29 Weeks Pregnant Symptoms: Week 29 Of Pregnancy And Prenatal Care
29 week pregnant symptoms include restless legs syndrome, pregnancy brain, quickening, heartburn, insomnia, bleeding gum, headaches, and lower back pain. Other 29 weeks pregnancy symptoms are hemorrhoids, constipation, overactive bladder, and Braxton-Hicks contractions.
Fetal movement, known as quickening, becomes more noticeable. The baby actively kicks, stretches, and makes rhythmic movements. Gastroesophageal reflux (GERD) occurs due to hormonal changes that relax the esophageal sphincter, leading to heartburn and discomfort. Insomnia is common, exacerbated by back pain, frequent urination, and fetal movements. Bleeding gums, headaches, and hemorrhoids are typical, reflecting the body’s adjustments.

The 29-week fetus, now the size of a butternut squash and weighing around 1,350 grams (47.62 ounces or 2.98 pounds), continues to grow rapidly. Developmental milestones include lung maturation and alveoli formation, which are vital for breathing post-birth. The bone marrow now produces red blood cells; fat accumulation under the skin supports energy storage and temperature regulation. The brain develops connections for movement and sensory processing, and the skeleton absorbs calcium to strengthen bones.
Regular prenatal checkups monitor fetal growth and development. Health providers measure key growth parameters like the biparietal diameter (BPD) and abdominal circumference (AC) using ultrasound to ensure the baby is progressing as expected. Counting fetal movements helps monitor your baby’s health. Any decrease in activity must be reported immediately to detect potential complications like preterm labor or fetal growth restriction. Understanding the symptoms and developmental changes at 29 weeks helps mothers manage discomfort and seek appropriate relief strategies.
What is 29 weeks pregnant in months?
29 weeks pregnant is 7 months and 1 week within the third trimester of pregnancy. You are in the first week of the eighth month of pregnancy. Week 29 is the first week in the third trimester.
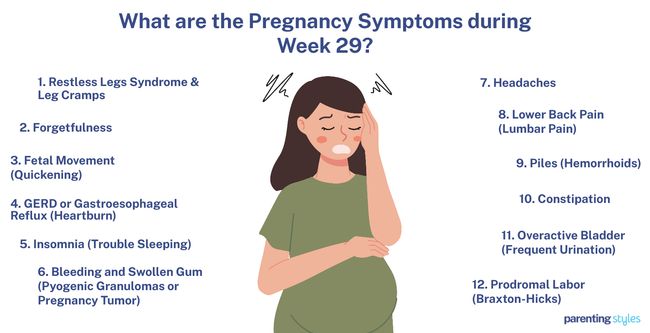
What Are The Pregnancy Symptoms During Week 29?
29 week pregnant symptoms include restless legs syndrome, pregnancy brain, quickening, heartburn, insomnia, bleeding gum, headaches, and lower back pain. Below are common 29 weeks pregnancy symptoms.
- Restless Legs Syndrome & Leg Cramps: Leg cramps (LCs) and restless legs syndrome (RLS) are two often underdiagnosed sleep disorders in the third trimester. Leg cramps are intense, painful muscle contractions, while RLS is discomfort characterized by an irresistible urge to move the legs. Leg cramps affect up to 30% of pregnant women, while RLS affects up to 26%, according to a 2009 study from The United States titled “Leg Cramps and Restless Legs Syndrome During Pregnancy,” conducted by Jennifer G. Hensley at the University of Colorado Denver and published in The Journal of Midwifery & Women’s Health. Leg Cramps and RLS typically occur at night and are characterized by a cramping sensation in the lower legs, usually relieved by movement.
- Forgetfulness: Forgetfulness is the tendency to forget things and have poor memory, often referred to as “pregnancy brain” or “baby brain” during gestation. Maternal cognitive functions rely on a steady supply of glucose. More glucose is redirected from the mother’s brain to the fetus during pregnancy, especially as the baby grows, leading to forgetfulness. Verbal recall ability, processing speed, and spatial recognition memory gradually decrease from the 29th week onward as the baby’s energy requirements increase. 80% of pregnant women report experiencing forgetfulness in pregnancy.
- Fetal Movement (Quickening): Quickening is the first noticeable movement of the fetus against the maternal abdominal wall. Mothers begin to feel the baby kick and stretch from weeks 14-22. The fetus is active, kicking more and making rhythmic and expressive movements. The fetus demonstrates grasping movements, squeezing, and occasionally sucking on the umbilical cord during the third trimester, including week 29.
- GERD or Gastroesophageal Reflux (Heartburn): Gastroesophageal reflux happens when stomach acid flows back into the esophagus, causing discomfort. Progesterone decreases lower esophageal sphincter pressure during pregnancy, leading to acid reflux. Common symptoms of GERD are heartburn, regurgitation, nausea, and vomiting. GERD affects 30-50% of pregnant women and often continues into the third trimester, even though symptoms usually decrease as pregnancy progresses.
- Insomnia (Trouble Sleeping): Insomnia is a sleep disorder in which a person has trouble falling or staying asleep at least three times a week for three months or more. Sleep disturbances are common during pregnancy due to backache, urinary frequency, fetal movements, GERD, and leg discomfort. Over 98% of pregnant mothers, including 29-week pregnant women, experience nighttime awakenings in the third trimester.
- Bleeding and Swollen Gum (Pyogenic Granulomas or Pregnancy Tumor): Bleeding and swollen gums in pregnancy are characterized by smooth or raised lesions on the mouth, often covered with red bumps. Local irritants, bacteria, and poor oral hygiene predispose women to pyogenic granulomas. Increased progesterone during pregnancy causes a chronic tissue reaction, exacerbating inflammation. Approximately 94.9% of the mouth lesions occurred during the second and third trimesters of pregnancy in a 2016 study from China titled “Initial periodontal therapy for the treatment of gingival pregnancy tumor,” conducted by C.Z. Li et al. at Wuhan University and published in Genetics and Molecular Research.
- Headaches: Headaches are severe, throbbing pains that start suddenly on one side of the head, above the ear. Headaches during pregnancy are categorized as primary headaches, including migraines, or secondary headaches, indicating more serious conditions such as preeclampsia. Headaches often lessen by the third trimester, though about 10% of pregnant women experience worsening symptoms.
