30 Weeks Pregnant Symptoms: Week 30 Of Pregnancy And Prenatal Care
30 weeks pregnant symptoms include lower back pain, shortness of breath, Braxton-Hicks contractions, fatigue, skin changes, mood swings, and snoring. 30 weeks pregnancy symptoms often feel worse due to discomfort from the growing baby and hormonal changes.
Joint looseness and muscle strain cause lower back pain. The uterus pushing against the diaphragm leads to shortness of breath. Braxton-Hicks contractions prepare the body for labor without impacting the cervix. Hormonal shifts and physical demands increase fatigue. Skin changes like hyperpigmentation and stretch marks appear. Hormonal fluctuations trigger mood swings. Nasal swelling and pressure on the throat result in snoring.
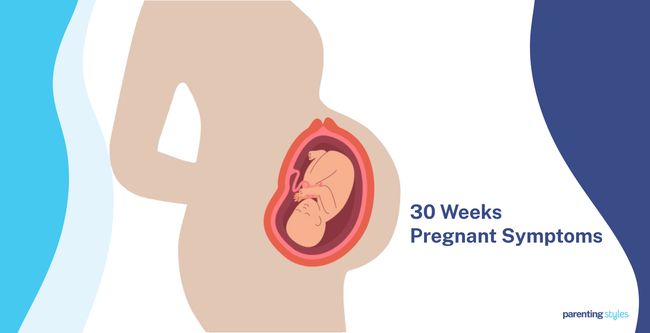
The 30-week-old baby weighs around 1,523 grams (3.36 pounds), about the size of a large cabbage, with lung and brain development progressing. Movements strengthen and respond to stimuli with coordinated eye movements and fully open eyelids. Lanugo sheds, thicker hair grows, fat develops for energy and heat regulation, and skin smooths with collagen. Lung development reaches the saccular stage. The head-down (cephalic) position is expected. Red blood cell production shifts to bone marrow. Brain connections control movement and senses.
Regular checkups and monitoring of the baby’s size and movements ensure proper prenatal care. Exercises like walking or stretching help manage symptoms, and support from a partner reduces anxiety caused by pregnancy.
What is 30 weeks pregnant in months? 30 weeks pregnant is 7 months and 2 weeks within the third trimester of pregnancy. You are in the middle of the eighth month of pregnancy.
What Are The Pregnancy Symptoms During Week 30?
Pregnancy symptoms during week 30 include lower back pain, shortness of breath, prodromal labor, fatigue, skin changes, mood swings, and snoring. Below are 30 weeks pregnancy symptoms.
- Lower Back Pain (Lumbar Pain): Lower back pain is a persistent discomfort in the lumbar area, often worsening upon tilting the pelvis forward. Lower back pain is due to joint looseness caused by hormonal changes, muscle strain from the baby’s growth, and decreased oxygenation from the compression of blood vessels. Lower back pain in pregnancy manifests as backaches restricting spinal movement and tenderness to the touch. Lumbopelvic pain begins around the 18th week of pregnancy and intensifies between weeks 24-36.
- Shortness of Breath (Dyspnea): Dyspnea is the feeling of running out of air or having difficulty breathing, resulting from the growing uterus pushing against the lungs and pressing on the diaphragm during pregnancy. Around 75% of pregnant women experience dyspnea upon exertion by week 30.
- Prodromal Labor (Braxton-Hicks Contractions): Braxton-Hicks contractions are intermittent uterine muscle contractions resembling mild menstrual cramps or abdominal tightening. Prodromal labor pains are practice contractions that help prepare the body for labor without causing the cervix to dilate. Braxton-Hicks contractions begin at week 6 of pregnancy, but most mothers only become aware of the sensation during the third trimester. Braxton-Hicks contractions are triggered by physical activity, a full bladder, and dehydration.
- Fatigue (Tiredness): Fatigue is the overwhelming feeling of tiredness and low energy, leading to difficulty performing routine activities. Pregnancy-associated fatigue is due to hormonal changes, increased blood volume, increased weight, and the demands of a growing baby’s needs. Sleeping problems typically associated with pregnancy further contribute to feelings of fatigue. About 60-90% of mothers experience fatigue, one of the four most frequently reported symptoms during all three trimesters of pregnancy, according to a 2017 study from The United States titled “Fatigue in Pregnancy,” conducted by Kwaghdoo Atsor Bossuah at Tennessee State University and published in International Journal of Childbirth Education.
- Skin Changes: Hyperpigmentation is the most common skin change reported during the third trimester. Pregnancy-associated stretch marks (striae distensae) appear as purple streaks from the 6th to 7th month of gestation, influenced by decreased calcium levels, altered immune response, and hormonal changes. About 90% of expectant mothers experience skin changes during pregnancy.
- Mood Swings: Mood swings are sudden, unpredictable changes in a pregnant woman’s emotional state and fluctuating feelings about her pregnancy and the baby. Mood swings in pregnancy are due to increased levels of stress hormones, estrogen, and progesterone, which cause the pregnant mother to feel more emotionally sensitive. It is not uncommon for pregnant women to experience mood swings and feelings of fear and anxiety, often from the start of pregnancy.
- Snoring: Snoring occurs when air passes through a relaxed throat, causing the soft tissues to vibrate and creating a noisy breathing sound as the person sleeps. Snoring during pregnancy is associated with hypertension and intrauterine growth retardation. Between 14%-23% of pregnant women experience snoring in the third trimester, compared to 4% of nonpregnant women.

What Is The Importance Of Understanding Being 30 Weeks Pregnant?
