancy. These relaxation practices have reduced fetal heart rate and motor activity, contributing to a calmer in-utero environment.
- Stay Engaged with Your Healthcare Provider: Regular consultations with your OB-GYN ensure consistent maternal and fetal health monitoring through tailored advice, prenatal screening, and routine checks such as urine tests, blood pressure measurements, weight monitoring, and measuring your belly.
What Types Of Foods Are Beneficial To Eat During Week 28 Of Pregnancy?
Foods that are beneficial to eat during week 28 of pregnancy include foods rich in folic acid, calcium, iron, iodine, choline, vitamins A, C, D, B6, and B12. Here are 15 essential minerals and vitamins for 28 weeks pregnant mothers.
Here are 15 types of foods rich in vitamins and minerals that are beneficial to eat during week 28 of pregnancy, according to the American College of Obstetricians and Gynecologists (ACOG).
- Folic acid (600 micrograms during pregnancy): Prevents neural tube defects and supports fetal growth. Best sources: Dark leafy greens, citrus fruits, fortified grains, asparagus, black beans.
- Calcium (1,000 milligrams for ages 19 to 50): Strengthens bones and teeth. Best sources: Buttermilk, brie, kefir, seaweed, bok choy.
- Iron (27 milligrams): Produces red blood cells and delivers oxygen to the fetus. Best sources: Ground beef, chicken, salmon, lentils, and chickpeas.
- Iodine (220 micrograms): Crucial for brain development. Best sources: Table salt, shrimp, dairy products, tuna, and eggs.
- Choline (450 milligrams): Choline supports fetal brain and spinal cord development. The best sources are skim milk, turkey liver, soybeans, kidney beans, and cauliflower.
- Protein: Essential for growth and repair, provides iron, zinc, and omega-3 fatty acids. Best sources: Lean beef, tofu, salmon, beans, nuts.
- Dairy: Sources of calcium, vitamin D, and protein. Best sources: Yogurt, cheddar cheese, goat milk, ricotta, fortified plant-based milk.
- Vitamin A (770 micrograms for ages 19 to 50): Aids in red blood cell formation and nutrient use. Best sources: Pumpkin, red peppers, kale, apricots, collard greens.
- Vitamin C (85 milligrams for ages 19 to 50): Promotes healthy gums, teeth, and bones. Best sources: Oranges, bell peppers, Brussels sprouts, strawberries, kiwi.
- Vitamin D (600 international units): Builds bones and teeth and maintains healthy eyesight and skin. The best sources are Sunshine, fortified orange juice, eggs, herring, and fortified almond milk.
- Vitamin B6 (1.9 milligrams): Assists in red blood cell formation and nutrient metabolism. Best sources: Tuna, chickpeas, bananas, pistachios, brown rice.
- Vitamin B12 (2.6 micrograms): Maintains the nervous system and aids red blood cell formation. Best sources: Clams, liver, sardines, fortified nutritional yeast, and dairy.
- Grains: Provide folic acid, fiber, iron, and B vitamins. Best sources: Quinoa, whole-grain bread, barley, millet.
- Fruits: Offer essential vitamins, minerals, antioxidants, and fiber. Best sources: Apples, berries, peaches, pomegranates, and figs.
- Vegetables: Supply calcium, vitamin D, and protein. Best sources: Kale, spinach, tomatoes, sweet potatoes, bell peppers.
What Exercises Can You Do During Week 28 of Pregnancy?
Exercises you can do during week 28 of pregnancy are walking, swimming, biking, stretching, and pelvic floor muscle training. Here are 6 exercises you can do at week 28 of pregnancy, according to the World Health Organization (WHO) 2020 Guidelines on Physical Activity and Sedentary Behaviour.
- Walking: A low-impact exercise that helps maintain cardiovascular health and keeps you moving without excessive strain. Walking uphill is particularly beneficial for building strength and endurance.
- Swimming: A full-body workout that supports your weight, reduces pressure on joints, and helps alleviate pregnancy-related discomfort. Aqua aerobics is another excellent option that is gentle on the body while providing effective exercise.
- Stationary Bicycling: Provides a good cardiovascular workout while minimizing the risk of falling, as balance is a concern during pregnancy.
- Stretching: Gentle stretches help maintain flexibility, relieve muscle tension, and prepare your body for childbirth.
- Pelvic Floor Muscle Training: Important for strengthening the muscles that support your bladder, bowels, and uterus, reducing the risk of urinary incontinence.