- Lower Back Pain (Lumbar Pain): Lower back pain is a dull ache in the lower back, sometimes spreading to the legs and often worsening upon bending forward. Lower back pain is caused by hormonal changes loosening the joints, abdominal muscles weakening as the uterus expands, and pressure on blood vessels. Pain in the lumbopelvic area, which involves pain in the lower back, the pelvis, or both, typically begins around week 18 and is most intense between weeks 24 and 36. Low back pain affects anywhere from 20%-90% of pregnant women.
- Piles (Hemorrhoids): Hemorrhoids are swollen veins located in the rectum and around the anus. Hemorrhoids are caused by increased pressure in the rectal veins due to the growing uterus, constipation, and hormonal changes during pregnancy. Hemorrhoids usually lead to symptoms like bleeding, itching, pain, and difficulty with bowel movements. About 85% of pregnant women experience hemorrhoids during the second and third trimesters.
- Constipation: Constipation in pregnancy is characterized by infrequent bowel movements, hard stools, and difficulty emptying the bowels, often accompanied by pain and straining. Constipation occurs due to increased progesterone, which slows intestinal movement and reduces water content, leading to harder stools. About 21% of women experience constipation during the third trimester.
- Overactive Bladder (Frequent Urination): Overactive bladder is characterized by a frequent, strong, and sudden urge to urinate, even when the bladder isn’t full. Urinary tract infection (UTI) and gestational diabetes contribute to the prevalence of urogenital symptoms in pregnancy. An overactive bladder occasionally leads to incontinence, resulting in urine leaks when sneezing, coughing, laughing, or straining. Overactive bladder symptoms begin early in pregnancy, with up to 95% of pregnant women experiencing frequent urination in late pregnancy.
- Prodromal Labor (Braxton-Hicks): Braxton-Hicks contractions are irregular, sporadic uterine contractions starting as early as the 6th week of pregnancy, becoming more noticeable during the second and third trimesters. Braxton-Hicks contractions are typically non-painful and vary in intensity, frequency, and duration. Often referred to as “false labor pains,” Braxton-Hicks contractions help prepare the body for actual labor, softening the cervix and improving blood flow to the placenta, but don’t cause cervical dilation or lead to birth.
What Is The Importance Of Understanding Being 29 Weeks Pregnant?
Understanding the significance of being 29 weeks pregnant involves recognizing the physical and emotional changes the mother and baby experience. The mother’s body undergoes significant adjustments to accommodate the growing baby, leading to symptoms such as sleep disturbances, forgetfulness, lower back pain, hemorrhoids, and constipation. The symptoms disrupt daily life and affect overall well-being, making coping strategies necessary.
Ensuring the mother gets adequate rest is one of the primary concerns at 29 weeks. Factors like lower back pain, an overactive bladder, and restless legs syndrome (RLS) interfere with sleep quality. RLS, characterized by an uncomfortable urge to move the legs and nighttime leg cramps caused by painful muscle contractions, disrupts sleep and contributes to fatigue. Understanding the symptoms enables the mother to seek relief through gentle exercises, proper hydration, and a comfortable sleeping environment.
“Pregnancy brain,” or forgetfulness, presents another critical aspect of week 29. The growing baby diverts glucose, a vital energy source, from the mother’s brain, leading to memory lapses. Recognizing the pregnancy brain as a normal part of pregnancy reduces anxiety and helps the mother manage by staying organized with lists and reminders.
The baby, now the size of a butternut squash, experiences significant developmental milestones. The baby’s lungs continue to mature, and fat tissue accumulates, preparing the baby for life outside the womb. Monitoring the baby’s development remains essential. Regular prenatal visits to check the baby’s growth, including measurements like the biparietal diameter (BPD) and abdominal circumference (AC), ensure the baby is progressing well. Counting fetal movements daily is a simple yet effective way to monitor the baby’s health.
Vigilance regarding potential complications like preterm labor remains crucial at week 29. Frequent, painful contractions prompt immediate medical attention to prevent preterm birth. Monitoring symptoms like severe headaches, abnormal swelling, or unusual discharge remains critical, indicating conditions such as preeclampsia or other complications.
Prenatal care during the third trimester includes attending regular check-ups, maintaining a balanced diet rich in essential nutrients like calcium, iron, and folic acid, and engaging in safe exercises. Understanding and addressing the changes and challenges of being 29 weeks pregnant helps ensure a healthy pregnancy. Tracking the pregnancy week by week helps mothers prepare for the upcoming weeks leading to childbirth.
What To Expect At 29 Weeks Pregnant?
The 29-week pregnant mother must expect several physical and emotional changes as her body adapts to the growing baby. Sleep disturbances are common third-trimester symptoms due to factors like lower back pain, an overactive bladder, and conditions such as restless legs syndrome (RLS) and leg cramps. RLS involves an uncomfortable urge to move the legs, often disrupting sleep, while leg cramps are painful muscle contractions typically occurring at night. Forgetfulness, frequently called “pregnancy brain,” usually worsens as the baby’s energy needs grow, diverting glucose from the mother’s brain and leading to memory lapses.
The expanding uterus and hormonal changes cause lower back pain and piles (hemorrhoids), which are swollen veins in the rectal area. These uterine changes lead to discomfort and difficulty with bowel movements. Constipation is another common symptom resulting from slowed intestinal movement. Gastroesophageal reflux (GERD) further causes heartburn and regurgitation due to relaxed esophageal muscles.
The mother notices increased fetal movement as the pregnancy progresses, called quickening. Fetal movements include kicks, stretches, and other movements as the baby becomes more active. Braxton-Hicks/false labor contractions become more noticeable, though they are usually non-painful and irregular.
The baby’s development is progressing rapidly. The fetus is about the size of a butternut squash, weighing around 1,350 grams (2.98 pounds). Key milestones include further lung development, with alveoli forming to prepare for breathing after birth. The baby’s brain is developing rapidly, with neurons forming vital connections, and the bone marrow is now the primary site of red blood cell production.