The importance of understanding being 30 weeks pregnant is to recognize you and your baby are undergoing significant changes. The baby increases in weight and is approximately the size of a large cabbage. The mother experiences lower back pain and shortness of breath due to the baby’s rapid growth. Fatigue and mood swings occur frequently at week 30 due to hormonal changes and physical demands. Gentle exercises and stress-relief techniques become increasingly important to manage physical and emotional changes.
Understanding Braxton-Hicks contractions, or prodromal labor, is essential as the due date nears. Distinguishing Braxton-Hicks from real labor contractions reduces the mother’s anxiety.
Maintaining a diet rich in essential nutrients is equally important to support the baby’s rapid brain and body development. Avoiding risky foods such as undercooked meats and soft cheeses minimizes the chance of infections.
Prenatal care is a continual priority, with regular OBGYN visits monitoring fetal growth and screening for potential complications such as pre-eclampsia becoming increasingly important. Routine tests like blood pressure monitoring and urine analysis are taken to ensure maternal and fetal health. Ultrasound scans are crucial during prenatal visits to assess the baby’s position and monitor organ development. Tracking the pregnancy week by week ensures antenatal visits are not missed.
What To Expect At 30 Weeks Pregnant?
A 30-week pregnant mother should expect several symptoms as the body adapts to the growing baby. Lower back pain occurs due to hormonal changes causing looser joints and the baby’s increasing weight. Shortness of breath happens because the uterus pushes against the diaphragm, making breathing difficult. Prodromal labor (Braxton-Hicks contractions) occurs to prepare the body for childbirth without affecting the cervix.
Fatigue increases due to hormonal shifts, additional blood volume, and the physical demands of carrying a larger baby. Discomfort often disrupts sleep, worsening tiredness. Stretch marks and hyperpigmentation are third-trimester symptoms that appear due to hormonal influences and skin stretching. Mood swings arise from fluctuating hormone levels, increasing emotional sensitivity. Snoring develops as nasal passages swell, and weight gain adds pressure on the throat, leading to nighttime breathing difficulties.
30-week-old baby (fetus) reaches the size of a large cabbage, weighing approximately 1,523 grams (3.36 pounds). Movements become more pronounced, with somersaults and kicks visible outside the belly. Key developments include improved eye movement, fat and hair growth, and continued lung and brain development. Babies usually position themselves head-down to prepare for birth.
Blood tests, Rh factor screening, and ultrasounds are taken to monitor the mother’s health and fetal development. Amniocentesis is performed to check for genetic conditions.
How Is The Baby Developing At 30 Weeks Pregnant?
The baby reaches the size of a large cabbage at 30 weeks of pregnancy, weighing around 1523 grams (3.36 pounds). Development includes specific measurements such as biparietal diameter (77 mm), head circumference (281 mm), abdominal circumference (260 mm), femur length (56 mm), and humerus length (51 mm).
Stronger and more varied movements occur, with babies responding to sounds, touch, and other stimuli. Movement becomes visible under the skin. Eye movements grow more coordinated, essential for vision control, and the eyelids remain fully open.
Lanugo, the fine protective hair, starts to shed as thicker hair grows on the scalp and other areas. Fat continues to develop, providing energy storage and regulating body heat. Skin matures, becoming smoother and more elastic due to collagen production.
Lung development progresses into the saccular stage, forming tiny air sacs to prepare the baby for breathing. Most babies assume the head-down, or cephalic, position by now, preparing for birth. Red blood cell production shifts from the liver to the bone marrow. Brain development accelerates, establishing connections controlling movement and senses such as vision.
How Big Is Your Baby At Week 30 Of Pregnancy?
Your 30-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 30-week-old fetus is about the size of a large cabbage. The 50th percentile measurements for 30-week fetal growth are as follows: the biparietal diameter (BPD) is 77 millimeters, the head circumference (HC) is 281 millimeters, the abdominal circumference (AC) is 260 millimeters, the femur length (FL) is 56 millimeters, and the humerus length (HL) is 51 millimeters.
The 30-week-old fetus weighs 1523 grams (53.72 ounces or 3.36 pounds), according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 30 Of Pregnancy?
Week 30 key developmental milestones include fetal movement, oculomotor control, hair growth, fat development, and skin development. Here are 9 key developmental milestones of babies at week 30 of pregnancy.
- Fetal Movement: Your baby performs various actions in the womb, including rolling, tumbling, and somersaulting. Fetal movement increases in strength, frequency, and variation from early in the third trimester, like week 30. The baby now moves in response to external stimuli, such as sounds, touch, and hunger cues. Many pregnant women report seeing the baby moving under her skin from weeks 28-32.
- Eye movement (Oculomotor Control): Oculomotor control refers to your baby’s ability to move the eyes and maintain visual stability. The first eye movements are observable on a 2D ultrasound at 14 weeks. The fetal eyes continue development during the early third trimester, with the eyelids partially opening by 28 weeks and fully opening by 30 weeks.
- Hair: Lanugo, the first type to develop in the fetus, is fine, soft, unpigmented hair that protects the baby from harmful substances in the amniotic fluid. Lanugo appears in the third month of pregnancy, helping anchor the vernix caseosa (a waxy protective coating) to the fetal skin. Lanugo starts to shed into the amniotic fluid in the third trimester and is eventually replaced by thicker hairs on the scalp, armpits, and genitals.
- Fat Development: Fat development (adipogenesis) involves the maturation of cells storing energy as fat (adipocytes). Fat tissue first appears from weeks 14-24 of gestation, helping regulate body heat and store energy. The fetus weighs about 1,523 g (3.36 lbs) at 30 weeks, according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine. Fat differentiation has likely already taken place in the fetal body since fat tissue differentiates in the head, neck, thorax, abdomen, and limbs when the fetus reaches a weight of around 625 g (1.38 lbs), according to a 1984 study from France titled “The chronology of adipose tissue appearance and distribution in the human fetus,” conducted by Stanley M. Garn et al. at The University of Michigan School of Public Health and published in Early Human Development.
