33 Weeks Pregnant Symptoms: Week 33 Of Pregnancy And Prenatal Care
33 weeks pregnant symptoms include pelvic girdle pain, Braxton Hicks contractions, insomnia, wrist pain, and vaginal swelling. 33 weeks pregnancy symptoms involve discomfort in the pelvis due to joint loosening and Braxton Hicks contractions, which are irregular and painless but prepare the body for labor. Insomnia, aggravated by hormonal changes and discomfort, is common, and wrist pain may result from carpal tunnel syndrome due to fluid retention. Vaginal swelling occurs from increased blood flow and pressure, and frequent urination happens as the baby presses on the bladder. Shortness of breath also develops due to the growing uterus limiting lung capacity. Forgetfulness, often called “pregnancy brain,” and swelling in the ankles and feet are frequent symptoms, along with general body aches from increased weight and shifting posture.
Monitoring these symptoms and the baby’s development is critical for maintaining health during this stage of pregnancy.

A 33-week-old (third trimester) baby is the size of a pineapple, with key systems like the nervous and immune systems maturing rapidly. Sensory abilities like responding to light and sound improve. The baby’s bones harden as calcium is transferred from the mother, and the immune system receives antibodies to protect the baby after birth.
Regular prenatal appointments are essential to monitor the baby’s development and prevent complications such as preeclampsia. Staying active with safe exercises like walking or swimming and maintaining a healthy diet rich in calcium and omega-3 fatty acids supports both mother and baby’s health during this stage.
What is 33 weeks pregnant in months? 33 weeks pregnant is 8 months and 1 week within the third trimester. You have started the ninth month of pregnancy.
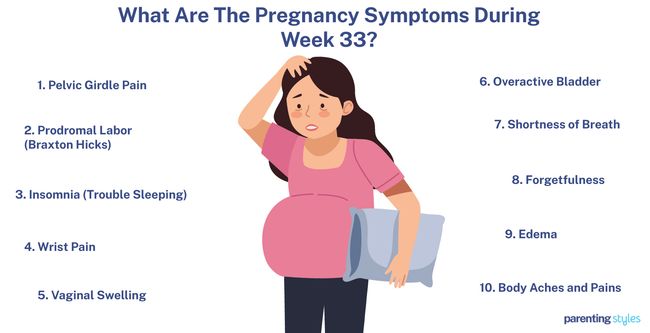
What Are The Pregnancy Symptoms During Week 33?
33 Weeks pregnant symptoms include pelvic girdle pain, Braxton Hicks contractions, insomnia, wrist pain, and vaginal swelling. Below are common 33 weeks pregnancy symptoms.
- Pelvic Girdle Pain: Pelvic girdle pain is characterized by stabbing, dull, shooting, or burning sensations in the pelvic area, sometimes radiating to the posterior thigh, perineum, or groin. Pregnancy-related pelvic girdle pain (PPGP) is commonly caused by inflammation, joint relaxation, insufficiency, or instability in the pelvic region. PPGP affects 16% to 25% of pregnant women, with symptoms peaking in the third trimester, particularly between weeks 24 and 36 of pregnancy, according to a 2011 study titled “Pregnancy-related pelvic girdle pain: an update,” by Nikolaos K Kanakaris et al., published in BMC Medicine.
- Prodromal Labor (Braxton Hicks): Braxton Hicks contractions are mild, painless contractions typically occurring during the second and third trimesters of pregnancy. Braxton Hicks contractions result from the tightening and relaxing of uterine muscle fibers and are a natural part of pregnancy, helping the body gradually prepare for labor. The contractions are irregular, usually lasting less than 30 seconds, though they can extend up to 2 minutes. In contrast, true labor contractions are more regular and last between 30 and 90 seconds.
- Insomnia (Trouble Sleeping): Insomnia is a sleep disorder characterized by difficulty falling or staying asleep and waking up too early. Hormonal fluctuations and changes in sleep patterns during pregnancy often worsen insomnia, particularly in the third trimester. Insomnia is associated with an increased risk of pregnancy complications, including high blood pressure, elevated labor pain, preterm birth, and both prenatal and postpartum depression. Approximately 23.7% of pregnant women reported difficulty falling asleep during the third trimester in a 2015 study titled “Insomnia and sleep deficiency in pregnancy,” by Cristina Reichner, published in Obstetric Medicine.
- Wrist Pain: Most cases of wrist pain during the third trimester of pregnancy are linked to Carpal Tunnel Syndrome (CTS), which occurs when pressure on a nerve affects hand and wrist motor function. De Quervain Tenosynovitis is another common type of wrist pain, often surfacing around 33 weeks of pregnancy, causing pain and swelling in the thumb due to irritated tendons. Many pregnant women report tingling sensations in their hands and difficulty carrying items like shopping bags. Symptoms of wrist pain typically result from postural changes, hormonal fluctuations, weight gain, and fluid retention. Approximately 67.4% of pregnant women experience wrist pain.
- Vaginal Swelling: Vaginal swelling during pregnancy is characterized by the dilation of vulvar varicosities (varicose veins in the vulva) and pudendal veins, often resulting in intense pain around the swollen veins. The increased blood volume and pressure from the growing uterus place additional strain on the pelvic veins, leading to venous reflux—where blood flows backward and pools in the veins. The impaired blood flow in the veins of the pelvis contributes to swelling in the vulvar region. Vulvar varicosities are estimated to affect 18%–22% of pregnant women, typically occurring in the second and third trimesters.
- Overactive Bladder (Frequent Urination): Overactive bladder during the third trimester of pregnancy occurs due to hormonal and physical changes. Extra baby weight creates pressure on the bladder as the baby grows, leading to the frequent need to urinate. Overactive bladder is the fifth most common symptom during pregnancy, with approximately 10% of pregnant women experiencing frequent urination, according to a 2017 study titled “Symptom Experience in Late Pregnancy,” conducted by Kathleen R. Beebe et al. at the University of California and published in Journal of Obstetric, Gynecologic & Neonatal Nursing.
- Shortness of Breath (Dyspnea): Pregnant women experience reduced vital capacity (the amount of air a person can exhale) and expiratory reserve volume (the ability to exhale more air after a normal exhale). This means the lungs are not able to fully expand or contract as much as usual, resulting in a restricted breathing pattern during pregnancy. Impaired respiratory function is caused by hormonal changes and increased intra-abdominal volume during the third trimester, leading to shortness of breath. Shortness of breath becomes a more common complaint as pregnancy progresses, with reports of dyspnea in pregnant women increasing from 50% before the 20th week to 76% after the 31st week, including week 33, according to a 2013 study from Poland titled “Respiratory function in pregnant women,” by L. Hirnle et al., published in Neurobiology of Respiration.