Regular prenatal checkups are essential, including tests like blood pressure monitoring, urinalysis, and possibly an oral glucose tolerance test (OGTT) to screen for gestational diabetes. An ultrasound is sometimes performed to check the baby’s growth and position, while preeclampsia screening usually involves a transvaginal ultrasound to assess the uterine arteries.
Week 29 is marked by continued growth and preparation for birth, with the mother experiencing physical symptoms and important milestones in her baby’s development.
How Is The Baby Developing At 29 Weeks Pregnant?
The 29-week-old baby is developing rapidly, reaching several key milestones in preparation for life outside the womb after pregnancy. The fetus is about the size of a butternut squash and weighs around 1,350 grams (47.62 ounces or 2.98 pounds). Lung development enters a critical stage as tiny air sacs, called alveoli, begin forming. Alveoli are essential for breathing after birth and develop throughout the pregnancy.
Red blood cell production has fully transitioned from the liver to the baby’s bone marrow. The shift ensures sufficient red blood cells are produced to meet increasing oxygen and nutrient demands.
Neurons form connections and essential nerve pathways in the brain, such as the corticospinal and spinothalamic tracts, crucial for movement and sensory processing.
Fat development accelerates, with deposits forming under the skin. These deposits are vital in energy storage and temperature regulation after birth.
Bone development continues, with the baby’s skeleton absorbing more calcium to strengthen bones. Secondary ossification centers become visible, indicating well-progressing bone formation.
How Big Is Your Baby At Week 29 Of Pregnancy?
Your 29-week-old baby is often measured in biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and humerus length (HL) rather than crown-rump length (CRL). The 29-week-old fetus is about the size of a butternut squash. The 50th percentile measurements for 29-week fetal growth are as follows: the BPD is 74 millimeters, the HC is 273 millimeters, the AC is 250 millimeters, the FL is 54 millimeters, and the HL is 49 millimeters. The 29-week-old fetus weighs 1,350 grams (47.62 ounces or 2.98 pounds), according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 29 Of Pregnancy?
The week 29 key developmental milestones include lung development, red blood cell production (definitive erythropoiesis), brain development, fat development, and bone development. Here are the 6 key developmental milestones for babies at week 29 of pregnancy.
- Lung Development: The fetal lungs enter the saccular–alveolar stage of development from week 28 to term. Tiny air sacs called alveoli begin forming at around 29 weeks through amelogenesis, the final stage of lung development. Alveoli continue to develop throughout the remainder of pregnancy, reaching 100-150 million by the time the baby is born. The lungs’ alveoli and airways play a crucial role in the baby’s breathing movements in preparation for life outside the womb.
- Red Blood Cell Production: The baby’s bone marrow is the primary site for red blood cell production by week 29 of pregnancy. The fetus starts making red blood cells, beginning in the yolk sac during weeks 3-6, shifting to the liver from weeks 6-22, and finally transitioning to the bone marrow. Bone marrow erythropoiesis significantly increases red blood cell production, ensuring the fetus has an adequate supply to meet growing metabolic demands.
- Size and Weight: Ultrasound biometry is used to monitor normal fetal growth, and at 29 weeks, your baby is about the size of a butternut squash. The fetus weighs approximately 1,350 grams (2.98 pounds), according to a 2017 study from Norway titled “The World Health Organization Fetal Growth Charts: A Multinational Longitudinal Study of Ultrasound Biometric Measurements and Estimated Fetal Weight,” conducted by Kiserud, T. et al. at Department of Clinical Science, University of Bergen and published in PLOS Medicine. It’s common for male fetuses to weigh slightly more than female fetuses.
- Brain Development: The fetal brain’s functional connection to the body is established, demonstrated by the ability to perceive pain during the third trimester. Brain neurons form connections with other neurons after reaching their final positions. The corticospinal tract, a vital nerve pathway, extends to the lower part of the spinal cord by week 29 of development. The spinothalamic tract, which links the spinal cord to the thalamus, becomes myelinated around week 29, improving the conduction of electrical signals.
- Fat Development: Fat development, or adipogenesis, involves the maturation of energy-storing cells as fat (adipocytes) and begins around the 14th week of gestation, with initial fat deposits appearing in the cheeks. The demand for structural lipids and fatty acids rises significantly in the third trimester as the fetal brain rapidly grows in cell size, number, and neuromotor activity. The mother provides long-chain polyunsaturated fatty acids (LC-PUFA) to the fetus, which are crucial for developing fat reserves necessary for the nervous system’s growth and function.
- Bone Development: Ossification is the process of bone formation in the fetus, beginning at around eight weeks of gestation, starting with the clavicles and mandible. Your baby’s skeleton is actively absorbing calcium to support bone development. Secondary ossification centers, which are cartilaginous structures at the ends of long bones, are seen on ultrasound and MRI, indicating primary ossification is mainly complete by week 29.

How To Know If Your Baby Is Healthy During Week 29 Of Pregnancy?
To know if your baby is healthy during week 29 of pregnancy, visit your OBGYN (obstetrician-gynecologist or OB-GYN), check the baby’s heartbeat, track fetal size, count fetal movement, and monitor bone growth. Here are 6 ways to know if your baby is healthy during week 29 of pregnancy.
- Visit Your OBGYN: Regular checkups with your OBGYN help monitor your baby’s health, with high-risk pregnancies needing more frequent surveillance. Your OBGYN assesses your blood pressure, weight gain, and other factors to ensure normal progress.
- Check Baby’s Heartbeat: Monitoring fetal heartbeat during prenatal visits helps ensure the baby is healthy. Your healthcare provider checks if your baby has enough oxygen and nutrients. An OBGYN uses Doppler ultrasound and physical examinations to monitor fetal heart activity.
- Track Fetal Size: The week-29 baby is about the size of a butternut squash. An OBGYN uses ultrasound to provide data on fetal size and estimated fetal weight (EFW) to ensure the baby thrives.
- Count Fetal Movements: Monitoring fetal movement (quickening) is one of the oldest and most effective methods for assessing your baby’s health. Fetal movements typically increase in strength and frequency between weeks 28 and 32 of pregnancy, according to a 2017 study titled “Maternal perception of fetal movements in the third trimester: A qualitative description.” Decreased fetal movement (DFM) early in the third trimester is linked to stillbirth or fetal growth restriction. Pregnant women are encouraged to track daily fetal activity. Report to your doctor immediately if unusual changes or decreases in quickening are noticed.