- Skin: Fetal skin development at 30 weeks pregnant involves the continuous production of collagen, a protein that gives the skin a smoother and more elastic appearance. Collagen production begins at about week 5 of gestation when fine collagen fibrils develop in the fetus’ skin. Larger collagen fibrils assemble into bigger bundles as your baby grows. Approximately 18-21% of the fetus’ total collagen in the third trimester is type III collagen, which provides skin elasticity.
- Lung Development: The baby’s lungs are in the saccular stage of development at 30 weeks, when the smooth tubes in the lungs start breaking into ridges called crests. Crests turn into tiny air sacs, called saccules, which later become the alveoli. The walls of the lungs become thinner, and the surface area expands for gas exchange. Type II pneumocytes (special cells producing surfactant for the baby to breathe) mature during the saccular stage.
- Fetal Position: Fetal position refers to the baby’s orientation in the uterus. Most babies are in the cephalic position by week 30, head down and facing the uterus, with the chin tucked into the chest. Around 83% of babies positioned themselves head-down between weeks 29-32 of pregnancy in a 1985 study from the United States, titled “Fetal position during pregnancy,” conducted by Michael John Hughey, M.D. at Northwestern University School of Medicine and Evanston Hospital and published in American Journal of Obstetrics and Gynecology. A malpositioned fetus at week 30 has a 75% likelihood of switching to the cephalic position before delivery.
- Red Blood Cells: Fetal erythropoiesis (red blood cell production) increases to about 3-5 times the average adult levels during the third trimester to support the baby’s rapid growth. The bone marrow gradually takes over from the liver as the primary site of erythropoiesis, with red blood cell production in the liver entirely ceasing shortly after birth.
- Brain Development: The fetal brain establishes functional connections with the body in areas controlling senses and movement during week 30, enabling pain perception in the third trimester. Your baby’s brain transitions from random activity to more organized sleep states. The brain cells for vision start functioning, even without external stimulation, and essential brain structures for sight mature during REM (rapid eye movement) sleep.

How To Know If Your Baby Is Healthy During Week 30 Of Pregnancy?
To know if your 30-week-old baby is healthy, monitor your baby’s size and weight, amniotic fluid index, fetal lung volume, and attend prenatal checkups. Your healthcare provider will perform the necessary tests and scans. Here are 5 ways to tell if your baby is healthy during week 30 of pregnancy.
- Monitor Size and Weight: A 30-week-old baby is approximately the size of a cabbage. Regularly attend prenatal checkups to monitor your baby’s size and weight.
- Evaluate Amniotic Fluid Index: The Amniotic Fluid Index (AFI) evaluates fetal well-being by calculating the amount of amniotic fluid in the abdomen using a specific formula. A normal AFI ranges between 5 and 25 cm. An AFI below 5 cm suggests low amniotic fluid levels (oligohydramnios), while an AFI above 25 cm indicates excess (polyhydramnios). Abnormalities in AFI are associated with several complications, including problems in the baby’s placenta.
- Perform Ultrasonography: An ultrasound uses high-frequency sound to provide a clear view of your baby in the womb. A third-trimester ultrasound allows an OBGYN (obstetrician-gynecologist or OB-GYN) to observe the baby’s growth patterns, positions, and organ development, offering reassurance about your baby’s health.
- Measure Fetal Lung Volume: Fetal lung volume is used by OBGYNs to assess fetal growth. The average total fetal lung volume of a 30-week-old baby is 63.5 mL, according to a 2018 study from The United States, titled “Fetal Lung Volumes by MRI: Normal Weekly Values From 18 Through 38 Weeks’ Gestation,” conducted by Mariana L. Meyers et al. at Department of Pediatric Radiology, Children’s Hospital Colorado, University of Colorado Denver, and published in American Journal of Roentgenology. Measurements below 63.5 mL at week 30 suggest issues like underdeveloped lungs.
- Attend Prenatal Checkups: Prenatal checkups provide ongoing assessments of the mother and baby’s health. Prenatal visits allow healthcare providers to monitor the baby’s development and assess the mother’s well-being. A prenatal appointment in week 30 of pregnancy helps detect complications like preterm birth and fetal growth problems.
Does Lanugo In The Baby Start To Disappear At 30 Weeks Pregnant?
Yes, lanugo starts to disappear from your baby at around 30 weeks of pregnancy. Lanugo is the fine, soft, unpigmented hair characteristic of fetuses and newborns. Lanugo is the first type of hair to develop in humans, arising about 3 months into development.
Lanugo helps bind the vernix caseosa, a dense white covering, to the fetal skin until it falls out around 30-33 weeks of pregnancy, according to a 2013 study from Poland titled “Skin melanocytes: biology and development,” conducted by Mirosława Cichorek et al. at the Medical University of Gdansk and published in Advances in Dermatology and Allergology/Postępy Dermatologii i Alergologii. Vernix caseosa protects the fetus’s skin, prevents water loss, and plays a role in thermoregulation.
Lanugo is incorporated into the amniotic fluid upon shedding, eventually contributing to the composition of meconium (baby’s first stool). Lanugo is ultimately replaced by vellus (fine, thin hair) and terminal hair (thicker hairs on the scalp, axilla, and genitalia). Lanugo is present in about 30% of newborns at birth and sometimes indicates premature birth.
What Are The Changes In The Mother’s Body At 30 Weeks Pregnant?