Engaging in at least 150 minutes per week of moderate-intensity activities like brisk walking or low-impact aerobics improves cardiorespiratory fitness and muscle strength. Regular exercise provides significant benefits. Start with low activity levels and gradually increase. Avoid exercises with physical contact and falling risks, and listen to your body as you work out.

What Are The Things To Avoid At 28 Weeks Pregnant?
Things to avoid at 28 weeks pregnant include alcohol, smoking, drugs, caffeine, fish high in mercury, raw meat, and unwashed vegetables. Here are 22 things to avoid at 28 weeks pregnant to ensure the health and well-being of you and your baby.
- Alcohol: Completely avoid alcohol, as it often causes severe developmental issues, including fetal alcohol spectrum disorders (FASD). Even low levels of alcohol consumption increase the risk of fetal cognitive and behavioral impairment, according to a 2020 study titled “Alcohol Use in Pregnancy,” published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Avoid smoking and exposure to secondhand smoke as it leads to complications like premature birth, low birth weight, and miscarriage. Quitting smoking early is beneficial to your baby’s well-being, as stated in the study “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy,” published in the International Journal of Environmental Research and Public Health.
- Recreational Drugs: Avoid all recreational drugs, including cannabis, as they tend to lead to low birth weight, developmental delays, and other complications.
- Caffeine: Limit caffeine intake to 200mg daily to reduce the risk of miscarriage and low birth weight. Caffeine is a central nervous system stimulant that increases alertness and attentional performance, so moderation is key.
- Certain Medications and Supplements: Consult your doctor before taking any medications, supplements, or herbal remedies, as some are harmful during pregnancy.
- High Mercury Fish: Limit consumption of fish high in mercury, such as swordfish, king mackerel, tilefish, and shark.
- Undercooked or Raw Meat: Avoid undercooked or raw meat to prevent infections that will likely harm your baby. Limit exposure to unpasteurized milk, as it poses health risks.
- Unwashed Vegetables and Fruits: Wash all produce thoroughly to prevent toxoplasmosis, which can sometimes lead to severe complications.
- Deli Meats: Avoid deli meats unless thoroughly heated to prevent exposure to harmful bacteria like Listeria. Lunch meats (cold cuts) fall into this category as they are often precooked or cured meats.
- Unpasteurized Foods: Avoid unpasteurized dairy products and soft cheeses, as they contain dangerous bacteria during pregnancy.
- Bagged Salads: Avoid pre-packaged salads due to the potential presence of harmful bacteria.
- Iron Supplements: Unnecessary intake of iron supplements leads to complications; only take iron supplements prescribed by your doctor.
- Extreme Diets: Avoid rapid weight loss or restrictive diets, as they tend to disrupt hormone levels and affect your pregnancy.
- Excessive Exercise: While staying active is beneficial, avoid intense exercise that negatively impacts your health or the baby’s. Remember to drink plenty of water and stay active safely to prevent constipation and hemorrhoids.
- Strenuous Activities or Contact Sports: Avoid activities with a high risk of falling, abdominal trauma, or heavy lifting.
- Trigger Foods: Be cautious of foods that trigger heartburn or hemorrhoids, which is common during pregnancy.
- Exposure to Chemicals and Toxins: Limit exposure to harmful chemicals and toxins in household cleaners and pesticides.
- Hot Tubs and Saunas: Avoid hot tubs and saunas, as high temperatures harm the developing fetus.
- Gardening: Wear gloves to avoid contact with contaminated soil that exposes you to harmful bacteria.
- Cat Litter: When handling cat litter, especially from outdoor cats, wear gloves and practice good hygiene to avoid toxoplasmosis, a parasitic disease that infects your baby.
- Stress: Avoid stress as much as possible and find healthy ways to manage it.
- Hair Dye: It’s best to avoid hair dye as it is likely to result in low birth weight, according to a 2018 journal, “The effect of pre-pregnancy hair dye exposure on infant birth weight: a nested case-control study.”
To have a healthy pregnancy, avoid these risks and remain well-informed. Always consult your OB-GYN or midwife if you have any questions or concerns.
Why is it Important to Count the Kicks of Your Baby at 28 Weeks Pregnant?
It is important to count your baby’s kicks at 28 weeks pregnant to monitor patterns of fetal movements because it provides insights into your baby’s well-being. Fetal movements are typically at their peak between weeks 28-34, according to a 2015 study titled “Fetal movement counting for assessment of fetal wellbeing,” by Lindeka Mangesi et al., published in the Cochrane Database of Systematic Reviews. Movements become more organized and feel slower but stronger as pregnancy progresses. A noticeable decrease in fetal movements sometimes indicates the baby is trying to conserve energy, indicating some distress. Counting kicks regularly helps you notice significant changes in your baby’s usual movement patterns.