- Monitor Bone Growth: Ultrasound and MRI track bone formation and maturation. Secondary ossification centers (where bone formation occurs) become visible on ultrasound and MRI from 29 weeks of pregnancy onward, according to a 2012 study titled “MR imaging of the fetal musculoskeletal system.”
Does Your Baby Get More Fat At 29 Weeks Pregnant?
Yes, your baby gets more fat at 29 weeks pregnant. The baby’s fat tissue starts transitioning from immature to mature fat cells at week 29. Subcutaneous fat begins to cover the body. The fat cells increasingly produce the CIDE-C (CIDEC) protein, which aids in fat storage and contributes to the baby’s growing weight.
The buildup of fat is crucial for brain and nervous system development in the third trimester as the fetal brain increases in size and cell number, requiring special fats known as long-chain polyunsaturated fatty acids (LC-PUFA), according to a 2021 study titled “Adipose tissue development and lipid metabolism in the human fetus: The 2020 perspective focusing on maternal diabetes and obesity,” by Gernot Desoye et al., published in Progress in Lipid Research.
Conditions such as gestational diabetes mellitus (GDM) and obesity in some mothers contribute to excess fat accumulation.
How to Identify What Position Your Baby Is In?
To identify what position your baby is in, attend a prenatal appointment to have an ultrasound scan. An ultrasound scan is the most reliable way to know your baby’s position, according to a 2014 study from the United Kingdom titled “Association between fetal position at onset of labor and mode of delivery: a prospective cohort study,” by A. Ahmad, published in Ultrasound in Obstetrics & Gynecology.
Ultrasound checks at 29 weeks pregnant provide precise details about your baby’s development and whether your baby is in a head-down, breech, or transverse position. Around 83% of fetuses are in the head-down position by week 29.
What Are The Changes In The Mother’s Body At 29 Weeks Pregnant?
Common changes in the mother’s body at 29 weeks pregnant include sleep disturbances, forgetfulness, lower back pain, hemorrhoids, and constipation. Here are 12 changes in the mother’s body at week 29.
- Sleep Disturbances: Pregnant women experience trouble sleeping, with insomnia resulting from factors like backache, frequent urination, and fetal movements.
- Forgetfulness: “Pregnancy brain” is a common symptom involving decreased memory and cognitive functions, partly due to more glucose being redirected to the growing fetus.
- Lower Back Pain: Hormonal changes and an expanding uterus lead to a dull ache in the lower back, spreading to the legs and worsening with specific movements.
- Piles (Hemorrhoids): Swollen veins in the rectal area cause discomfort, itching, and difficulty with bowel movements, often due to increased pressure from the growing uterus and constipation.
- Constipation: Hormonal changes slow intestinal activity, leading to infrequent bowel movements and difficulty passing stools.
- Restless Legs Syndrome (RLS) & Leg Cramps: Some women experience a strong urge to move their legs (RLS) and painful muscle contractions (leg cramps), particularly at night.
- GERD (Heartburn): Increased progesterone levels relax the esophageal sphincter, leading to acid reflux and discomfort.
- Bleeding and Swollen Gums: Hormonal changes cause inflammation and swelling in the gums, sometimes leading to bleeding, especially during oral hygiene routines.
- Headaches: Hormonal changes cause headaches, though the headache frequency typically decreases by the third trimester.
- Overactive Bladder: The growing uterus exerts pressure on the bladder, leading to frequent urination and sometimes incontinence.
- Fetal Movement (Quickening): The mother feels the baby kicking and moving frequently, with fetal movements becoming more pronounced.
- Prodromal Labor (Braxton-Hicks Contractions): Irregular, non-painful contractions prepare the body for labor but do not lead to childbirth.
How Big Is A 29-Week Pregnant Belly?
A 29-week pregnant belly has a fundal height of around 29 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 29-week-pregnant belly measures around 29 centimeters, between 27 to 31 centimeters. The expanding uterus grows to accommodate the growing fetus. The 29-week pregnant uterus has grown enough to be palpated above the navel level.
Several factors affect uterine size and growth rate, such as the mother’s body mass index (BMI), the number of prior pregnancies, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than women with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth in the past. The 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence of using the SFH to predict fetal health.
Do Contractions Occur Daily at 29 Weeks Pregnant?
No, contractions do not typically occur daily at 29 weeks pregnant. Frequent, painful contractions lasting longer than 60 seconds or occurring at least 4 times in 20 minutes likely indicate preterm labor, which is labor beginning before 37 weeks of pregnancy, according to a 2017 study titled “Preterm Labor and Birth Management: Recommendations from the European Association of Perinatal Medicine,” by G. C. Di Renzo et al., published in The Journal of Maternal-Fetal & Neonatal Medicine.
Braxton Hicks contractions (“practice contractions”) occur at 29 weeks and are a normal part of pregnancy, helping your body prepare for true labor. Braxton Hicks contractions are infrequent, irregular, and less intense than true labor contractions, lasting less than 60 seconds, causing no cervical changes.
Contact your OBGYN immediately if you experience unusual contractions or at shorter intervals with increasing intensity. Your OBGYN will perform necessary tests, check for cervical dilation, and likely perform an ultrasound. Preterm labor poses severe risks to you and your baby and warrants immediate attention.
Are Varicose Veins Common at 29 Weeks Pregnant?
Yes, varicose veins are common at 29 weeks pregnant, often visible as dark purple or blue under the skin. Increased blood flow during the third trimester places pressure on the leg’s large vein, making blood circulation difficult. Pressure from the expanding uterus affects blood circulation further. The resulting congestion causes expectant mothers to develop lumpy, swollen, and bluish leg veins, according to a 2010 study from Hungary titled “Varicose Veins of Lower Extremities in Pregnant Women and Birth Outcomes,” by Andrew E. Czeizel et al., published in Central European Journal of Public Health.
Varicose veins typically appear during the second trimester, peaking between months five and six and becoming more prominent as pregnancy progresses. The onset of varicose veins is influenced by maternal age and previous pregnancies.
What Are The Tips For Prenatal Care During Week 29?