- Forgetfulness (Pregnancy Brain): Pregnancy brain is a term used to describe maternal forgetfulness and other cognitive changes experienced during pregnancy, particularly in the third trimester. Symptoms of pregnancy brain include clumsiness, poor concentration, difficulty finding words, and general memory issues. Maternal cognitive decline is often attributed to changes in sleep patterns, stress, hormonal fluctuations, and physiological adjustments of pregnancy. Approximately 81% of pregnant women report experiencing some form of cognitive decline, which significantly affects daily life by causing confusion, disorientation, lack of motor coordination, and reading difficulties, according to a 2020 study from Indonesia titled “Variables Associated to the Decline of Cognitive Function in the Third Trimester of Pregnancy,” by Hamid Mukhlis et al., published in Journal of Critical Reviews.
- Edema (Swollen Ankles and Feet): Swollen ankles and feet due to edema are caused by excess fluid trapped in the tissue, frequently occurring in the third trimester. Symptoms of edema include heaviness, soreness, and a bursting sensation in the limbs. An enlarged uterus, higher body mass, increased blood volume, and hormonal changes during pregnancy cause edema. Lower limb edema is experienced by 80% of pregnant women, according to a 2017 study from Poland titled “Risk Factors Related to Lower Limb Edema, Compression, and Physical Activity During Pregnancy: A Retrospective Study” Zbigniew Szygula et al., published in Lymphatic Research and Biology.
- Body Aches and Pains: Body aches and pains during pregnancy include neck, back, lower back, hip, knee, ankle-foot pain, and hand-wrist numbness. Increased body aches and pains develop dramatically in the third trimester due to changes in hormones and posture, weight gain, and fluid retention. Low back pain (70.7%), back pain (43.5%), hand-wrist discomfort (33.2%), and hip pain (32.1%) were the most common body pain symptoms during pregnancy in a 2018 study from Turkey titled “Musculoskeletal pain and symptoms in pregnancy: a descriptive study” by Serdar Kesikburun et al., published in Therapeutic Advances in Musculoskeletal Diseases.
What Is The Importance Of Understanding Being 33 Weeks Pregnant?
The importance of understanding being 33 weeks pregnant is recognizing and managing the physical and emotional changes in the third trimester. The 33-week pregnant mother prioritizes staying active while managing symptoms like pelvic girdle pain, wrist pain from carpal tunnel syndrome, and body aches. These discomforts are normal but can be alleviated through gentle exercises, stretching, and maintaining a healthy posture.
Monitoring Braxton Hick’s contractions is crucial. Braxton-Hicks contractions are irregular, mild contractions that prepare the uterus for labor but are not true labor contractions. Contractions are a sign of preterm labor if they become regular and painful, which requires immediate medical attention. Regularly checking fetal movements ensures the baby’s well-being, as decreased activity sometimes signals complications.
Managing common symptoms like insomnia, shortness of breath, and frequent urination is essential. Insomnia tends to worsen in the third trimester, a common pattern seen when examining pregnancy week by week. OB-GYNs suggest sleeping on the left side to improve sleep. Shortness of breath is common due to the growing uterus pressing on the diaphragm.
Understanding the baby’s development at week 33 is important for emotional preparation. The baby is about the size of a pineapple and continues to grow, with key systems like the nervous system, immune system, and bones maturing rapidly. The mother’s diet should be rich in calcium, iron, and omega-3 fatty acids to support the baby’s development.
Attending prenatal appointments is crucial for monitoring the baby’s growth and health and the mother’s blood pressure to watch for preeclampsia. Staying informed about these changes ensures a healthier pregnancy and prepares both mother and baby for a safe delivery.
What To Expect At 33 Weeks Pregnant?
The 33-week pregnant mother must expect a range of physical and emotional changes as the baby grows. Pelvic girdle pain, a sharp or dull ache in the pelvic area, occurs due to loosening joints and increased pressure. Braxton Hicks contractions, third-trimester symptoms, are irregular mild contractions that help prepare the uterus for actual labor. Insomnia often happens, with hormonal changes and discomfort disrupting sleep.
Wrist pain, often from Carpal Tunnel Syndrome, causes tingling or weakness in the hands. Vaginal swelling due to increased blood flow and pressure in the pelvic veins is another common symptom. Frequent urination results from the growing baby pressing on the bladder. Shortness of breath develops as the expanding uterus restricts lung capacity.
Pregnancy brain (forgetfulness or difficulty concentrating) is commonly reported. Fluid retention results in edema (swelling in the feet and ankles). General body aches and pains, especially in the back, hips, and legs, increase as the body adapts to extra weight and shifting posture. The baby continues significant developmental strides, preparing for birth.
How Is The Baby Developing At 33 Weeks Pregnant?
Your baby grows to the size of a pineapple and weighs approximately 2103 grams (74.18 ounces or 4.64 pounds) at 33 weeks pregnant. Key developmental milestones focus on physical growth and maturation across multiple systems.
Your baby’s sensory abilities during week 33 are advancing. The pupils now detect and respond to light, while eye movements and blinking are becoming more coordinated. The nervous system, particularly the brain, quickly develops, allowing the baby to form early memories and recognize sounds.
Facial expressions are becoming more complex, with the baby showing responses such as grimacing or smiling. Movements are more refined as the baby reacts to touch and external sounds. Self-touch behaviors, like hand-to-face contact, become more frequent at week 33.
The baby’s bones harden as calcium and other minerals are transported from the mother to the baby. The immune system matures, with the transfer of maternal antibodies increasing to help protect the baby after birth.
How Big Is Your Baby At Week 33 Of Pregnancy?
Your 33-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 33-week-old fetus is about the size of a pineapple. The 50th percentile measurements for 33-week fetal growth are as follows: the biparietal diameter (BPD) is 83 millimeters, the head circumference (HC) is 303 millimeters, the abdominal circumference (AC) is 288 millimeters, the femur length (FL) is 63 millimeters, and the humerus length (HL) is 56 millimeters.
The 33-week-old fetus weighs 2103 grams (74.18 ounces or 4.64 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 33 of Pregnancy?