The changes in the mother’s body at 30 weeks include lumbar pain, dyspnea, Braxton-Hicks contractions, fatigue, skin changes, mood swings, and snoring. Here are 7 changes in the mother’s body during week 30 of pregnancy.
- Lower Back Pain (Lumbar Pain): Joint looseness, muscle strain, and compression of blood vessels result in persistent discomfort in the lower back. Pain intensifies as pregnancy progresses, restricting movement and causing tenderness.
- Shortness of Breath (Dyspnea): Pressure on the lungs and diaphragm from the growing uterus causes breathing difficulties, particularly during exertion. Around 75% of pregnant women experience dyspnea by week 30.
- Prodromal Labor (Braxton-Hicks Contractions): Mild uterine contractions resembling menstrual cramps or abdominal tightening prepare the body for labor without causing cervical dilation.
- Fatigue (Tiredness): Hormonal changes, increased blood volume, and the physical demands of pregnancy create overwhelming tiredness. Sleep disruptions, affecting most mothers, further contribute to fatigue.
- Skin Changes: Hyperpigmentation and stretch marks (striae distensae) result from hormonal shifts and physical stretching of the skin. Nearly 90% of pregnant women experience skin changes.
- Mood Swings: Fluctuations in emotions, driven by elevated estrogen, progesterone, and stress hormones, increase sensitivity and prompt sudden shifts in mood.
- Snoring: Relaxation of throat tissues during sleep causes snoring, which becomes more frequent in the third trimester and is linked to hypertension and complications such as intrauterine growth retardation.
How Big Is A 30-Week Pregnant Belly?
A 30-week pregnant belly has a fundal height of around 30 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height correlates with the gestational age. Therefore, a 30-week-pregnant belly measures around 30 centimeters, between 28 to 32 centimeters. The expanding uterus grows to accommodate the growing fetus. The 30-week pregnant uterus has grown enough to be palpated above the navel level.
Uterine size and growth rate are affected by several factors, such as the mother’s body mass index (BMI), number of previous pregnancies, variations in the amount of amniotic fluid, or different fetal sizes. For example, women with higher BMI tend to have a slightly larger fundal height measurement than women with lower BMI.
Fundal height measurement has traditionally been used in clinical practice to monitor fetal growth. The World Health Organization (WHO) ANC Guidelines concluded in 2016 there is inadequate evidence for using the SFH to predict fetal health.
Is Your Baby More Active at 30 Weeks Pregnant?
Yes, your baby is more active at 30 weeks pregnant, becoming even more so as you approach full term. Your baby exhibits a marked increase in the strength, frequency, and variation of movements during the early third trimester. You’ll likely feel your baby moving more often and more intensely than before. Increased fetal movement is a positive sign, indicating the baby’s growing size, strength, and neurological system.
The baby’s movements evolve from simple flutters or kicks to a broader range of actions, including wriggling, pressing, rolling, kicking, flipping, tumbling, and even “dancing.” Some mothers describe feeling the baby jump as if startled or experiencing what feels like a spasm. Many pregnant mothers report making out the baby’s movement under the skin from weeks 28-32, according to a 2017 study from New Zealand titled “Maternal perception of fetal movements in the third trimester,” conducted by Billie Bradford et al. at Victoria University of Wellington and published in Women and Birth.
Mothers often observe a consistent increase in fetal activity later in the day, typically nearing bedtime, and report feeling babies respond to external stimuli such as sounds, touch, and even hunger cues in the third trimester.
How Often Do Contractions Occur at 30 Weeks Pregnant?
Contractions occur about 2.9 times per hour on average at 30 weeks pregnant, according to a 2005 study from The United States titled “Uterine Contraction Assessment,” conducted by Roger B. Newman, MD at the Medical University of South Carolina and published in Obstetric and Gynecological Clinics of North America. Contractions are typically infrequent for most women, though no contractions were observed 73% of the time, and there were three or fewer contractions per hour in 96% of cases in the study. Contractions gradually increase in frequency as pregnancy progresses, with a slight weekly increase in uterine activity after 30 weeks.
Normal uterine contractions are usually unnoticeable, constant, low-intensity contractions (Alvarez waves) or sporadic, higher-intensity contractions (Braxton-Hicks contractions). Braxton-Hicks contractions (“false labor” pains) are a normal part of pregnancy believed to prepare the uterus for labor. Braxton-Hicks contractions don’t lead to cervical dilation or birth but contribute to cervical softening and improving blood flow to the placenta.
Abnormal uterine contractility is typically characterized by a higher frequency of contractions, such as more than 5 contractions an hour at 30 weeks pregnant. Abnormal contractions sometimes indicate a higher risk of preterm labor and warrant further investigation.
What Are The Tips For Prenatal Care During Week 30?
The tips for prenatal care during week 30 include attending prenatal appointments, doing physical activity, getting physical comfort, maintaining a healthy diet, and attending childbirth education. Here are 6 tips for prenatal care during week 30.
- Attend Prenatal/OBGYN Appointments: Regular prenatal visits to an OBGYN (obstetrician-gynecologist or OB-GYN) are essential for monitoring maternal and fetal health. Prenatal appointments help assess fetal growth, identify potential risks early and offer opportunities to discuss important decisions, such as vaccinations during pregnancy. Prioritizing check-ups with your OBGYN promotes a healthy pregnancy and better outcomes for mother and child.
- Do Physical Activity: Staying fit during week 30 of pregnancy enhances maternal physical and psychological well-being. Stick to an exercise routine including walking, swimming, and pelvic floor exercises to promote better health outcomes for the baby. Stretching while sitting helps prevent complications like backache and cramps.
- Get Physical Comfort: Find comfortable sleeping positions, such as sleeping on your side, and prop your feet up when sitting, since discomfort increases as pregnancy progresses.