Tips for prenatal care during week 29 of pregnancy include attending prenatal appointments and childbirth classes, monitoring blood sugar, and tracking fetal movement. Here are 7 tips for prenatal care during week 29 of pregnancy.
- Attend Appointments: Regular consultations with your OBGYN ensure consistent maternal and fetal health monitoring and address potential health issues. Having tailored advice from your healthcare provider is especially important as pregnancy progresses. Now is a great time to discuss childbirth preferences with your OBGYN and birth partner to ensure you’re prepared for upcoming tests and appointments.
- Monitor Blood Sugar: High blood sugar during pregnancy leads to gestational diabetes mellitus (GDM), posing risks like higher birth weight, delivery complications, and future health risks for the baby, such as childhood obesity and diabetes. Your healthcare provider will likely conduct a glucose tolerance test (GTT) and monitor your blood sugar if GDM is suspected. Maintaining a balanced lifestyle, including a nutritious diet and physical activity, supports blood sugar control.
- Track Fetal Movement: Maternal perception of fetal movements is the oldest and most common method for assessing fetal well-being. A noticeable decrease in fetal movement patterns sometimes indicates complications, such as stillbirth or fetal growth restriction. It’s important to remain attentive to your baby’s daily activity patterns and promptly alert your OB-GYN if you notice any drastic changes or movements suddenly stop.
- Attend Childbirth Classes: Childbirth classes provide you and your partner with essential knowledge about labor, delivery, and the weeks leading up to childbirth. Choose childbirth classes covering pain management, warning signs, and preparation for breastfeeding and parenting. Regular attendance in childbirth classes significantly reduces anxiety and increases confidence in natural childbirth.
- Practice Relaxation Techniques: Relaxation techniques such as deep breathing exercises and meditation help to manage stress. Incorporating rest into your day significantly reduces stress levels. Communicate your feelings with loved ones or therapists to help you prepare emotionally for the changes ahead.
- Engage in Physical Activity: Regular physical activity (PA) in your 29th week, such as walking, exercising, and swimming, helps manage pregnancy-related discomforts. Moderate PA improves overall health, boosts energy levels, enhances mood, and helps reduce common pregnancy issues, such as backaches. Follow a PA routine tailored to your body size at week 29 for a more enjoyable pregnancy experience.
- Maintain a Healthy Diet and Lifestyle: Eat a varied diet, including all food groups, to support your health and baby’s growth. Adequate calcium intake is crucial for your baby’s bone development. Stay hydrated by drinking plenty of liquids, and incorporate fiber-rich foods into your meals to maintain digestive health. Adjust your daily routine by shifting your work posture and avoiding heavy lifting to help ease pregnancy-related discomforts.

What Types Of Foods Are Beneficial To Eat During Week 29 Of Pregnancy?
Types of foods beneficial to eat during week 29 of pregnancy include sources from all food groups containing essential nutrients and vitamins like calcium, iron, and folic acid. Here are 15 particularly beneficial foods during week 29 of pregnancy.
- Calcium (1,000 milligrams for ages 19 to 50): Helps build strong bones and teeth. The best sources are yogurt, dark green leafy vegetables, and cheese.
- Iron (27 milligrams): Crucial for making red blood cells and delivering oxygen to your baby. Best sources: Lean red meat, dried beans, iron-fortified cereals.
- Iodine (220 micrograms): Essential for healthy brain development. Best sources: Dairy products, eggs, seafood.
- Choline (450 milligrams): Important for your baby’s brain and spinal cord development. The best sources are beef liver, soy products, and peanuts.
- Vitamin A (770 micrograms): Helps form red blood cells and utilize nutrients. The Best sources: Sweet potatoes, carrots, green leafy vegetables.
- Vitamin C (85 milligrams): Supports healthy gums, teeth, and bones. The best sources are Broccoli, strawberries, and citrus fruit.
- Vitamin D (600 international units): Vital for building bones and promoting healthy skin and eyesight.Best sources: Fatty fish like salmon and fortified milk.
- Vitamin B6 (1.9 milligrams): Assists in red blood cell formation and nutrient metabolism. The best sources are Whole-grain cereals, bananas, and pork.
- Vitamin B12 (2.6 micrograms): Supports the nervous system and red blood cell formation. The best sources are Milk, poultry, and fish.
- Folic Acid (400 micrograms): Important for preventing birth defects and supporting fetal growth. Best sources are Dark green leafy vegetables, enriched bread, and orange juice.
- Grains: Provide fiber, B vitamins, and iron. The best sources are Quinoa, oats, and brown rice.
- Fruits: Offer vitamins, minerals, and antioxidants. The best sources are Fresh fruit, dried fruit, and canned fruit.
- Vegetables: Packed with essential nutrients. The best sources are Frozen vegetables, raw vegetables, and 100% vegetable juice.
- Protein: Important for growth and development. The best sources are Poultry, eggs, and nuts.
- Dairy: Provides calcium, protein, and vitamin D. The best sources are Pasteurized milk, cheese, and yogurt.
Continue focusing on a balanced diet supporting your health and your baby’s development in week 29.
What Exercises Can You Do During Week 29 Of Pregnancy?
Exercises you can do during week 29 of pregnancy include the exercise recommended by the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Engage in at least 150 minutes of moderate-intensity aerobic activity and muscle-strengthening exercises weekly for significant health benefits. Here are 5 exercises appropriate for pregnancy.
- Walking: Low-impact exercise helps maintain cardiovascular health without putting undue stress on your joints. Walking uphill enhances muscle endurance.
- Swimming: Swimming is excellent during pregnancy. Summing supports your body weight and reduces strain on your back and joints, which is especially beneficial as your belly grows. Adapt different swimming styles for a full-body workout.
- Pelvic Floor Muscle Training: Strengthening your pelvic floor muscles daily helps prevent urinary incontinence and tones the muscles involved in labor, aiding in a smoother delivery.
- Stationary Bicycling: Stationary biking is a safe way to keep your heart rate up without the risk of falling, which is vital as your center of gravity shifts.
- Stretching: Gentle stretching helps maintain flexibility and alleviate discomfort from the physical changes in your body during week 29. Regular stretching improves your comfort during rest periods, whether at your work desk or on the sofa at home.