Counting kicks helps detect potential issues, but it’s essential to avoid unnecessary stress and understand variations in fetal movement are normal. Some babies are more active than others, and a reduction in movement doesn’t always indicate a problem. Factors like decreased amniotic fluid, maternal health, or even the baby’s sleep patterns influence how much you feel your baby moving. Inform your healthcare provider to perform additional tests if you notice a significant decrease in fetal movement.
Should You be Worried if You Don’t Feel Any Kicking of Your Baby at 28 Weeks Pregnant?
It’s understandable to be worried if you don’t feel any kicking from your baby at 28 weeks pregnant. Still, it’s important to remember that several factors affect how often you feel fetal movements. Perception of fetal movements varies due to factors such as the baby’s sleep cycles, position, and daily activities. Fetal movements normally increase until around 32 weeks and then level off, so a decrease in the number or strength of movements is not entirely unusual, according to a 2020 study from Greece titled “Reduced Fetal Movements and Perinatal Mortality,” conducted by Aikaterini Bekiou et al. at the University of West Attica and published in Materia Socio Medica.
However, a significant decrease or absence of fetal movements indicates possible issues, especially if so few movements are unusual for you. Factors like low amniotic fluid, placental problems, and fetal distress influence fetal movement patterns. A lack of movement does not always mean something is wrong, but contacting your healthcare provider with concerns is essential. Your OBGYN performs tests to ensure your baby’s well-being and address any issues if necessary. Regular monitoring of fetal movements and consulting with your provider helps manage potential risks and ensures your health and your baby’s.
What Are The Possible Complications That Can Happen At 28 Weeks Pregnant?
Possible complications that can happen at 28 weeks pregnant include severe vomiting, preeclampsia, miscarriage, placental abruption, preterm birth, ectopic pregnancy, and premature rupture of membranes. Here are the seven complications that are possible during week 28 of pregnancy.
- Hyperemesis Gravidarum or HG (Severe Morning Sickness): Hyperemesis Gravidarum or HG (Severe Morning Sickness) is severe morning sickness characterized by excessive vomiting and weight loss during pregnancy. HG primarily affects young, non-Caucasian, and primiparous (first-time) mothers, with a familial history increasing the risk. Signs include excessive vomiting, at least a 5% loss of pre-pregnancy weight, the presence of ketones in urine, and electrolyte abnormalities.
- Preeclampsia: Preeclampsia is a severe condition occurring after 20 weeks of pregnancy, marked by high blood pressure and protein in urine. Signs of preeclampsia typically include elevated blood pressure (higher than 140/90 mmHg) and maternal organ dysfunction. Preeclampsia occurs in 3%-5% of pregnancies globally and leads to severe outcomes if untreated, such as eclampsia (seizures), kidney failure, and even death. Early detection and management of preeclampsia are vital to prevent serious complications such as intrauterine growth restriction (IUGR), preterm birth, oligohydramnios (low amniotic fluid), placental abruption (placenta separating from the uterus), fetal distress, and fetal death in utero.
- Miscarriage (Spontaneous Abortion): Miscarriage involves the death and expulsion of the embryo from the uterus before viability, specifically before 28 weeks. Common signs of miscarriage include vaginal bleeding and a lack of fetal cardiac activity. The risk of miscarriage increases significantly with advancing maternal age. The fetal loss rate escalated from 2.94% for women under 20 years to 50% for those aged 40-45 and over 45, in a 2001 study from Switzerland, titled “Spontaneous fetal loss rates in a non-selected population,” conducted by Wolfgang Holzgreve et al. at University of Basel and published in American Journal of Medical Genetics.
- Placenta Previa (Placental Abruption or Abruptio Placentae): Placenta previa is a serious pregnancy complication where the placenta lies unusually low and covers part or all of the cervical opening. Placenta previa causes painless vaginal bleeding and escalates to serious bleeding and shock, posing risks of postpartum hemorrhage and maternal death. Signs of placenta previa typically include painless vaginal bleeding during the second or third trimester, sometimes triggered by intercourse or medical examinations. Always consult your OBGYN for proper testing and management if you experience vaginal bleeding during pregnancy.
