36 Weeks Pregnant Symptoms: Week 36 Of Pregnancy And Prenatal Care
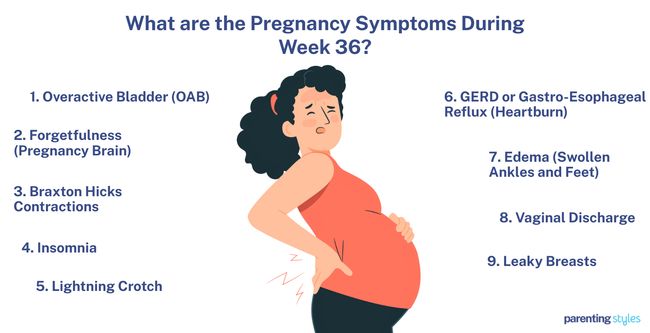
36 weeks pregnant symptoms include an overactive bladder, forgetfulness, Braxton-Hicks contractions, insomnia, and lightning crotch. Frequent urination occurs due to uterine pressure on the bladder, leading to an overactive bladder (OAB). Hormonal changes and glucose redirection to the baby cause forgetfulness, often called “pregnancy brain.” Irregular and painless Braxton-Hicks contractions increase in frequency without indicating labor. Physical discomfort and hormonal changes worsen insomnia. Lightning crotch, sharp pelvic pain, results from increased pressure on pelvic nerves when the 36-week baby moves lower into the pelvis.
Heartburn (GERD) persists due to the baby’s growth increasing pressure on the stomach, leading to acid reflux. Swelling in the feet and legs (edema) results from increased blood volume and uterine pressure. Increased vaginal discharge, including the loss of the mucus plug, signals preparation for labor. Colostrum leaks from the breasts in preparation for breastfeeding, although full milk production remains suppressed by high progesterone levels.
Recognizing symptoms helps 36 weeks pregnant mothers manage discomfort and prepare for labor. Regular prenatal checkups are essential for monitoring the health of mother and baby at 36 weeks.
Beneficial foods at week 36 pregnancy contain essential nutrients such as calcium, iron, iodine, choline, vitamins A, B6, B12, C, D, and folate, which support maternal health and the baby’s development. Calcium, critical for strong bones and teeth, comes from dairy products like milk, yogurt, cheese, and dark leafy greens. Iron-rich foods like lean meats, fish, beans, and fortified cereals are necessary for red blood cell production. Iodine, vital for thyroid and brain development, comes from seafood, dairy, and eggs.
Choline, found in eggs, tofu, and beef liver, aids brain and spinal cord development. Vitamin A, which supports vision and immune function, comes from sweet potatoes, carrots, and leafy greens. Vitamin C strengthens the immune system and improves iron absorption, with citrus fruits, broccoli, and strawberries being good sources. Vitamin D in fortified milk and fatty fish like salmon supports calcium regulation and bone health. Vitamin B6 aids brain development and metabolism, with bananas, chicken, and whole grains as common sources. Vitamin B12, necessary for red blood cell formation and nervous system health, comes from fish, meat, and dairy. Folate, which helps prevent neural tube defects, is present in enriched grains, beans, and spinach.
Eating a balanced diet is crucial for supporting the growth of the 36-week fetus and preparing the body for labor and postpartum recovery.
What is 36 weeks pregnant in months? 36 weeks pregnant is 9 months in pregnancy within the third trimester. You’ve finished the ninth month of pregnancy.
What Are The Pregnancy Symptoms During Week 36?
36 weeks pregnant symptoms include overactive bladder, forgetfulness, Braxton-Hicks contractions, insomnia, and lightning crotch. Below are common 36 weeks pregnancy symptoms.
- Overactive Bladder (OAB): Overactive bladder, characterized by frequent urination and a strong, urgent need to empty the bladder, is a common symptom throughout pregnancy, persisting at 36 weeks gestation. Leaking urine often occurs during physical activity, coughing, or sneezing due to stress incontinence, becoming more common as pregnancy progresses. 96.5% of women reported one or more urogenital symptoms in the 36th week in a 2006 study from The Netherlands titled “How Do the Prevalences of Urogenital Symptoms Change During Pregnancy?” by H. Jorien van Brummen et al., published in Neurourology and Urodynamics: Official Journal of the International Continence Society.