Remember to stay hydrated and distance yourself from activities involving a high risk of falling or heavy contact, especially as you enter the final trimester of pregnancy.
What Are The Things To Avoid At 29 Weeks Pregnant?
The things to avoid at 29 weeks pregnant include mind-altering substances like alcohol and drugs, smoking and secondhand smoke, caffeine, undercooked or raw meat and fish, and fish high in mercury. Here are 18 things to avoid at 29 weeks pregnant to ensure your health and your baby’s development.
- Alcohol: Consuming alcohol during pregnancy results in severe developmental issues and birth defects like fetal alcohol spectrum disorders (FASD). Completely avoid intake, as even small amounts of alcohol negatively impact your baby’s cognitive and behavioral development, as found in a 2020 study titled “Alcohol Use in Pregnancy” from Oregon Health and Science University and Oregon State University.
- Smoking and Secondhand Smoke: Smoking and secondhand smoking increases the risks of miscarriage, premature birth, and low birth weight, according to a 2020 study published in the International Journal of Environmental Research and Public Health, titled “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy.”
- Recreational Drugs: Avoid all recreational drugs which cause significant harm to your baby and lead to various health complications.
- Cannabis: Cannabis results in low birth weight and developmental delays, like other recreational drugs. Avoid cannabis entirely.
- Caffeine: Keep your caffeine intake below 200 mg per day. Excessive caffeine consumption is linked to an increased risk of miscarriage and low birth weight. Caffeine worsens heartburn, a common symptom during the third trimester.
- Certain Medications and Supplements: Consult with your healthcare provider before taking any medications, supplements, or herbal remedies, as some are harmful during pregnancy.
- High Mercury Fish: Do not consume high-mercury fish such as swordfish, king mackerel, tilefish, and shark to protect your baby’s developing nervous system.
- Undercooked or Raw Meat: Avoid consuming undercooked or raw meat to avoid infections like toxoplasmosis (a disease that causes fetal complications).
- Unwashed Vegetables and Fruits: Wash all fruits and vegetables thoroughly to prevent toxoplasmosis and other foodborne illnesses.
- Deli Meats: Do not eat deli meats unless thoroughly heated to avoid listeriosis, a dangerous foodborne bacterial illness for your baby.
- Unpasteurized Foods: Do not eat unpasteurized dairy products, soft cheeses, raw meat, undercooked meat, fish, or eggs to prevent exposure to harmful bacteria.
- Bagged Salads: Avoid pre-packaged salads, which sometimes contain harmful bacteria and pose risks during pregnancy.
- Iron Supplements: Only take iron supplements if prescribed by your healthcare provider, as unnecessary intake causes complications.
- Extreme Diets: Avoid restrictive or extreme diets, which disrupt hormone levels and affect your baby’s development. Try to eat little but often, focusing on nutritious foods to avoid sluggish digestion, gas, and constipation.
- Excessive Exercise: Avoid intense or excessive exercise, which negatively impacts hormone balance and causes complications.
- Strenuous Activities or Contact Sports: Steer clear of activities involving a high risk of falling, abdominal trauma, or heavy lifting to prevent injury to you and your baby.
- Exposure to Chemicals and Toxins: Minimize exposure to harmful chemicals and toxins from household cleaners, pesticides, and other products.
- Hot Tubs and Saunas: Avoid high temperatures in hot tubs and saunas, which can be harmful to your baby’s development.
Avoiding risks helps ensure a healthy and safe pregnancy. Seek medical advice from your OBGYN if you have concerns or questions.
How To Count Your Baby’s Kicks?
To count your baby’s kicks in week 29, lie down on your side or sit comfortably in a chair and count how long it takes to feel ten movements during a time when your baby is usually active, as recommended by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG).
Regular fetal movements typically indicate fetal well-being, while decreased fetal movement (DFM) signals potential complications, making fetal movement crucial for assessing fetal health and well-being. Focused counting while lying down is considered the most reliable, though different methods exist for counting fetal movements. More widely accepted guidelines for defining DFM are “10 movements in 10 hours”, or other thresholds based on older “Daily Movement Counts” methods, supported by more comprehensive evidence. Strictly adhering to the “10 movements in 2 hours” rule sometimes leads to unnecessary anxiety, as each pregnancy displays unique deviation from standard patterns. The time required to count ten kicks varies from less than 10 minutes to over 2.5 hours, for example, depending on the mother’s perception of movement.
Consult your OBGYN for counting methods, concerns about fetal activity, and reduced movements.
What Are The Possible Complications That Can Happen At 29 Weeks Pregnant?
Possible complications that can happen at 29 weeks pregnant include preterm birth, bleeding, hypertension and preeclampsia, severe headaches, gestational diabetes mellitus (GDM), and swelling. Here are 6 possible complications that can happen at 29 weeks pregnant.
- Preterm Birth: Preterm birth refers to the delivery of a baby before 37 weeks of pregnancy, occurring in approximately 12% of pregnant women. Signs of preterm birth include vaginal discharge, back pain, vaginal bleeding, and pelvic pressure. Risk factors for preterm birth include a history of preterm birth, specific infections, chronic conditions such as diabetes or high blood pressure, and lifestyle choices like smoking or inadequate prenatal care. Preterm birth is a leading cause of perinatal morbidity and mortality, often resulting in neurological complications for the baby.
- Bleeding: Vaginal bleeding in late pregnancy is associated with a few complications, requiring prompt evaluation by an obstetric care provider for diagnosis. Bleeding from the vagina in pregnancy doubles the risk of preterm birth. Risk factors for vaginal bleeding include a history of pregnancy complications, placental abruption, or placenta previa.
- Hypertension and Preeclampsia: Preeclampsia is a complication of pregnancy characterized by high blood pressure starting after the 20th week of pregnancy. Common signs of preeclampsia include headaches, vision changes, abdominal pain, and swelling. Preeclampsia is typically marked by a blood pressure reading of 140/90 or higher, protein in the urine (proteinuria), organ dysfunction, or placental dysfunction. Preeclampsia increases the mother’s risk of developing long-term high blood pressure 2- to 4-fold. Preeclampsia heightens the fetal risks of intrauterine growth restriction (IUGR), low amniotic fluid (oligohydramnios), preterm birth, and stillbirth in severe cases.