Key developmental milestones of babies at week 33 of pregnancy include sight, facial expressions, blinking, movement, and immune system development. Here are 7 key developmental milestones of babies in week 33.
- Sight: The fetal pupils have matured enough to detect changes in light levels and respond to light stimuli at week 33. The baby begins to show significant eye movements essential for visual development, such as constricting and dilating in response to light. This means your baby’s eyes have developed to see and react to bright lights shining through your belly.
- Facial Expressions: Fetal facial expressions become more complex in the third trimester, showing emotion-like reactions such as crying and laughing. Babies display a range of facial expressions, including “smiling” and “grimacing,” in response to different stimuli at 33 weeks of pregnancy, according to a 2011 study from Durham titled “Do Facial Expressions Develop before Birth,” by Nadja Reissland et al., published in Plos One. Facial expressions reflect the development and maturity of the fetal brain and central nervous system, crucial for fetal and maternal communication and bonding.
- Blinking: Your baby begins to blink slowly and spontaneously (about six blinks per minute) at 33 weeks. Fetal blinking might begin earlier in gestation, though ultrasound scans only detect the tiny blinking movements between 31-33 weeks as the eyelids grow more.
- Movement: Fetal movement increases, with your baby responding to maternal touch and vibroacoustic stimulation with exaggerated arm, head, and mouth movements and changes in heart rate. Babies often show significant self-touch behaviors like rubbing the eyelids and scratching the temples at 33 weeks, according to a 2005 study from Spain titled “Analysis of fetal breathing movements at 30–38 weeks of gestation,” by Jesús Florido et al., published in Journal of Perinatal Medicine. Facial movements like eyelid blinking, mouthing, and hand-to-face interactions become more frequent in the third trimester.
- Immune System: Maternal antibodies are vital to the fetus and newborn’s immunity against pathogens. Fetal IgG (Immunoglobulin G, an antibody) levels increase gradually during the first and second trimesters, with the most significant rise occurring in the third trimester, including the 33rd week. The increase leads to newborn IgG levels of approximately 125% of maternal serum levels, indicating active antibody transfer.
- Bones: Fetal calcium demand is highest during the third trimester as the baby’s bones are hardening. Essential minerals such as calcium (Ca), phosphorus (P), and magnesium (Mg) are transported from the mother’s body across the placenta to support bone development. The rate of calcium transfer from mother to fetus increases significantly in the last trimester, from around week 24 of pregnancy until delivery, with peak accumulation rates occurring at 36 to 38 weeks.
- Nervous System: Your baby’s sensory systems are becoming functional and integrated at 33 weeks. The developing cortex now has an adult-like structure, with connections from various central neurotransmitter systems and increasing connectivity between brain regions. Sleep phases, including rapid eye movement (REM) and non-REM sleep, develop by weeks 33 to 35 as the neural connections and brainstem mature. The brain is sufficiently developed to support fetal awareness and the formation of neural circuits based on experience, allowing the baby to learn and recognize sounds, music, language features, and odors and to store memories of prenatal experiences, according to a 2019 study from Italy titled “Correlation between human nervous system development and acquisition of fetal skills: An overview” by Elisa Borsani et al., from the University of Brescia, published in Brain and Development.

How To Know If Your Baby Is Healthy During Week 33 Of Pregnancy?
To know if your 33-week-old baby is healthy, track fetal size and weight, track fetal movement, check amniotic fluid levels, take prenatal screenings, and monitor bone development. Here are 5 ways to know if your baby is healthy during week 33 of pregnancy.
- Track Fetal Size and Weight: The 33-week-old baby is about the size of a pineapple. Have an ultrasound consultation during prenatal checkups with your OBGYN to monitor your baby’s size and estimated fetal weight.
- Track Fetal Movement: Monitoring fetal movement is one of the oldest methods to assess your baby’s health. Women at 33 weeks of pregnancy are encouraged to keep track of baby movements daily by counting and recording any dramatic changes. Regular fetal movements (10 movements within 2 hours) indicate a healthy baby, while decreased fetal movement is associated with stillbirth.
- Check Amniotic Fluid Level: Amniotic fluid is a clear, slightly yellowish liquid surrounding your fetus for protection and development. Low amniotic fluid suggests complications like umbilical cord compression, while too much indicates fetal abnormalities. An ultrasound monitors amniotic fluid levels, and other tests are performed if abnormal levels are detected.
- Take Prenatal Screenings: Cell-free DNA (cfDNA) testing is a blood test performed in any trimester, including week 33. The test checks the baby’s DNA through the mother’s bloodstream and detects conditions such as Down Syndrome and trisomy 18.
- Monitor Bone Development: Your baby’s bones continue to harden at 33 weeks pregnant, except for the skull. A three-dimensional ultrasound test is used to diagnose selected skeletal malformations.
What Is The Position Of Your Baby At 33 Weeks Pregnant?
The position of your baby at 33 weeks pregnant is likely cephalic (head-down), according to a 1985 study titled “Fetal position during pregnancy,” conducted by Michael John Hughey at Northwestern University School of Medicine and published in the American Journal of Obstetrics and Gynecology. The study demonstrated about 93% of fetuses were in a cephalic position between 33-36 weeks, while 6% were in a breech (feet-first) position, and 1% were in transverse or other positions. Babies in a cephalic position are head down, chin tucked into the chest, and bodies facing the mother’s back, typically causing a heavy feeling in your lower stomach and pelvis.
Most babies assume a cephalic position during the third trimester in preparation for birth. The fetal position at 33 weeks is not final as the baby often moves and adjusts positions, and the final birth position of your baby is usually identified at 36 weeks. Babies in a non-cephalic position have a 75% chance of turning into a cephalic position, while babies in a cephalic position have a 1% chance of changing positions before delivery.
Why Do Your Baby’s Kicks Feel Heavier At 33 Weeks Pregnant?
Your baby’s kicks feel heavier at 33 weeks pregnant because of the baby’s growing size and changing position, according to a 1985 study from Japan titled “Fetal Movement and Fetal Position” conducted by Shigeo Suzuki et al. at Kyoto University and published in Early Human Development.
Fetal movements start to become restricted by the abdominal walls at around 21 to 31 weeks as your baby grows. The restriction results in a smaller space for the baby to move, leading to stronger and more noticeable kicks. The fetus is unable to extend their limbs fully within the womb from 32 weeks onward, causing movements like kicking and rolling to be felt more intensely and clearly by the mother.