- Maintain a Healthy Diet: Prioritize nutrition and food safety during week 30 of pregnancy, as food-borne illnesses like listeriosis and toxoplasmosis pose dangers to maternal and fetal health. Avoid high-risk foods like soft cheeses, cold seafood, raw or undercooked meats, and pre-prepared salads. Avoid substances like alcohol, caffeine, and smoking, which negatively impact your health and the health of your baby.
- Attend Childbirth Education: Participate in childbirth education classes to understand labor, delivery, pain management options, and coping strategies. Make a checklist addressing essential topics and preparations. Learn how to prepare your body for the physical demands of giving birth.
What Types Of Foods Are Beneficial To Eat During Week 30 Of Pregnancy?
Types of foods beneficial to eat during week 30 of pregnancy include a nutrient-rich diet to support your health and your baby’s development. Here are 15 types of beneficial foods to include in your diet at week 30.
- Calcium (1,000 mg): Essential for your baby’s bone development. Include yogurt, sardines, dark green leafy vegetables, broccoli, and kale.
- Iron (27 milligrams): Important for preventing anemia and supporting increased blood volume. Lean red meat, prune juice, iron-fortified cereals, lentils, chickpeas, and beans are good sources of iron.
- Iodine (220 micrograms): Vital for your baby’s brain development. Consume iodized table salt, dairy products, eggs, and seafood like salmon.
- Choline (450 milligrams): Supports brain and spinal cord development. Try foods like beef liver, peanuts, soy products, and eggs.
- Vitamin A (770 micrograms): Helps with cell growth and the immune system. Consume sweet potatoes, carrots, and green leafy vegetables.
- Vitamin C (85 milligrams): Important for skin health and iron absorption. Eat foods like strawberries, broccoli, oranges, mango, and tomatoes.
- Vitamin D (600 international units): Supports bone health and immune function. Include fortified milk, salmon, and egg yolks.
- Vitamin B6 (1.9 milligrams): Helps with metabolism and brain development. Good sources are bananas, whole-grain cereals, pork, and nuts like cashews.
- Vitamin B12 (2.6 micrograms): Essential for nerve function and red blood cell formation. Include fish, poultry, milk, and lean meats.
- Folic Acid (400 micrograms): Crucial for preventing neural tube defects. Include dark green leafy vegetables, orange juice, enriched bread and pasta, and whole grains.
- Grains: Try quinoa, brown rice, oats, and whole-wheat pasta for energy and other essential nutrients.
- Fruits: Eat fresh, frozen, dried fruits and whole fruits like apples, berries, and bananas to get vitamins, minerals, and fiber.
- Vegetables: Incorporate raw, frozen, or dried vegetables into your meals for essential nutrients, including dark green vegetables.
- Protein: Eat eggs, beans, seafood, lean meats, and lentils to meet your protein and iron needs.
- Dairy: Consume cheese, milk, and yogurt for calcium, vitamin D, and probiotics.
Eating a balanced diet during the 30th week of pregnancy ensures you and your baby get the nutrients necessary for healthy development. Be mindful of caffeine and alcohol intake during pregnancy to prevent development complications.
What Exercises Can You Do During Week 30 of Pregnancy?
Exercises you can do during week 30 of pregnancy include walking, swimming, pelvic floor exercises, stretching, and stationary cycling, as recommended by the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Here are 5 exercises you can perform during your 30th week of pregnancy.
- Walking: Walking is a low-impact activity that benefits cardiovascular health and overall fitness. Try brisk walking for at least 30 minutes at a moderate intensity.
- Swimming: Swimming offers a full-body workout without straining your joints. The water helps to support your extra weight, making swimming one of the safest and most productive activities during pregnancy.
- Pelvic Floor Exercises (Kegels): Kegels strengthen the muscles supporting your bladder, uterus, and bowels, helping to reduce the risk of urinary incontinence. Pelvic floor exercises help manage labor pain, becoming especially important as your body prepares for childbirth.
- Stretching: Gentle stretching exercises help alleviate tension, improve flexibility, and enhance range of motion. Stretches like the mermaid stretch and side leg raises further help with muscle relaxation and preparation for labor.
- Stationary Cycling: Riding a stationary exercise bike provides a safe, low-impact cardiovascular workout to maintain fitness levels. Indoor stationary bicycling is particularly suitable, eliminating the risks associated with outdoor cycling.
Do at least 150 minutes of moderate-intensity aerobic and muscle-strengthening activities each week. Start slowly, listen to your body, and gradually increase the intensity and duration of your exercises. Avoid overheating, high-risk activities, and high-impact exercises to prevent complications.
What Are The Things To Avoid At 30 Weeks Pregnant?
Things to avoid at 30 weeks pregnant include alcohol, smoking, recreational drugs, caffeine, and certain medications and supplements. Here are 18 things to avoid during 30 weeks of pregnancy.
- Alcohol: Alcohol causes significant developmental issues and birth defects like fetal alcohol spectrum disorders (FASD). Avoid alcohol intake as even minimal alcohol consumption during pregnancy negatively affects fetal cognitive and behavioral development, according to a 2020 study titled “Alcohol Use in Pregnancy,” conducted at Oregon Health and Science University and Oregon State University and published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Smoking increases the risk of complications such as miscarriage, preterm birth, and low birth weight. The dangers of smoking during pregnancy were highlighted in a 2020 study, “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy: A Pragmatic Overview of Reviews of Maternal and Child Outcomes, Effectiveness of Interventions and Barriers and Facilitators to Quitting,” published in the International Journal of Environmental Research and Public Health by Gillian S. Gould and colleagues.