- Premature (Preterm) Birth: Premature (preterm) birth occurs when a mother goes into labor and delivers the baby between weeks 20 and 36 of pregnancy. Premature birth leads to severe complications, especially for babies born extremely early. Premature infants are at a higher risk of developing health issues such as respiratory distress syndrome (RDS) and neonatal jaundice. Premature babies usually need to be admitted to the intensive care nursery (ICN) and often require an extended stay in the neonatal intensive care unit (NICU) due to their delicate condition. Preterm labor poses significant health risks for the mother, including an increased chance of postpartum hemorrhage and the need for blood transfusions.
- Ectopic Pregnancy (Extrauterine Pregnancy): Ectopic pregnancy is when an embryo attaches and implants outside the uterus, often in the fallopian tube. Late diagnosis of ectopic pregnancy in the second trimester is usually due to inadequate care, especially in rural areas. Signs of ectopic pregnancy include severe abdominal pain, tenderness in the right lower abdomen, a pulse rate of 140 beats per minute, and low blood pressure at 90/60 mm Hg. Ectopic pregnancy is diagnosed by an ultrasound examination confirming the presence of a viable fetus in an abnormal location, and surgical intervention is usually necessary.
- Premature Rupture of Membranes or PPROM (Prelabor Rupture of Membranes): Premature Rupture of Membranes (PPROM) is a pregnancy complication where the amniotic sac, or “water,” breaks before labor begins. Signs of PPROM include a delay between the waterbreaking and delivery, maternal fever, rapid fetal heart rate, tenderness in the uterus, and foul-smelling amniotic fluid. PPROM affects 2-3% of pregnancies and is responsible for one-third of preterm births, according to a 2021 study from Spain titled “Obstetric and Perinatal Outcomes after Very Early Preterm Premature Rupture of Membranes (PPROM)-A Retrospective Analysis over the Period 2000–2020,” by Ernesto González-Mesa et al., published in Medicina. Potential complications of PPROM include placental abruption, cord prolapse, and perinatal mortality. Pregnant mothers must carefully monitor and report any unusual symptoms to their healthcare provider.
Can Preterm Labor Happen at 28 Weeks Pregnant?
Yes, preterm labor can happen at 28 weeks of pregnancy, giving birth to very preterm infants. Very preterm infants are born between 28 weeks and 37 weeks gestation. Extremely preterm infants are born before 28 weeks of gestation. Iatrogenic (illness-related) delivery is responsible for almost half of the very preterm births between 28 and 35 weeks in developed countries. Hypertension, pre-eclampsia, diabetes, multiple pregnancies, intrauterine growth restriction, maternal stress, and heavy physical work are among the major causes of such iatrogenic deliveries, according to a 2005 study from the UK, titled “The epidemiology of preterm labour,” conducted by Philip Steer at Imperial College London and published in BJOG: an International Journal of Obstetrics and Gynaecology.
Regular contractions, leaking fluid, and changes in vaginal discharge, such as an increase in pressure in the pelvis or persistent low back pain, signal preterm labor. Evidence shows that these signs occurring before 37 weeks necessitate seeing an OBGYN immediately.
How Can A Partner Support The Mother At 28 Weeks Pregnant?
A partner can be a great source of comfort and assistance for a pregnant woman at 28 weeks. Here are five ways to show your support
- Emotional Support: Provide emotional support during the 28th week to enhance mental health, especially when she tends to not feel like her usual self. Partners listen, show care, and understand the mother’s feelings to reduce anxiety. Practice patience and offer words of affirmation, compliments, and extra help to strengthen the relationship, decrease stress, and improve outcomes for mother and baby.
- Physical Support: Provide physical support by doing household chores, including cleaning, grocery shopping, and preparing meals to ease daily burdens. Offer additional comfort by providing back and foot massages. Engage in stress-relief activities, such as gentle exercises, to reduce anxiety and contribute to a positive experience at 28 weeks of pregnancy.
- Shared Responsibilities: Support mothers by effectively sharing responsibilities. Show a positive attitude by attending prenatal appointments to ease the mother’s burden. Offer instrumental support by physically helping with daily tasks. This instrumental support, which involves hands-on assistance, is crucial in lightening the load for the mother.
- Encourage Healthy Habits: Encourage healthy habits by participating in a balanced diet and regular physical activity together. Partners positively influence each other’s behaviors, leading to more nutritious choices like increased fruit and vegetable intake. Joint efforts in meal planning and physical activities create a supportive environment. Help her avoid unsafe foods by being mindful of ingredients and food choices during meal preparation. Exercise alongside her and provide emotional and practical support to enhance outcomes for mother and baby.