Your baby is likely in a cephalic (head-down) position at 33 weeks, with the head pressing against your lower belly and pelvis. Cephalic fetal positioning often leads to stronger kicks felt underneath the ribs. Babies in a cephalic position generally produce more intense kicks compared to those in a breech position, according to a 2018 study from the United Kingdom titled “European Society of Biomechanics S.M. Perren Award 2018: Altered biomechanical stimulation of the developing hip joint in the presence of hip dysplasia risk factors” by Stefaan W. Verbruggen et al. and published in Journal of Biomechanics.
Is Your Baby’s Immune System Developed At 33 Weeks Pregnant?
Yes, your baby’s immune system is developed at 33 weeks but only becomes fully functional after birth, according to a 2019 study titled “Maturation of the immune system in the fetus and the implications for congenital CMV,” conducted at Tel Aviv University and published in Best Practice & Research Clinical Obstetrics and Gynaecology. Your baby now has the essential components of a functional immune system, including classical lymphocytes like B-cells, T-cells, and NK (natural killer) cells.
The fetal immune system begins developing as early as 8 weeks of pregnancy with the formation of classical lymphocytes, which detect and fight pathogens in the body. T-cells and B-cells start functioning during the second trimester and are typically detectable in the blood by the second to mid-third trimester. The receptors on T-cells and B-cells further diversify in the last three months, signaling a period of rapid maturation for the fetal immune system in the third trimester.
NK cells destroy infected cells in the body without requiring prior activation. Fetal NK cells start developing in the liver at 6 weeks and migrate to the bone marrow by week 20. NK cells continue to diversify and mature rapidly, showing responses to pathogens, such as Cytomegalovirus (CMV), by the third trimester.
What Are The Changes In The Mother’s Body At 33 Weeks Pregnant?
Changes in the mother’s body at 33 weeks pregnant include pelvic girdle pain, Braxton Hicks contractions, insomnia, wrist pain, and vaginal swelling. Here are 10 changes in the mother’s body in week 33 of pregnancy.
- Pelvic Girdle Pain: Characterized by stabbing, dull, or burning sensations in the pelvic area due to joint relaxation or instability.
- Braxton Hicks Contractions: Painless mild, irregular uterine contractions help prepare the body for labor.
- Insomnia: Hormonal changes and physical discomfort cause difficulty falling or staying asleep, leading to fatigue and potential complications.
- Wrist Pain: Fluid retention and weight gain cause pressure on the wrists, resulting in Carpal Tunnel Syndrome or De Quervain Tenosynovitis.
- Vaginal Swelling: Increased blood flow and pressure in the pelvic veins lead to swelling and discomfort in the vulvar region.
- Frequent Urination: The growing baby puts increased pressure on the bladder, which results in a more frequent urge to urinate.
- Shortness of Breath: Hormonal changes and the enlarged uterus limit lung expansion, causing a feeling of restricted breathing.
- Forgetfulness (Pregnancy Brain): Hormonal and physical changes contribute to memory lapses, confusion, and difficulty concentrating.
- Edema (Swollen Ankles and Feet): Fluid retention and increased blood volume cause swelling in the lower limbs, leading to discomfort and heaviness.
- Body Aches and Pains: Increased weight, posture changes, and hormonal fluctuations contribute to pain in the back, hips, and other body areas.
How Big Is A 33 Weeks Pregnant Belly?
A 33-week pregnant belly has a fundal height of around 33 centimeters (cm). The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height generally correlates with the gestational age. Therefore, a 33-week-pregnant belly measures around 33 centimeters, between 31 to 35 centimeters. The expanding uterus grows to accommodate the growing fetus. The 33-week pregnant uterus has grown enough to be palpated above the navel level.
The uterine size and growth rate are affected by several factors, such as the mother’s body mass index (BMI), the number of pregnancies she has had, variations in the amount of amniotic fluid, or the different sizes of the fetus. For example, women with a higher BMI tend to have a slightly larger fundal height measurement than those with a lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. Still, the 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence for using the SFH to predict fetal health.
Do Contractions Occur More At 33 Weeks Pregnant?
Yes, contractions do occur more at 33 weeks pregnant. Regular uterine contractions occurring before 37 weeks and causing cervical dilations of 2 cm or more indicate preterm labor, according to “Preterm Labor and Birth: A Clinical Review,” by Kellie M Griggs et al. published in American Journal of Maternal/Child Nursing. Preterm labor is characterized by period-type cramps, feeling the baby “balling up,” and frequent painless contractions. Signs of preterm labor include increased amounts of mucus-like, watery, or bloody discharge and fluid leakage from the vagina, typically accompanied by pain in the lower back and pressure in the pelvis or lower abdomen.
Contractions at 33 weeks sometimes indicate Braxton-Hicks contractions or “false labor pains,” which do not signify actual labor or cause cervical changes. Braxton-Hicks contractions are common during the second to third trimester and are often mistaken for true labor. Symptoms include weak, irregular, painless, and uncomfortable cramps lasting between 30 seconds and 2 minutes. Contact your OBGYN (obstetrician-gynecologist or OB-GYN) for unusual contractions occurring more than 5 times per hour and increasing in duration and intensity.
What Are The Tips For Prenatal Care During Week 33?
Prenatal care tips for women at 33 weeks pregnant include attending prenatal appointments, getting prenatal tests, eating a healthy diet, hydrating often, and engaging in physical activity. Here are 6 prenatal care tips for women at week 33 of pregnancy.
- Attend Prenatal Appointments: Regular check-ups with an OBGYN assess fetal development and detect any signs of complications such as hypertension and preeclampsia. Prenatal appointments involve ultrasound, blood tests, and urinalysis to identify potential issues and adjust treatment plans as needed.
- Get Prenatal Tests: Prenatal tests at week 33 are essential for monitoring your baby’s health. Genetic screenings such as cell-free DNA (cfDNA) identify potential genetic conditions, helping parents prepare and plan. A biophysical profile through an ultrasound evaluates the baby’s heart rate, breathing, fetal movements, amniotic fluid volume, and muscle tone. Talk to your OBGYN about which prenatal tests are recommended during the third trimester.