- Recreational Drugs: Recreational drug use leads to severe health issues for your developing baby, including developmental delays and other long-term effects. Misuse of tramadol was associated with congenital malformation in a 2019 study titled “Effects of unconventional recreational drug use in pregnancy.”
- Cannabis: Cannabis use during pregnancy is linked to low birth weight and developmental complications, similar to other recreational drugs. Cannabis is associated with the development of mental disorders such as Attention Deficit Hyperactivity Disorder (ADHD) and depression, according to a 2020 study titled “Cannabis use during pregnancy and its relationship with fetal developmental outcomes and psychiatric disorders. A systematic review.”
- Excessive Caffeine: Limit your caffeine intake to 200mg daily to reduce the risk of miscarriage and low birth weight, though moderate caffeine consumption is generally considered safe.
- Certain Medications and Supplements: Consult with your healthcare provider before taking any medications, supplements, or herbal remedies, as some pose risks during pregnancy.
- High Mercury Fish: Avoid eating fish high in mercury, such as swordfish, king mackerel, tilefish, marlin, and shark, as mercury harms your baby’s developing nervous system.
- Undercooked or Raw Meat: Avoid consuming undercooked or raw meat or fish to reduce the risk of infections like toxoplasmosis and listeriosis, which are harmful to your baby.
- Unwashed Vegetables and Fruits: Ensure all fruits and vegetables are thoroughly washed before eating to prevent exposure to harmful bacteria and parasites.
- Deli Meats: To reduce the risk of listeriosis, avoid eating deli or cold meats unless they are heated to steaming hot.
- Unpasteurized Foods: Avoid unpasteurized juices and dairy products such as soft cheeses like brie and feta, which carry harmful bacteria.
- Bagged Salads: Avoid pre-packaged salads or ensure thorough washing, as bagged salads sometimes carry bacteria.
- Strenuous Activities or Contact Sports: Avoid activities that involve a high risk of falling or abdominal injury, heavy lifting, or contact sports.
- Exposure to Chemicals and Toxins: Limit exposure to household cleaners, pesticides, and other chemicals that can be harmful during pregnancy.
- Hot Tubs and Saunas: Avoid hot tubs and saunas, as elevated temperatures can harm your developing baby and increase the risk of overheating.
- Stress: Actively manage and reduce stress through relaxation techniques, as chronic stress negatively impacts you and your baby.
- Hair Dye: Avoid chemical hair treatments. Talk to your OBGYN about concerns, or consider natural alternatives.
- Eating Habits: Avoid foods triggering heartburn, such as fried foods, spicy foods, chocolates, and citrus fruits. Eat small, frequent meals and avoid lying down immediately after eating to prevent indigestion.
Avoid risks and follow your healthcare provider’s advice to ensure a safe and healthy pregnancy for you and your baby at 30 weeks.
What Is The Best Sleeping Position For Mothers At 30 Weeks Pregnant?
The recommended sleeping position for mothers at 30 weeks pregnant is on the left side, as sleeping on the left side helps maintain optimal blood flow to the mother and the baby, reducing the risks associated with decreased circulation, according to a 2017 study, “Going to sleep in the supine position is a modifiable risk factor for late pregnancy stillbirth; Findings from the New Zealand multicentre stillbirth case-control study,” by Lesley M. E. McCowan et al., published in PLoS ONE.
Sleeping on the back (supine position) is linked to several health risks, including decreased maternal cardiac output and uterine blood flow and a higher likelihood of pregnancy complications such as hypertensive disorders, gestational diabetes, and fetal growth restriction. The study further observed how babies spend less time in an active behavioral state when the mother sleeps on her back, indicating a reduced blood supply to the fetus in the supine position. Interventions encouraging women to avoid supine sleeping reduce the risk of stillbirth by approximately 9%.
What Can You Do To Prepare For Labor At 30 Weeks Pregnant?
To prepare for labor at 30 weeks pregnant, attend childbirth classes and prepare a birth plan.
Childbirth preparation classes, often led by midwives, provide information about pregnancy, labor, and early parenthood. The class curriculum usually includes topics like fetal development, warning signs during pregnancy, different stages of labor, pain relief techniques, breathing exercises, and postpartum preparation for breastfeeding and newborn care.
A birth plan is a document communicating your preferences for labor and delivery with your healthcare team. Childbirth preparation classes help you determine your preferences regarding pain management, potential labor interventions, and ideal birthing positions, which are included in your plan.
Labor and delivery are unpredictable processes, often causing anxiety in pregnant women. Childbirth education reduces anxiety and increases confidence, with women who attended childbirth classes regularly reporting better labor and pain management, according to a 2009 study from the United States titled “Primiparous women’s knowledge and satisfaction based on their attendance at childbirth preparation classes,” by Lisa Hanson, CNM, PhD et al., published in the Journal of Midwifery Womens Health.
What Are The Possible Complications That Can Happen At 30 Weeks Pregnant?
Possible complications that can happen at 30 weeks pregnant include swelling, urinary tract infection, pemphigoid gestationis, stillbirth, intrauterine growth restriction, and mood and anxiety disorder. Here are six complications experienced during week 30 of pregnancy:
- Swelling (Edema): Pregnant women are prone to swollen hands and feet (edema) due to excess fluid buildup in the upper and lower limbs. Common signs of edema include heaviness, pain, and a bursting feeling in the legs. Risk factors for edema include poor blood flow in the veins, blood clots, high blood pressure, diabetes, and lack of physical activity.
- Urinary Tract Infection (UTI): Pregnant women are more prone to UTIs due to hormonal changes. Symptoms include burning sensations when urinating, cloudy urine, and frequent urination. Contact your OBGYN for treatment to avoid kidney infection and preterm labor.