- Severe Headache: A severe headache is sometimes a significant complication at 29 weeks of pregnancy due to the possible presence of preeclampsia. Preeclampsia is a condition typically preceded by a headache and a flash of light feeling. About 2/3 of pregnant women with preeclampsia or eclampsia (seizure) noted experiencing severe headaches, according to a 2017 study titled “Headache and pregnancy: a systematic review.”
- Gestational Diabetes Mellitus (GDM): Gestational diabetes mellitus (GDM) involves high blood sugar levels during pregnancy and affects approximately 15% of pregnancies worldwide, according to a 2022 study titled “Gestational Diabetes Mellitus – Recent Literature Review.” GDM leads to complications like cardiovascular disease, obesity, and the development of type 2 diabetes in mother and baby. Untreated GDM often results in preeclampsia and sometimes pregnancy termination via Caesarean section.
- Swelling (Edema): Lower limb swelling (edema) frequently occurs during the third trimester. Increased blood volume, pressure from the growing uterus on the veins, weight gain, and hormonal changes complicate blood return to the heart, leading to water and salt buildup in the legs. Risk factors for developing edema include obesity and a lack of physical activity.
Self-diagnosing pregnancy complications is often inaccurate and dangerous. Consult your OBGYN or physicians if you notice any symptoms or have concerns. Early detection and intervention are keys to healthy and positive pregnancy outcomes.
Is Fetal Growth Infection Most Often Diagnosed at 29 Weeks in Pregnancy?
No, fetal growth restriction is not most often diagnosed at 29 weeks because multiple assessments are required weeks apart, starting in the first trimester, to correctly diagnose intrauterine growth restriction (IUGR), according to a 2016 study from India titled “Intrauterine Growth Restriction: Antenatal and Postnatal Aspects,” by Deepak Sharma, et al., published in Clinical Medicine Insights: Pediatrics. Reassessment is performed during the third trimester if a fetus is flagged during earlier assessments.
Intrauterine Growth Restriction (IUGR) is a condition in which fetal growth deviates from the expected pattern for gestational age. The pattern deviation indicates that the baby is not growing at a standard rate based on gestational age, gender, and race. Major contributing factors for IUGR include maternal age, hypertension, diabetes, substance abuse, infections, abnormal blood flow or dysfunction, chromosomal abnormalities, congenital diseases, and genetic factors.
IUGR poses several risks to the developing baby, including short-term risks like perinatal asphyxia, hypoglycemia, and respiratory distress. Long-term risks of IUGR include poor growth, cognitive impairments, and increased likelihood of adult-onset diseases like hypertension and type 2 diabetes.
Can Preterm Labor Occur at 29 Weeks Pregnant?
Yes, preterm labor can occur at 29 weeks pregnant. Preterm delivery (PTD) is when a baby is born between 22 and 37 weeks of pregnancy. Symptoms of preterm labor at 29 weeks include pelvic pain, vaginal discharge, back pain, and cramping similar to menstrual cramps.
The leading cause of preterm labor is an infection traveling from the lower genital tract to the uterus, causing the uterus to contract, membranes to break, and cervical changes, according to a 2017 study titled “Preterm Labor and Birth Management: Recommendations from the European Association of Perinatal Medicine,” by G. C. Di Renzo et al., published in The Journal of Maternal-Fetal & Neonatal Medicine. Other causes of preterm labor include a short cervix, carrying multiple babies, and various lifestyle and social factors.
OBGYNs typically measure the cervical length and use a transvaginal ultrasound to diagnose preterm labor. Cervical length measurements help in predicting preterm birth.
How Can A Partner Support The Mother At 29 Weeks Pregnant?
A partner can support the mother at 29 weeks pregnant by making lifestyle changes, displaying physical affection, offering mental support, taking on physical tasks, and offering reassurance. Here are 5 ways a partner can support the mother at 29 weeks pregnant.
- Lifestyle Changes: Encourage and participate in healthy habits together, such as avoiding smoking, adopting a balanced diet, and incorporating nutritious foods into your meals, to positively influence the mother’s well-being and support the baby’s healthy growth. Follow the doctor’s diet guide to make the best choices. Ensure smoking happens outside the home and consider joining a quitting program to protect the health of the mother and baby.
- Physical Affection: Offer your partner a hug and show your affection through small gestures of intimacy to help with discomfort and swelling. Acts of affection reduce partner stress and anxiety, enhance security, and promote well-being, according to a 2006 study, “Effective social support: Antecedents and consequences of partner support during pregnancy.”
- Mental Support: Offer your partner mental security by being present and encouraging during week 29 of pregnancy. Consistent support significantly reduces maternal distress during pregnancy. Help your partner feel more secure, confident, and informed by learning about pregnancy and helping her deal with the daily challenges of pregnancy.
- Take on Physical Tasks: Many physical activities become increasingly challenging for your partner at 29 weeks pregnant. Take over uncomfortable or unsafe physical tasks for your partner in the third trimester, including lifting heavy items, helping her sit or lie down, and assisting with housework. Supporting your partner alleviates physical strain and makes her more comfortable.
- Offer Reassurance: Remind her you are there for her and love her. Acknowledge pregnancy’s stress and changes and share your understanding and concerns about the baby and parenting.

What Prenatal Tests Are Needed At 29 Weeks Pregnant?
Prenatal tests at 29 weeks pregnant include blood pressure checks, urinalysis, amniocentesis, preeclampsia screening, ultrasound, and oral glucose tolerance test (OGTT).
Blood pressure checks monitor possible hypertension, and urinalysis detects protein in the urine to identify preeclampsia, a life-threatening pregnancy complication marked by high blood pressure.
Amniocentesis is a procedure where a sample of amniotic fluid is extracted from the uterus with a needle when chromosomal disorders are suspected, according to a 2019 study titled “The Complete Guide to Prenatal Testing,” conducted by Kiefer, A. et al. at the University of Wisconsin Hospital and published in Bloomlife. Ultrasound guides the needle to prevent contact with the fetus. The amniotic fluid is sent to a laboratory to analyze fetal cells for genetic abnormalities. Expect some pressure, pinching, or mild pain during the procedure.