- Continue Eating a Healthy Diet: Focus on consuming various nutrient-rich foods, including fruits and vegetables. Calcium-rich foods like dark green leafy vegetables prevent calcium depletion and support fetal bone development. Avoid foods with high caffeine, such as coffee, chocolate, and fizzy drinks. Watch out for foods that worsen heartburn symptoms, and refrain from restrictive diets to avoid nutrient deficiencies.
- Hydrate Often: Hydrate often to meet increased water needs. Fluid intake helps maintain balance, supports various bodily functions, prevents complications like urinary tract infections, and promotes healthy fetal growth. Pregnant women must drink 2.7-4.8 liters of water daily, as the American Medical Research Institute and World Health Organization (WHO) recommend.
- Do Physical Activity: Staying fit during pregnancy enhances maternal physical and psychological well-being. More energy spent on exercise is associated with better health outcomes for the mother and the baby. Create an exercise routine, including low-impact aerobics such as walking and swimming.
- Get a Comfortable Sleeping Position: Sleep problems are common during the last few months of pregnancy. Leg cramps, urinary incontinence, shortness of breath, and back pain lead to poor sleep, according to a 2016 study, “The relationship between sleep disturbance in late pregnancy and labor outcomes.” Use pillows to create a comfortable position and increase sleep quality. Sleeping on your side is particularly helpful as your uterus grows at week 33.

What Types Of Foods Are Beneficial To Eat During Week 33 Of Pregnancy?
Types of foods beneficial to eat during week 33 include foods rich in calcium, iron, iodine, choline, vitamins A, B6, B12, C, D, and folate to ensure your health and baby’s growth. Here are 15 beneficial foods to eat during week 33 of pregnancy.
- Calcium-rich Foods: Help build strong bones and teeth. Try yogurt, dark green leafy vegetables, and cheese.
- Iron-rich Foods: To increase blood volume and oxygen supply to your baby, try lean red meat, iron-fortified cereals, and prune juice.
- Iodine-rich Foods: Essential for brain development. Iodine-rich foods include eggs, seafood, and dairy products.
- Choline-rich Foods: Important for brain and spinal cord development. Eat peanuts, eggs, and soy products.
- Vitamin A-rich Foods: Support your baby’s eyes and skin development. Choose from sweet potatoes, carrots, and green leafy vegetables.
- Vitamin C-rich Foods: Help with collagen formation and iron absorption. Citrus fruits, strawberries, and tomatoes are good sources of Vitamin C.
- Vitamin D-rich Foods: Promote bone health. Try fortified milk, sardines, and salmon.
- Vitamin B6-rich Foods: Help form red blood cells. Try bananas, pork, and whole-grain cereals.
- Vitamin B12-rich Foods: Support the nervous system and red blood cell production. The best sources of Vitamin B12 are poultry, fish, and milk.
- Folic Acid-rich Foods: Prevent birth defects and support placenta health. Try enriched bread, beans, and dark green leafy vegetables.
- Grains: Provide energy and fiber. Choose from quinoa, oats, and brown rice.
- Fruits: Rich in vitamins and antioxidants. Try fresh fruit, dried fruit, and canned fruit.
- Vegetables: Provide essential vitamins and minerals. Choose from raw vegetables, frozen vegetables, and 100% vegetable juice.
- Protein: Supports baby’s growth and development. Poultry, beans, and eggs are good sources of protein.
- Dairy: Provides calcium and protein. Try pasteurized milk, cheese, and yogurt.
Why Is Omega-3 Fatty Acid Important?
Omega-3 Fatty Acids are essential during week 33 and pregnancy because they support your baby’s brain and eye development and are associated with reduced risks for preterm births and higher birth weights, according to a 2010 study titled “Omega-3 Fatty Acid Supplementation During Pregnancy,” conducted by Jaclyn M. Coletta, MD et al. and published in Reviews in Obstetrics & Gynecology. Pregnant women in the study who incorporated omega-3 fatty acids in their diets delivered babies with higher birth weights than mothers who did not.
Omega-3 fatty acids are healthy fats containing long-chain omega-3 polyunsaturated fatty acids (PUFA), essential for supporting the rapid development of your baby’s brain and retina during the third trimester. Omega-3 fatty acids have anti-inflammatory properties and help regulate inflammatory substances that stimulate labor, decreasing risks for preterm birth.
Common sources of omega-3 fatty acids include various kinds of seafood like salmon, pollock, shrimp, and scallops. Pregnant women are advised to avoid high-mercury fishes like swordfish and king mackerel, which are often associated with increased risks for birth defects. About two 6-ounce portions of low-mercury fish and seafood per week are recommended during pregnancy. Some women prefer to take daily fish oil capsules without harmful amounts of mercury and PCB (polychlorinated biphenyls).
What Exercises Can You Do During Week 33 Of Pregnancy?
Exercises you can do during week 33 of pregnancy include walking, swimming, stationary bicycling, stretching, and kegel exercise, as the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour recommends. Here are 5 exercises you can do during week 33 of pregnancy.
- Walking: Walking improves circulation without overstressing the joints. Walking is an easy and effective way to stay active and is ideal for a low-impact workout routine.
- Swimming: Swimming alleviates joint pressure, supports a growing belly, and enhances cardiovascular health. The buoyancy of water supports the weight of your bump and other joints during swimming, helping you stay fit without getting too exhausted.
- Stationary Cycling: Riding a stationary bike helps maintain endurance without the risk of falls. Stationary cycling is ideal for staying active while reducing strain on pelvic floor muscles.
- Stretching: Gentle stretches improve flexibility, reduce muscle tension, and relieve common pregnancy discomforts like lower back pain. Incorporating stretches focused on the pelvic floor promotes muscle tone and strength as labor approaches.
- Pelvic Floor Exercises (Kegels): Strengthening pelvic floor muscles is essential in week 33 to support your weight and reduce the risk of urinary incontinence during and after delivery.
Aim for 150 minutes of moderate-intensity aerobic and muscle-strengthening activities weekly. Always start with small exercises and gradually increase the duration. Listen to your body and avoid exercises that involve risks of falling or injuries.
What Are The Things To Avoid At 33 Weeks Pregnant?
Things to avoid at 33 weeks pregnant include alcohol, smoking, certain medications and supplements, recreational drugs, and caffeine. Here are 17 things that you should avoid at 33 weeks pregnant.
- Alcohol: Steer clear of alcohol at any stage of pregnancy, including week 33, to avoid serious developmental problems such as fetal alcohol spectrum disorders (FASD). Even small amounts of alcohol harm the baby, as detailed in a 2020 study, “Alcohol Use in Pregnancy,” by researchers at Oregon Health and Science University.