- Pemphigoid Gestationis (PG, Gestational Pemphigoid): Pemphigoid gestationis (PG) is a skin disorder that causes blistering of the skin and mucosal membranes. Symptoms include intense abdominal itching around the navel, followed by blistering. PG is most common during the second and third trimesters and is associated with fetal growth restriction and prematurity.
- Stillbirth: Stillbirth occurs when a pregnancy ends after 20 weeks, while a loss before 20 weeks is called a miscarriage. Symptoms of stillbirth include a sudden decrease in fetal movement or no movement at all. Complications following a stillbirth include parental emotional distress and potential health concerns for the mother, such as infection. Risks for stillbirth include high blood pressure, diabetes, and complications with the placenta. Regular prenatal care and monitoring help manage risks for stillbirth and identify potential issues early.
- Intrauterine Growth Restriction (IUGR): IUGR occurs when a baby does not develop adequately in the womb due to insufficient blood flow or placental issues. IUGR leads to low fetal birth weight and an increased risk of health complications, including neonatal death. Proper management of IUGR ensures the necessary support for mother and baby during and after delivery.
- Mood and Anxiety Disorder: Symptoms of mood and anxiety disorder in pregnant women include sleep changes, constant worrying, and mood swings. Depression and anxiety during pregnancy negatively affect maternal bonding with the fetus and lead to postnatal depression, according to a 2015 study titled “The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review.” Physical consequences include low birth weight and preterm birth.

Can Preterm Labor Occur at 30 Weeks Pregnant?
Yes, preterm labor can occur at 30 weeks pregnant. Preterm labor is defined as regular uterine contractions leading to cervical dilations of 2cm or more before the 37th week of pregnancy.
Spontaneous preterm labor and birth occur when the cervix dilates, natural contractions begin, and the amniotic sac ruptures prematurely, a condition known as premature preterm rupture of membranes (PPROM). About 75% of preterm births are categorized as spontaneous preterm labor, according to a 2020 study from The United States titled “Preterm Labor and Birth,” by Kellie M Griggs et al., published in the American Journal of Maternal/Child Nursing. In contrast, some cases of preterm labor are medically induced (iatrogenic) due to pregnancy complications.
Symptoms of acute preterm labor include frequent, often painless contractions, menstrual-like cramps, or feeling like your baby is “balling up.” Some women notice increased discharge, a trickle or gush of fluid, and watery, mucus-like, or bloody discharge. Other signs include persistent dull backaches and pressure in the pelvis or lower abdomen. Risk factors for preterm labor include maternal age, chronic stress, hypertensive disorders, cervical insufficiency, and fetal anomalies.
How Can A Partner Support The Mother At 30 Weeks Pregnant?
A partner can support the mother at 30 weeks pregnant through physical task assistance, emotional support, mental support, healthy activities, and pregnancy education. Here are 5 ways a partner can support the mother at 30 weeks.
- Physical Tasks Assistance: Physical tasks become challenging around week 30 of pregnancy. Take on tasks involving heavy lifting, like carrying groceries or moving furniture. Help pack the hospital bag and handle most household chores, including cleaning, cooking, and laundry, to relieve physical strain. Practical support eases the mother’s discomfort and shows your commitment to preparing for the baby’s arrival.
- Emotional Support: Support your partner by actively listening and being present during stressful times. Reading pregnancy books together provides valuable insights and opens up conversations, helping you feel more prepared for the journey ahead. Celebrate milestones like reaching 30 weeks to help reduce prenatal anxiety and offer gestures like holding hands to help foster emotional well-being.
- Mental Support: Offer your partner mental security by being present and creating a stable, safe environment. Consistent support reduces maternal distress, helping mothers feel more secure and confident. Avoid complaints and complete tasks out of love and compassion, which contribute to effective support, according to a 2020 study titled, “Active husband involvement during pregnancy: a grounded theory. family relations.”
- Healthy Activities Together: Commit to joining the mother for healthy activities like walking or swimming exercises.
- Pregnancy Education: Research pregnancy stages and baby’s development together. Attend prenatal appointments together, ask about prenatal tests, and recognize common symptoms and complications during week 30 of pregnancy.
What Prenatal Tests Are Needed At 30 Weeks Pregnant?
Prenatal tests needed at 30 weeks pregnant include blood tests, Rh status assessment, amniocentesis, screening for Pre-eclampsia, and ultrasound scans.
Blood tests are often necessary for high-risk patients around week 30 of pregnancy in preparation for the management of potential complications. The relevant urine and blood tests are taken to screen for human immunodeficiency virus (HIV), syphilis, and chlamydia, typically between 28-36 weeks.
Rhesus (Rh) disease occurs when a mother who is Rh-negative (lacking a specific protein in the red blood cells) carries a baby with a positive Rh factor (who has the protein). The mother’s immune system becomes sensitized to the Rh protein, producing antibodies against Rh, which cross the placenta and attack the baby’s red blood cells. Rh incompatibility is tested through Rh status assessment. Positive screens are confirmed through a Kleihauer-Betke (KB) test. The KB test determines the amount of fetal blood in maternal circulation to prepare for further action.
Amniocentesis is performed anytime after 15 weeks of pregnancy to test the amniotic fluid for genetic disorders like cystic fibrosis, neural tube defects like spinal muscular atrophy, or intra-amniotic fetal infection. The process of amniocentesis is minimally invasive, involving a sterile needle being carefully inserted into the abdomen with the guidance of an ultrasound to collect fluid from the amniotic sac.