Preeclampsia screening at 29 weeks includes a transvaginal ultrasound to check the uterine arteries. The patient lies supine (on the back) with legs raised after emptying the bladder, and a small ultrasound probe is gently inserted into the vagina. The technician measures the length of the cervix, checks blood flow in the uterine arteries, and looks for specific patterns indicating preeclampsia.
Ultrasound visualizes the fetus during pregnancy to determine fetal size, sex, and potential anomalies. A probe scans the abdomen, providing images of the fetus on a screen. The technician looks for specific markers to determine different characteristics of the fetus or potential concerns.
The oral glucose tolerance test (OGTT) involves having blood drawn after consuming a sugary drink to check how the body processes glucose. OGTT and urinalysis diagnose gestational diabetes mellitus (GDM). Expect to have blood drawn multiple times over 2-3 hours during the test.
When Should You Call Your Doctor If Something Feels Wrong At Week 29 Of Pregnancy?
Call your doctor if you feel something is wrong at week 29 of pregnancy or experience any of the following five complications.
- Decreased Fetal Movement: Decreased Fetal Movement (DFM) is a noticeable reduction in your baby’s movements. DFM during week 29 of pregnancy is sometimes indicative of stillbirth and growth concerns since fetal movements are expected to peak.
- Extreme/Sudden Swelling: Extreme swelling in the face and hands often indicates preeclampsia, a serious pregnancy condition characterized by high blood pressure. Additional symptoms of preeclampsia include persistent headaches, confusion, vision problems, and sudden weight gain. Preeclampsia has severe consequences for the mother and baby if left untreated.
- Fever/Chills: Some women, as many as 1 in 5, report experiencing a fever during pregnancy, according to a 2014 study from Denmark titled “Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring.” Elevated maternal body temperature during pregnancy, particularly 39°C (100.4°F) and over, increases the risk of fetal neural tube defects, congenital heart defects, and oral clefts.
- Vaginal Bleeding: Heavy and prolonged vaginal bleeding is typically associated with preterm labor. Multiple episodes of bleeding often result in low birth weight and delivery complications.
- Severe Abdominal Pain/Cramping: Severe abdominal pain indicates serious conditions like uterine complications. Seek urgent medical evaluation if you experience intense pain, heavy bleeding, or fainting, indicating a miscarriage or premature labor.
These symptoms are not exhaustive. Contact your OBGYN if you feel something is wrong, experience symptoms, or have concerns about your pregnancy.
What are the 29 weeks pregnant symptoms not to ignore?
29 weeks pregnant symptoms not to ignore include decreased fetal movement, sudden swelling, fever or chills, vaginal bleeding, and severe abdominal pain. Always trust your instincts during pregnancy. If something feels off at week twenty-nine, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins Needed To Be Taken During Week 29 Of pregnancy?
Yes, prenatal vitamins and supplements are recommended during week 29 of pregnancy for the baby’s development and maternal health. 10 vitamins and minerals to be taken during week 29 of pregnancy are outlined below, according to the American College of Obstetricians and Gynecologists (ACOG).
Calcium continues to be crucial, with a recommended intake of 1,000 milligrams for women aged 19 to 50. Calcium supports the development of a baby’s rapidly growing bones and teeth while maintaining the mother’s bone density.
Iodine, at 220 micrograms per day, continues to play a vital role in the baby’s brain development and supporting the mother’s thyroid function, which regulates metabolism and is critical for fetal growth.
Zinc supports the immune system and helps with cell growth and division, which are important as the pregnancy progresses.
Iron, with a recommended intake of 27 milligrams, helps prevent anemia by supporting the increased blood volume needed to supply oxygen to the mother and baby during the third trimester. Iron is particularly important as the baby’s brain develops and blood supply demands increase.
Choline needed at 450 milligrams daily, is essential for the ongoing development of the baby’s brain and spinal cord. Choline supports cognitive development and helps prevent neural tube defects.
Vitamin A, at 770 micrograms, is important for developing the baby’s skin, eyesight, and other organs. Vitamin A supports the formation of the baby’s heart, lungs, kidneys, and overall growth.
Vitamin C, recommended at 85 milligrams, aids in tissue repair, develops the baby’s immune system, and enhances iron absorption, which is increasingly important as pregnancy progresses.
Vitamin D, at 600 international units, supports the baby’s development of strong bones and teeth. Vitamin D helps the mother’s body absorb calcium more effectively, ensuring you and your baby have sufficient bone strength.
Vitamin B6, with a daily requirement of 1.9 milligrams, and Vitamin B12, at 2.6 micrograms, are necessary for red blood cell formation, brain development, and prevention of birth defects. Vitamin B6 also helps manage nausea, which some women still experience during the third trimester.
Finally, folic acid, recommended at 400 micrograms daily, is important for preventing neural tube defects, supporting the placenta, and overall fetal growth.
A balanced prenatal diet, rich in fruits, vegetables, whole grains, and lean proteins, is essential alongside prenatal vitamins. Always check with your healthcare provider to confirm you’re meeting all your nutritional needs for a healthy pregnancy.
What Does Parenting Styles Suggest About 29 Weeks Pregnant?
Parenting Styles offers 5 suggestions for the twenty-ninth week of pregnancy. First, choose a pediatrician for your baby. Research pediatricians in your area. Pay attention to their credentials, office hours, and overall approach to care. Look for a pediatrician who aligns with your values. Set up a get-to-know-you appointment with a pediatrician.
Second, prepare your hospital bag. Start thinking about what you need, such as comfortable clothing, toiletries, snacks, and baby essentials. You feel more organized and ready when the time comes.
“Think about what items make your stay comfortable and bring a sense of calm,” says Pamela Li, parenting specialist, Founder and Editor-in-Chief of Parenting Styles. “This personal touch makes a difference in your hospital experience.”
Third, organize baby gifts. If you’ve received baby shower gifts, take the time to organize them neatly and send the thank-you cards.
Fourth, choose your baby’s homecoming outfit. Pick out a special outfit for your baby’s first day home.
Lastly, prepare your postpartum wardrobe. Gather comfortable clothing that will work well during recovery and nursing, if applicable.
Congratulations on being 29 weeks pregnant!