- Smoking and Secondhand Smoke: Smoking and secondhand smoking increase the risk of complications like preterm birth and low birth weight. Seek help to quit if necessary.
- Recreational Drugs: Recreational drugs pose severe risks to your baby, including developmental delays and low birth weight.
- Cannabis (Marijuana): Cannabis use during pregnancy is linked to complications like low birth weight and developmental issues.
- Excessive Caffeine: Limit caffeine intake to below 200 mg daily to avoid an increased risk of miscarriage or low birth weight. Consider using a caffeine calculator to track your intake from sources like coffee and chocolate.
- Certain Medications: Always check with your doctor before taking any new medications, supplements, or herbal remedies, as some are harmful to you and your baby.
- High Mercury Fish: Limit eating fish with high mercury levels, such as swordfish, shark, and king mackerel, to protect your baby’s developing nervous system.
- Undercooked or Raw Meat: Avoid raw or undercooked meat to prevent foodborne illnesses like toxoplasmosis.
- Unwashed Vegetables and Fruits: Wash all produce thoroughly to avoid potential exposure to harmful bacteria and parasites.
- Deli Meats: Reheat deli meats before consumption to avoid the risk of listeriosis, a dangerous infection for pregnant women.
- Unpasteurized Foods: Avoid unpasteurized dairy products, soft cheeses, and undercooked eggs to minimize the risk of bacterial infections.
- Hot Tubs and Saunas: Avoid hot tubs, saunas, and other heat sources, as overheating harms your developing baby.
- Strenuous Activities: Avoid contact sports or activities with a high risk of falling or abdominal injury.
- Heavy Lifting: Avoid lifting heavy objects to prevent straining your body and possibly causing preterm labor.
- Stress: Manage stress by finding relaxing activities, as high stress levels negatively impact you and your baby. Regular exercise and a healthy diet help reduce stress and improve overall well-being.
- Gardening and Cat Litter: Always wear gloves to avoid contact with contaminated soil. Have someone else handle changing cat litter to reduce the risk of toxoplasmosis.
- Chemicals and Toxins: Be cautious when using cleaning products or handling chemicals, as some are harmful during pregnancy. Consider using natural or pregnancy-safe alternatives.
Follow precautions and avoid harmful influences in week 33 to ensure your health and your baby’s safety. Always consult your healthcare provider for any concerns.
Should You Go To Prenatal Classes At 33 Weeks Pregnant?
Yes, you should go to prenatal classes when you are 33 weeks pregnant. Prenatal classes teach essential information and skills regarding pregnancy, labor, and early postpartum experiences, according to a 2017 study titled “Perceived Benefits of Childbirth Education on Future Health-Care Decision Making,” conducted by Jane Leach, PhD, RNC, IBCLC, et al. and published in The Journal of Perinatal Education
Prenatal classes help parents prepare for childbirth by providing information on what to expect, including possible complications, medical interventions, and pain management options. Attending prenatal classes often improves mothers’ mood and attitude, boosting vitality, confidence, and emotional well-being. Preparation in prenatal classes helps mothers cope more effectively with the physiological and psychological changes of pregnancy, enhancing the overall birthing experience.
What Can You Do To Prepare For Labor At 33 Weeks Pregnant?
You can prepare for labor at 33 weeks by attending prenatal classes, practicing pelvic floor exercises, keeping yourself healthy and relaxed, contacting a doula, and preparing your hospital essentials. Keeping in touch with your OBGYN (obstetrician-gynecologist) to assess and prevent preterm birth risks becomes increasingly important as you approach delivery.
Prenatal classes provide parents with valuable information about how to prepare for and what to expect during labor and delivery. Pelvic floor exercises (Kegel exercises) help strengthen the pelvic muscles to support the uterus during labor. Being relaxed and healthy helps the mother manage childbirth’s physical and mental stress. Contacting a doula is helpful for additional guidance during labor. Prepare a hospital bag with essentials such as clothes, toiletries, nursing pads, and important hospital documents like your ID and birth plan.
Why Is Sleeping On Your Left Side The Ideal Sleeping Position?
Sleeping on your left side is the ideal sleeping position during pregnancy because it promotes blood flow and oxygen delivery to the fetus, reducing the risk of stillbirth, according to a 2017 study, “Going to sleep in the supine position is a modifiable risk factor for late pregnancy stillbirth; Findings from the New Zealand multicentre stillbirth case-control study,” by Lesley M. E. McCowan et al., published in PLoS ONE.
Studies using magnetic resonance imaging (MRI) and Doppler ultrasound have shown the diameter of the vena cava (returning blood to the heart) is reduced when lying supine (on the back) compared to lying on the left side in late pregnancy and blood flow in the uterine artery (supplying blood to the uterus and baby) is lowered when lying on the back compared to the left side. A left-side sleeping position relieves pressure from the internal organs compared to a supine or right-sided sleep position, reducing reflux symptoms of GERD (gastroesophageal reflux disease). The findings suggest sleeping on the left side to improve blood circulation to the uterus, placenta, and baby during pregnancy. Pregnant women who sleep supine are associated with a 3.7-fold increased risk of stillbirth.
What Are The Possible Complications That Can Happen At 33 Weeks Pregnant?
Possible complications that can happen at 33 weeks pregnant include vaginal bleeding, placental abruption, preterm birth, swelling, and hypertension or preeclampsia. Here are 6 possible complications that occur during week 33.
- Vaginal Bleeding: Vaginal bleeding is experienced in about 25% of pregnancies and is associated with higher risks of preterm delivery. Multiple episodes of heavy or prolonged bleeding increase the risk of low birth weight and perinatal death, making prompt medical care essential if bleeding occurs.
- Placental Abruption: Placental abruption occurs when the placenta separates from the uterus before the baby is born, reducing oxygen supply to the baby and often leading to heavy bleeding in the mother. Placental abruption causing fetal distress requires an emergency cesarean delivery to protect the baby. Factors like high blood pressure, substance abuse, and abdominal trauma increase the risk of placental abruption.
- Preterm Birth: Preterm birth is when a baby is delivered before 37 weeks of pregnancy. Preterm birth is commonly due to an infection triggering inflammation, membrane rupture, and cervical changes, leading to early delivery. Signs of preterm birth include regular abdominal tightening, menstrual-like cramps, pelvic pain, and a plug of mucus or fluid leaking from the vagina. Preterm birth during week 33 is associated with fetal illnesses.