- Partner Communication: Get advice from other parents to better support your partner during this time. Listening to other parents’ experiences is valuable. Like resources such as books and websites, family and friends provide essential information. A great birth coach helps you prepare for the baby’s arrival by offering guidance and support. You benefit from asking questions in childbirth education classes and seeking resources tailored explicitly for fathers.
What Prenatal Tests Are Needed At 28 Weeks Pregnant?
Prenatal tests needed at 28 weeks include ultrasound, MRI, urine testing, amniotic fluid analysis, and the Oral Glucose Tolerance Test (OGTT). Additional assessments, such as chorionic villus sampling (CVS), noninvasive prenatal testing (NIPT), and the maternal serum screening test, are relevant earlier in the pregnancy or in cases requiring more comprehensive evaluation. Prenatal tests at week 28 focus on monitoring maternal and fetal health, while earlier tests like CVS and NIPT are critical for detecting genetic conditions.
Ultrasound remains the primary tool for detecting fetal anomalies, but MRI is useful when ultrasound is unable to fully assess an anomaly or rule out associated conditions. MRI uses electromagnetic fields instead of radiation and is safe during pregnancy, with no harmful effects reported.
Urine tests check for the presence of protein, sugar, and signs of infections to help identify complications like preeclampsia and anemia, according to a 2002 study from Brazil, titled “Biochemical profile of amniotic fluid for the assessment of fetal and renal development,” conducted by FR Oliveira et al. at Universidade Federal do Rio Grande do Sul and published in the Brazilian Journal of Medical and Biological Research. Amniotic fluid analysis measures biochemical markers like creatinine, urea, and uric acid, which indicate fetal kidney maturity. Screening for infectious diseases such as hepatitis B, HIV, and syphilis is essential for comprehensive prenatal care.
The Oral Glucose Tolerance Test (OGTT) assesses the risk of Gestational Diabetes Mellitus (GDM), which affects birth weight and fetal development. OGTT is performed between 24 and 28 weeks as a 1-hour, 50 g Glucose Challenge Test (GCT). A blood sample is taken after fasting, followed by a glucose solution. Additional blood samples are drawn at set intervals to track glucose levels. The OGTT identifies abnormal glucose tolerance, helping to prevent complications like larger birth weights. Early testing is essential for women with risk factors for diabetes.
Should You Be Admitted To The Hospital At 28 Weeks For Having Multiple Pregnancy?
Yes, admission to the hospital at 28 weeks is recommended for some multiple pregnancies, such as some monochorionic monoamniotic (Mo-Mo) twins, for daily surveillance. However, evidence supporting the efficacy of bed rest in reducing preterm birth risk remains weak. Women with uncomplicated twin pregnancies are often not recommended for routine hospitalization.
Monoamniotic twins are at high risk of intrauterine (the unborn baby) and neonatal (the baby from birth to four weeks of age) death, with perinatal mortality ranging between 10 and 40%, according to a 2014 study titled “Prenatal Management of Monoamniotic Twin Pregnancies,” by Tim Van Mieghem et al., published in Obstetrics & Gynecology. Multiple pregnancies are at high risk of complications like preterm labor, fetal growth restriction, or preeclampsia. Fetal death risks of multiple pregnancies are 18.1%, primarily due to factors such as umbilical cord entanglement. Fetal growth is reduced from 27 to 30 weeks in twins and from the 27th week in triplets compared with singletons.
Observational studies in the early 1950s identified improved perinatal outcomes in twins born to middle-class women. The suggestion to admit all twin mothers to the hospital at the 30th week, providing diet and rest to help them through the dangerous period, became widely accepted in obstetric practice, according to a 2010 study from Australia titled “Hospitalisation and bed rest for multiple pregnancy,” conducted by Caroline A Crowther et al. at The University of Adelaide and published in Cochrane Database of Systematic Reviews. Current studies have found no evidence supporting the assertion of benefits.
When To Call Your Doctor If Something Feels Wrong?
Call your doctor if you sense a drop in fetal movement, severe vomiting, premature labor contractions, depression, abdominal pain or bleeding, or generally feel that something feels wrong. Here are 6 things you must report to your doctor.
- Decreased Fetal Movement: A decrease in fetal movement signals potential perinatal issues, such as fetal growth restriction or stillbirth. J. Frederik Frøen et al.’s 2008 study in Seminars in Perinatology associates decreased fetal movement with severe outcomes. Monitoring the baby’s movements closely and seeking medical advice for fewer than ten movements in two hours is recommended.