- Forgetfulness (Pregnancy Brain): Forgetfulness during pregnancy is commonly called “pregnancy brain” or “mommy brain” and is a normal experience at week 36. Cognitive changes occur as the mother’s body prioritizes supporting the growing fetus. Glucose, essential for brain function, is redirected towards fetal development, leaving fewer resources for memory and attention. Elevated cortisol levels during pregnancy contribute further to maternal forgetfulness. Tasks like remembering information and concentrating feel more challenging as a result.
- Braxton Hicks Contractions: Braxton Hicks contractions are irregular, painless contractions preparing the body for labor without shortening the cervix. The uterus contracts, causing your bump to feel tighter. Braxton-Hicks contractions become more frequent with a shorter cervix but remain irregular and non-progressive. Contractions reaching a frequency of 4 or more per hour raises the risk of preterm birth, though Braxton Hicks contractions usually remain intermittent and do not lead to labor.
- Insomnia: Insomnia becomes a prevalent symptom due to physical and hormonal changes at 36 weeks of pregnancy. Frequent awakenings and less time spent in deeper stages of sleep disrupt restful slumber, leading to sleeping problems. Trouble sleeping leads to increased fatigue as the body struggles to rest properly. Physical discomforts, such as pain and bladder pressure, intensify in the later stages of pregnancy, further complicating the ability to sleep soundly.
- Lightning Crotch: Pelvic discomfort and pelvic pain become more common as the baby drops lower into the pelvis during the third trimester, increasing pelvic pressure. Pregnancy symptoms of Symphysis Pubis Dysfunction (SPD) occur, with sharp, stabbing pain sometimes radiating through the abdomen, back, legs, and perineum. Movements such as turning in bed, standing on one leg, or bending down often intensify the pain, commonly described as burning or shooting.
- GERD or Gastro-Esophageal Reflux (Heartburn): Symptoms of gastroesophageal reflux disease (GERD) include heartburn and regurgitation, which occurs when undigested food rises back up the esophagus. Regurgitation is more common than heartburn and is often accompanied by nausea and vomiting. GERD symptoms usually persist into the third trimester, especially if experienced earlier in pregnancy. Women who experience GERD symptoms early in pregnancy are more likely to continue to experience symptoms until delivery, according to a 2011 study from Spain titled “Atypical Symptoms of Gastro-esophageal Reflux During Pregnancy,” by Fernando Rodríguez-Artalejo, et al., published in Revista Española de Enfermedades Digestivas.
- Edema (Swollen Ankles and Feet): Edema is commonly characterized by swelling in the lower limbs, particularly in the feet and legs. The swelling often causes discomfort, with symptoms such as heaviness, pain, and bursting sensation in the affected areas. Edema is caused by the growing uterus increasing venous pressure, leading to venous stasis (where blood struggles to flow from the legs back to the heart) and causing water retention. Increased blood volume, body weight, and hormonal changes further contribute to the development of edema.
- Vaginal Discharge: Clear or milky vaginal discharge increases as labor approaches. A thicker, jelly-like discharge in week 36 indicates a dislodged mucus plug in the cervix, signaling the body is already preparing for labor.
- Leaky Breasts: The breasts prepare for breastfeeding during the third trimester by expanding the ductal system and producing colostrum—a thick, yellow fluid rich in antibodies that serves as the baby’s first milk. Colostrum starts forming around the 20th week and increases as pregnancy progresses. Colostrum leaks from the nipples by week 36 due to increased prolactin, though full milk production remains blocked by high progesterone.
What Is The Importance Of Understanding Being 36 Weeks Pregnant?
The importance of understanding being 36 weeks pregnant involves understanding labor is likely to begin soon and preparing physically and mentally for delivery. Pregnancy week by week, regular prenatal checkups play a critical role in monitoring maternal and fetal health. Your OBGYN (obstetrician-gynecologist or OB-GYN) or midwife will track the baby’s position, typically head-down (cephalic), and check for complications such as preeclampsia or preterm labor.
Pressure from the uterus on the bladder causes an overactive bladder, leading to frequent urination. Burning or pain during urination likely indicates a urinary tract infection (UTI). Hormonal changes often result in forgetfulness, referred to as “pregnancy brain,” making lists and reminders useful for daily tasks.
Irregular and painless contractions, called Braxton-Hicks contractions, become more frequent. 36 weeks pregnant mothers must differentiate false labor pains from true contractions, which are more regular and increase in intensity, possibly accompanied by a mucous-like bloody discharge.