- Swelling (Edema): Swelling during pregnancy often occurs in the feet, ankles, and legs. Increased blood volume, pressure on the inferior vena cava, and body weight result in salt and water retention, leading to swelling. Lower limb edema occurs as early as the first trimester but is more common in the second and third trimesters, affecting an estimated 50-80% of pregnancies.
- Hypertension and Preeclampsia: Gestational hypertension is diagnosed when a mother receives a blood pressure reading greater than 140/90. Preeclampsia is characterized by high blood pressure, protein in the urine, and organ dysfunction. Signs of preeclampsia include severe headaches, vision changes, upper abdominal pain, and swelling in the face and hands. Pregnant women with obesity and a history of high blood pressure are at a higher risk for developing hypertension and preeclampsia during pregnancy.
- Carpal Tunnel: Carpal tunnel syndrome (CTS) occurs when the median nerve running through the wrist is compressed, causing numbness, tingling, and pain in the hand and fingers. Studies indicate around 31-62% of pregnant women have self-reported CTS symptoms. Risk factors of CTS include pre-pregnancy obesity, excessive gestational weight gain, a higher number of previous live births, gestational hypertension, and diabetes.
How Common Are Preterm Labors At 33 Weeks Pregnant?
Preterm labors at 33 weeks pregnant are relatively common, with over 84% of preterm births occurring between 32–36 weeks, according to a 2020 study titled “Global burden of preterm birth,” conducted by Salimah R. Walani at the Global Programs Department and published in the International Journal of Gynecology and Obstetrics. Preterm labor at week 33 is considered moderately preterm.
Preterm labor is typically caused by an infection of the lower genital tract to the uterus, causing regular uterine contractions and leading to cervical dilations of 2cm or more before the 37th week of pregnancy. Spontaneous preterm labor is caused by natural contractions, cervical dilation, placenta previa (low placement of the fetus in the uterus), and premature rupture of the amniotic fluid (PPROM), which makes up approximately 75% of preterm births.
Common symptoms of preterm labor include leaking fluid from the vagina and increased discharge, often accompanied by menstrual-like cramps and pain in the lower back and pelvis. Pregnant women experiencing preterm labor at 33 weeks are typically admitted to a healthcare facility for monitoring, including checking for cervical dilation, potential complications, and the baby’s health. Contact your doctor immediately for medical assistance if you notice any symptoms of preterm labor.
How Can A Partner Support The Mother At 33 Weeks Pregnant?
A partner can support the mother at 33 weeks pregnant through physical task assistance, emotional support, lifestyle changes, responsibility sharing, and self-care encouragement. Here are 5 ways a partner can support the mother at 33 weeks.
- Physical Task Assistance: Demonstrate physical support by doing housework, helping with cooking, running errands, or going to the grocery store. Assist with tasks requiring bending, reaching, or heavy lifting to ease the burden on the mother’s body.
- Emotional Support: Offering praise and reassurance at 33 weeks pregnant helps the mother feel loved and supported. Provide affirmations by expressing appreciation for the mother’s strengths and beauty.
- Lifestyle Changes: Encourage healthy changes to ensure the mother and baby’s well-being at 33 weeks pregnant. Help maintain a balanced diet rich in nutrients, avoid harmful substances, and prioritize adequate rest. Encourage regular prenatal check-ups and offer assistance with household chores or errands. Do physical activities together, such as brisk walking, to provide support and motivation.
- Responsibility Sharing: Shared involvement strengthens the emotional bond and ensures the mother does not face the journey alone. Attend OBGYN appointments together to show commitment and support. Join childbirth classes and get involved in decisions to build a strong parenting foundation.
- Self-Care Encouragement: Encourage the mother to take time for self-care and show support in activities that promote well-being, such as getting enough rest, eating well, and engaging in enjoyable activities.
What Prenatal Tests Are Needed At 33 Weeks Pregnant?
Prenatal tests needed at 33 weeks include blood tests and vaccination checks, amniocentesis, genetics screening, preeclampsia screening & hypertension monitoring, a biophysical profile (BPP or BPS), and a nonstress test (NST).
Blood tests and vaccination checks performed at 33 weeks of pregnancy help monitor the health of the mother and the baby. Blood tests include checking for possible anemia through a complete blood count (CBC) or iron level screening and screening for infections like HIV, syphilis, chlamydia, and gonorrhea using serum tests at 28-36 weeks gestation. Vaccine shots for Influenza (Flu) and tetanus, diphtheria, and pertussis (TDaP) are recommended during the third trimester of pregnancy to help provide immunity and reduce the risk of infection for the baby at 33 weeks.
Amniocentesis is a procedure in which a small amount of amniotic fluid is extracted from the uterus to test for fetal conditions. Amniocentesis is typically performed in the second trimester but sometimes occurs in the third trimester if the mother has not been offered amniocentesis earlier in the pregnancy or due to a late diagnosis of fetal malformations or intrauterine growth restriction (IUGR).
Non-invasive prenatal testing (NIPT) using cell-free fetal DNA (cffDNA) is a method for detecting chromosomal abnormalities in the fetus, particularly useful for genetics screening for disorders like Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and Patau syndrome (trisomy 13). Cell-free fetal DNA testing is valuable in the later stages of pregnancy, like week 33 when traditional diagnostic methods are more invasive and carry higher risks. The cffDNA test uses a blood sample from the pregnant mother to analyze fetal DNA circulating in the bloodstream. The test is highly accurate but tends to perform better when performed in the second and third trimesters of pregnancy, according to a 2016 study from the UK titled “Accuracy of non-invasive prenatal testing using cell-free DNA for detection of Down, Edwards and Patau syndromes: a systematic review and meta-analysis,” by Siobhan Quenby et al., published in BMJ Open.
Preeclampsia screening is crucial in the third trimester due to the potential complications for the mother and baby. Maternal evaluation includes checking vital signs and a physical examination to identify symptoms of preeclampsia, such as elevated blood pressure and swelling. Laboratory tests include a complete blood cell count, platelet count, and assessments of kidney function and liver health to determine whether organs are affected. Urine tests measure the total protein/creatinine ratio in the mother’s urine to confirm proteinuria, a key indicator of preeclampsia. Frequent assessments are performed in cases of suspected or confirmed preeclampsia to monitor the condition, including monitoring blood pressure and daily blood tests to monitor platelet count and liver and kidney function.