- Severe Vomiting: Severe vomiting during this stage sometimes indicates hyperemesis gravidarum (HG), a condition beyond normal morning sickness that sometimes leads to dangerous dehydration, weight loss, and complications like electrolyte imbalances or preeclampsia. Vomiting that prevents food or fluid intake requires immediate contact with an OBGYN, as untreated HG tends to result in serious health issues.
- Premature Labor: Premature labor is another critical concern, characterized by regular contractions and cervical dilation before 37 weeks. Frequent contractions, severe abdominal pain, or lower back pain around week 28 necessitate calling an OBGYN immediately to manage the risks of early delivery.
- Depression or Anxiety: Mood or anxiety disorders often significantly affect pregnancy. With 60% of women experiencing these conditions, seeking help for overwhelming stress, sadness, or anxiety is important. Early intervention prevents the exacerbation of these disorders.
- Severe Abdominal Pain: Severe pain or cramping often indicates acute issues.
- Bleeding: Vaginal bleeding at 28 weeks pregnant significantly increases the risk of preterm delivery, low birth weight, and perinatal mortality. A 2013 study from Iran, titled “The Relationship Between Vaginal Bleeding in the First and Second Trimesters of Pregnancy and Preterm Labor,” conducted by Seyedeh Hajar Sharami, M.D. et al. at Guilan University of Medical Sciences and published in the Iranian Journal of Reproductive Medicine, supports this finding.
Don’t hesitate to contact an OBGYN if you experience issues or feel something is wrong.
What are the 28 weeks pregnant symptoms not to ignore? 28 weeks pregnant symptoms not to ignore include decreased fetal movement, severe vomiting, signs of premature labor, depression or anxiety symptoms, severe abdominal pain, and bleeding. Always trust your instincts during pregnancy. If something feels off at week twenty-eight, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins Needed To Be Taken During Week 28 Of Pregnancy?
Yes, prenatal vitamins and minerals are essential during the 28th week of pregnancy to support maternal health and fetal development. According to the American College of Obstetricians and Gynecologists (ACOG), maintaining adequate levels of these nutrients is crucial as the pregnancy progresses.
Calcium remains important at 28 weeks, with a recommended intake of 1,000 milligrams for women aged 19 to 50. Talking calcium is vital as the baby’s bones and teeth continue to develop and strengthen, drawing calcium from the mother’s stores if necessary.
Iron is equally crucial at this stage, with a recommended dose of 27 milligrams. Iron supports the increased blood volume and helps deliver oxygen to the mother and the baby. Without adequate iron, the risk of anemia increases, which leads to complications.
Iodine, needed at 220 micrograms, is essential for developing the baby’s brain and nervous system. Iodine ensures the thyroid functions properly, critical for regulating the baby’s growth.
Choline, at 450 milligrams, continues to play a significant role in developing the fetal brain and spinal cord. This nutrient helps prevent neural tube defects and supports overall cognitive development.
Vitamin A, with a recommended intake of 770 micrograms, aids in developing the baby’s skin, eyesight, and organs. However, not exceeding this amount is important, as too much vitamin A is harmful.
Vitamin C, recommended at 85 milligrams, supports the immune system, promotes healthy skin and connective tissues, and helps with iron absorption. It is imperative in conjunction with the increased iron needs at 28 weeks.
Vitamin D, at 600 international units, is necessary for calcium absorption, ensuring the baby’s bones and teeth are properly developing. It supports the mother’s immune system and mood.
Vitamin B6, needed at 1.9 milligrams, is essential for forming red blood cells and helps manage pregnancy-related nausea, which is still an issue during the 28th week.
Vitamin B12, at 2.6 micrograms, supports the development of the baby’s nervous system and works with folic acid to produce red blood cells and DNA.
Finally, folic acid remains essential, with 400 micrograms recommended daily to continue supporting the baby’s neural development and preventing brain and spine birth defects.
It’s recommended to continue taking a daily prenatal vitamin that includes these nutrients. Discuss with your healthcare provider if any adjustments to your supplementation are needed as your pregnancy progresses, and ensure you’re eating a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
What Does Parenting Styles Suggest About 28 Weeks Pregnant?
Parenting Styles suggests that 28-week pregnant mothers create a birth plan and start packing the hospital bag.
“Preparing a birth plan and packing a hospital bag help you feel ready as the due date approaches, giving you peace of mind,” explains Pamela Li, writer, Founder, and Editor-in-Chief of Parenting Styles.
Congratulations on being 28 weeks pregnant!