Discomfort and sleep disturbances, including insomnia, often worsen as the baby’s weight increases and pelvic and abdominal pressure rises. Resting when possible, adjusting sleep positions, and using pillows for support help manage sleep difficulties.
A 36-week baby reaches developmental milestones such as brain growth and bone hardening. Ultrasound confirms fetal positioning and checks for healthy growth. The 36-week fetus weighs 2745 grams (96.83 ounces or 6.05 pounds) and is about the size of a romaine lettuce.
Breathing typically improves as the baby descends into the pelvis (lightening), though pelvic pressure and discomfort intensify. The descent signals preparation for labor, and any signs of preterm labor require close attention.
Good nutrition remains essential. A balanced diet rich in vitamins like calcium, iron, and folate supports the baby’s growth and prepares the body for labor and postpartum recovery. Staying hydrated and avoiding high-mercury fish, alcohol, and certain medications are crucial for maintaining a healthy week 36 pregnancy.
Understanding changes in the body and the baby’s development at 36 weeks enables adequate preparation for labor, symptom management, and the prompt seeking of medical care if complications arise.
What To Expect At 36 Weeks Pregnant?
A 36 weeks pregnant mother should expect various symptoms during the third trimester of pregnancy as the baby nears full term. Pressure from the baby causes an overactive bladder (OAB), leading to frequent urination. Hormonal changes and the body’s focus on supporting fetal development result in forgetfulness, often known as “pregnancy brain.” Braxton Hicks contractions (third-trimester symptoms) occur more often but remain irregular, which does not indicate true labor. Physical discomfort and hormonal shifts disrupt sleep and worsen insomnia.
Sharp shooting pains in the pelvis, often called “lightning crotch,” occur when the baby drops lower, increasing pressure on the pelvic nerves. Stomach acid rises into the esophagus, leading to persistent heartburn (GERD). Swollen feet and ankles (edema) occur frequently due to increased fluid retention and pressure on veins. Increased vaginal discharge often indicates labor, primarily upon the release of the mucus plug. Colostrum, the first milk, leaks from the breasts in preparation for nursing.
A 36-week-old baby is about the size of a romaine lettuce and weighs about 6 pounds (2745 grams). Brain and lung development continue, with myelination (nerve coating) improving nerve function. Soft and nearly fully developed bones allow passage through the birth canal. Established sleep patterns alternate between REM and non-REM phases, which is critical for brain development.
Prenatal tests, including Group B Strep screening, blood tests, and ultrasound, during week 36 pregnancy help monitor the baby’s health and detect potential complications like pre-eclampsia. The baby likely assumes a head-down (cephalic) position in preparation for birth.
How Is The Baby Developing At 36 Weeks Pregnant?
Your 36-week baby is the size of a romaine lettuce, weighing 6.05 pounds (2.75 kg) and measuring 18-19 inches (45-48 cm) in length. Measurements include biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and humerus length (HL), highlighting significant aspects of the baby’s physical development.
Several developmental milestones are reached at week 36, including sleep pattern maturation. Organized sleep cycles include rapid eye movement (REM) and non-REM sleep, which are crucial for brain development. The baby now has fully developed eyelids, allowing the regulation of light by controlling pupil constriction. Your baby is likely in a head-down (cephalic) position in preparation for birth.
The brain continues to develop with the advancement of myelination, improving brain and spinal cord communication. Calcium transfer in the bones peaks around week 35, after which bone growth slows, but hardening continues. Fine hairs (lanugo) covering the skin begin to shed.
Coordinated swallowing of amniotic fluid and digestive movements improve. Alveoli continue forming, preparing the lungs for post-birth breathing. The fetus at 36 weeks performs strong movements like sucking and responds to external stimuli, such as the mother’s voice.
How Big Is Your Baby At Week 36 Of Pregnancy?
Baby size at 36 weeks is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 36-week-old fetus is about the size of a romaine lettuce. The 50th percentile measurements for 36-week fetal growth are as follows: the biparietal diameter (BPD) is 89 millimeters, the head circumference (HC) is 321 millimeters, the abdominal circumference (AC) is 317 millimeters, the femur length (FL) is 69 millimeters, and the humerus length (HL) is 61 millimeters.