A biophysical profile (BPP) is a detailed assessment tool used in the third trimester of pregnancy, combining ultrasound assessments and fetal heart rate monitoring (cardiotocography or CTG) to monitor the baby’s well-being and predict potential complications. The BPP measures five key factors, including fetal movements, fetal muscle tone, fetal breathing movements, amniotic fluid volume, and fetal heart rate reactivity. Monitoring multiple activities allows a more reliable prediction of the baby’s health status since reduced fetal movement is a potential warning sign of fetal distress. A modified BPP (MBPP) is performed immediately when a full BPP is unnecessary, focusing only on fetal heart rate reactivity and amniotic fluid volume. A complete BPP is conducted if abnormalities are detected in the MBPP for a more comprehensive assessment.
The nonstress test (NST) and contraction stress test (CST) monitor the fetal heart rate (FHR) and responses to different conditions, ensuring your baby is developing normally. NSTs are commonly performed during the third trimester to detect potential issues with the baby’s cardiovascular or nervous systems and to assess fetal oxygenation. The NST is a non-invasive test using cardiotocography to monitor FHR through external abdominal transducers to determine how the baby’s heart rate responds to fetal movements. A reactive NST is demonstrated by FHR accelerations, indicating a healthy fetal autonomic nervous system. A nonreactive NST, where sufficient accelerations are absent, requires further evaluation.
A CST evaluates how the baby’s heart rate responds to uterine contractions and is typically conducted if NST results are nonreactive. A CST checks whether the fetus experiences late decelerations (slowed FHR after a contraction), indicating compromised oxygenation. Late decelerations are a warning sign of fetal distress due to placental insufficiency. The CST helps to determine whether the baby is able to handle the stress of labor.
When To Call Your Doctor If Something Feels Wrong At Week 33 Of Pregnancy?
Call your doctor if something feels wrong at 33 weeks pregnant or if you experience symptoms such as regular contractions, heavy bleeding, decreased fetal movement, sudden swelling, and shortness of breath. The 5 symptoms that must be reported to your doctor are listed below.
- Decreased Fetal Movement: Fetal movements are maximal between 28-34 weeks of pregnancy. Call your OBGYN if you feel a dramatic change in your baby’s movement, especially if you feel less than 10 movements within two hours.
- Regular Contractions: Regular contractions or abdominal tightening is a sign of preterm labor. Contact your doctor immediately if you experience contractions with period-type pains or a “show” (a mucus plug coming out of the cervix). Preterm labor during week 33 is harmful to your baby.
- Heavy Bleeding: Vaginal bleeding is linked to many complications, including placental abruption and placenta previa. Placental abruption occurs when the placenta separates from the uterine wall before the baby is born, occurring at any time, but most commonly during the third trimester. Placenta previa is the abnormal implantation of the placenta in the cervical opening, accounting for about 20% of bleeding during late pregnancy. Call your OBGYN immediately to determine the cause of your bleeding.
- Sudden Swelling (Edema): Edema is a symptom of pre-eclampsia, a hypertensive disorder developing after 20 weeks of gestation. Call your OBGYN immediately if you notice puffiness and swelling in your hands, feet, or face, especially if accompanied by symptoms like headaches and vision changes.
- Shortness of Breath: Shortness of breath (SOB) is common during pregnancy, occurring in 60% to 70% of healthy pregnant women, but severe SOB must be checked to rule out underlying heart or lung disorders. Contact your healthcare provider if you notice significant changes in your breathing.
What are the 33 weeks pregnant symptoms not to ignore? 33 weeks pregnant symptoms not to ignore include decreased fetal movement, regular contractions, bleeding, swelling, and shortness of breath. Contact your OBGYN immediately if something feels wrong, you experience any symptoms, or you have concerns.
Are There Prenatal Vitamins Needed To Be Taken During Week 33 Of Pregnancy?
Yes, 10 essential prenatal vitamins and minerals, including calcium, iron, iodine, choline, vitamins A, C, D, B6, B12, and folic acid, need to be taken during week 33 of pregnancy to support the mother’s health and the baby’s development. The American College of Obstetricians and Gynecologists (ACOG) recommends maintaining a steady intake of key vitamins and minerals throughout pregnancy.
Calcium, at 1,000 milligrams for ages 19 to 50, is essential for bone development. The baby’s skeleton hardens during the third trimester, making adequate calcium intake vital to prevent maternal bone loss.
Iron, at 27 milligrams, supports the production of red blood cells to meet the growing baby’s needs. Iron prevents anemia and supports the increased blood volume that peaks in the later stages of pregnancy, including week 33.
Iodine, at 220 micrograms, remains necessary for proper brain development and thyroid function in the fetus.
Choline, at 450 milligrams daily, supports brain and spinal cord development. Adequate choline intake prevents neural tube defects and promotes healthy fetal brain growth.
Vitamin A, at 770 micrograms, contributes to the baby’s lung development and supports the mother’s skin, eyesight, and immune system.
Vitamin C, recommended at 85 milligrams, aids in forming healthy skin, tissues, and bones. Vitamin C enhances iron absorption, helping prevent anemia.
Vitamin D, at 600 international units, supports calcium absorption and strengthens the immune system.
Vitamin B6, at 1.9 milligrams, produces neurotransmitters and red blood cells needed for the baby’s brain development. Late-pregnancy symptoms like fatigue are alleviated by taking Vitamin B6.
Vitamin B12, at 2.6 micrograms daily, supports nerve function and red blood cell formation, ensuring healthy fetal nervous system development.
Folic acid, at 400 micrograms, promotes cell growth and placenta development. Folic acid prevents neural tube defects and supports fetal growth as pregnancy progresses.
Always follow your healthcare provider’s recommended dosages. Excessive doses of certain vitamins, such as Vitamin A, harm the baby.
What Does Parenting Styles Suggest About 33 Weeks Pregnant?
Parenting Styles suggests attending a breastfeeding workshop at 33 weeks pregnant.
“Attending a free breastfeeding workshop in our local library was invaluable when I was pregnant. It gave me the confidence and knowledge I needed to feel like I could do this,” says Pamela Li, the Founder and Editor-in-Chief of Parenting Styles.
Congratulations on being 33 weeks pregnant!
What Readers Are Saying
It’s our first baby this article is very very helpful and very informative for us thank you very much