Pre-eclampsia screening at 30 weeks involves several tests assessing pregnancy-induced hypertension. Laboratory tests evaluate protein and creatinine levels in the urine, indicating proteinuria, a key sign of pre-eclampsia. A complete blood count monitors platelet levels, and a complete metabolic panel checks liver and kidney function. Management and monitoring of maternal blood pressure are essential for effective screening and managing pre-eclampsia in pregnancy. However, elevated blood pressure alone isn’t a definitive indicator of pre-eclampsia.
Ultrasound scans are imaging tests utilizing sound waves to visualize images inside the body, such as your baby’s shape, size, and position. Ultrasound scans help determine prenatal sex by visualizing fetal genitals and pelvic structures by the third trimester. Fetal sex determination by ultrasound is more accurate after the first trimester, with an accuracy rate ranging from 93% to 99% in the second and third trimesters, according to a 2012 study titled “The accuracy of 2D ultrasound prenatal sex determination” by Blessing Ose-Emenim Igbinedion et al., published in Nigerian Medical Journal.
When To Call For Your Doctor If Something Feels Wrong At Week 30 Of Pregnancy?
Call your doctor if you feel something is wrong at week 30 of pregnancy or experience any of the following four issues.
- Decreased Fetal Movement: Unusual changes in your baby’s movement in week thirty require immediate attention. A noticeable decrease in fetal movement sometimes signals complications, such as fetal growth restriction or stillbirth. Monitor your baby’s movements daily, and call your OBGYN or healthcare provider if you observe fewer than ten movements in an hour.
- Persistent Headaches with Vision Changes: Headaches are common among pregnant women. Persistent headaches accompanied by blurred signs likely indicate preeclampsia (high blood pressure after 20 weeks gestation). Preeclampsia leads to severe complications if left untreated. Contact your OBGYN immediately if you experience recurring headaches, vision changes, and severe swelling.
- Fever Over 100.4°F (38°C): A fever over 100.4°F is a sign of infection and must not be ignored. Contact your healthcare provider immediately if you experience chills and fever, which sometimes lead to neural tube defects, congenital heart defects, and oral clefts, based on a 2014 study, “Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring,” conducted by Anne-Marie Nybo Andersen, Gabriele Berg-Beckhoff, and Julie Werenberg Dreier and published in Pediatrics.
- Severe Abdominal Cramping: Severe abdominal cramping without diarrhea at 30 weeks of pregnancy is a symptom of preterm labor. Contact your OBGYN immediately if abdominal cramping is accompanied by vaginal bleeding, fluid leakage, pelvic pressure, low backache, or contractions every 10 minutes or more.
- Mood or Anxiety Disorders: Mood and anxiety disorders like major depressive disorder and generalized anxiety disorder (GAD) affect 60% of women throughout pregnancy. Contact your OBGYN if you experience distress, elevated stress or anxiety, or thoughts of harming yourself.
What are the 30 weeks pregnant symptoms not to ignore? 30 weeks pregnant symptoms not to ignore include decreased fetal movement, persistent headaches with vision changes, fever over 100.4°F, severe abdominal cramping, and mood or anxiety disorders. Always trust your instincts during pregnancy. If something feels off, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms during week thirty that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins Needed To Be Taken During Week 30 Of Pregnancy?
Yes, some specific prenatal vitamins and minerals must be taken during week 30 of pregnancy to support maternal health and fetal development, as outlined by the American College of Obstetricians and Gynecologists (ACOG).
Calcium, at a recommended dosage of 1,000 milligrams for ages 19-50, is vital in maintaining bone health as the baby’s skeletal development accelerates.
Vitamin D, at 600 international units, helps the body to use calcium effectively, assisting with the baby’s bones and teeth development.
Iron, recommended at 27 milligrams daily, supports the increased blood volume during pregnancy. Iron delivers oxygen and nutrients to the fetus, which is necessary for preventing anemia and preparing for childbirth.
Iodine, at 220 micrograms, is necessary for the continued healthy development of the baby’s brain and nervous system. Iodine supports thyroid function, which is essential for overall growth and neurological development.
Choline intake, at 450 milligrams daily, supports the ongoing development of the baby’s brain and spinal cord and prevents certain birth defects.
Folic acid, at 400 micrograms daily, helps prevent neural tube defects and supports the baby’s overall central nervous system development.
Vitamin A, at 770 micrograms, aids in fetal organ development, including the heart, lungs, and kidneys, and maintains healthy skin and eyesight.
Vitamin C, recommended at 85 milligrams, helps form connective tissue, supports the immune system, and enhances iron absorption.
Vitamin B6, at 1.9 milligrams, plays a role in red blood cell formation, is vital for the baby’s brain development, and helps manage pregnancy-related nausea.
Vitamin B12, recommended at 2.6 micrograms, helps maintain the nervous system and supports red blood cell production. Vitamin B12 helps prevent certain birth defects and supports overall fetal development.
Consult with your healthcare provider to ensure you’re taking the right vitamins and to discuss any additional supplements you need.
What Does Parenting Styles Suggest About 30 Weeks Pregnant?
Parenting Styles suggests expecting parents take a childbirth class by week 30 of pregnancy if they haven’t already done so. Childbirth classes provide essential information about the stages of labor, pain management options, and practical tips for both the mother and her support team. Childbirth classes offer an excellent opportunity to ask questions, dispel fears, and connect with other expecting parents.
“Taking a childbirth class by week 30 is one of the best ways to mentally and physically prepare yourself for labor. It’s not just about learning the stages of childbirth—it’s about feeling confident, informed, and ready for the life-changing moment ahead. Many classes offer hands-on practice for techniques like breathing exercises and different birthing positions, which can make a real difference when the big day arrives,” says Pamela Li, Founder and Editor-in-Chief of Parenting Styles.
Congratulations on being 30 weeks pregnant!