The 36-week fetus weighs 2745 grams (96.83 ounces or 6.05 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
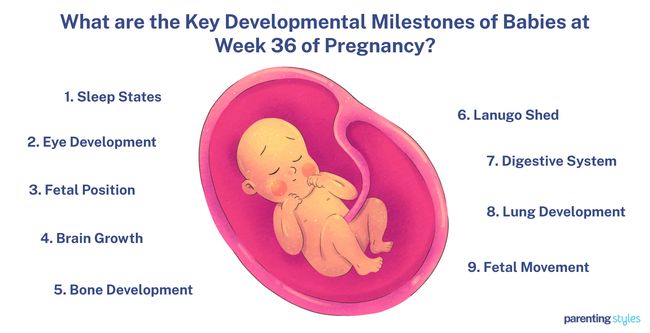
What Are The Key Developmental Milestones Of Babies At Week 36 Of Pregnancy?
Key developmental milestones of babies at week 36 of pregnancy include sleep states, eye development, fetal position, brain growth, and bone development. Here are 9 key developmental milestones of babies in week 36.
- Sleep States: Your baby’s sleep states are already well-organized by 36 weeks pregnant, according to a 2009 study, “Nonlinear analysis and modeling of cortical activation and deactivation patterns in the immature fetal electrocorticogram.” There is a clear distinction between rapid eye movement (REM) sleep and non-rapid eye movement (non-REM) sleep, which are important for cognitive growth and neurological function, indicating positive brain development.
- Eye Development: Your baby’s eyelids are thicker and nearly fully developed at 36 weeks. The edge of the eyelid (eyelid margin) is smooth, and the tarsal glands, which produce oil to lubricate the eyes, now cover a larger portion of the eyelid. The orbicularis oculi muscle, responsible for closing the eyes, moves closer to the skin’s surface, while two other muscles—the levator and Müller’s muscles—connect, allowing the baby to raise the upper eyelid more easily. Fetal optic function further improves as pupillary constriction becomes more consistent at 36 weeks, helping regulate the amount of light entering the retina.
- Fetal Position: Your baby has likely moved into the cephalic (head-down) position at 36 weeks, according to a 1985 study titled “Fetal position during pregnancy,” by Michael John Hughey at Northwestern University School of Medicine. Cephalic position accounted for 93% of the fetuses in the study, while breech (feet-first) position and other positions were observed in 6% and 1% of the babies, respectively. The baby in the cephalic position is tightly curled up, with the back of the head facing the spine, indicating the baby is ready to be born.
- Brain Growth: The baby’s brain undergoes significant development in myelination at 36 weeks, with the proportion of brain volume containing myelinated white matter increasing to 5%. Myelination is the process of coating nerve fibers with a protective myelin sheath, enhancing the speed and efficiency of nerve signal transmission. The myelination of the spinal nerve roots and nerve bundles in the spinal cord has reached a level comparable to a mature brain at week 36. Advanced myelination in the 36th week improves nerve signal efficiency for proper sensory and motor function, indicating the spinal cord is nearing full functional maturity, allowing for better communication between the brain and the rest of the body.
- Bone Development: The amount of calcium making up your baby’s body increases between 24-40 weeks of gestation, with about 80% of fetal bone growth occurring in the third trimester. Rapid bone formation occurs due to the active transport of calcium and phosphorus from the mother to the fetus during the last trimester. Calcium accretion for bone development typically peaks in week 35, dramatically decreasing in the previous five weeks of pregnancy, including week 36.
- Lanugo Shed: Lanugo, the silky, fine hair on the baby’s skin, falls off between 33-36 weeks. The primary function of lanugo is to bind the vernix caseosa (a protective waxy substance covering the fetus’s skin in the womb) to the skin and protect the baby from damaging substances in amniotic fluid. The shed lanugo mixes with the amniotic fluid and is eventually replaced by vellus (thin hair) and terminal hair (thicker hair) on the baby’s body. Some babies do not fully shed the lanugo before birth, and around 30% of newborns are born with lanugo in some areas.
- Digestive System: The baby’s digestive system shows mature movement at 36 weeks, with the stomach muscles working in a coordinated way to help with digestion and gastric emptying. Sodium absorption and transport in the colon develop in the third trimester. Your baby swallows increasing volumes (450 mL/day) of amniotic fluid, indicating the esophagus functions well.
- Lung Development: Fetal lungs mature in preparation for the first gasp of air after birth. Alveolar formation, the final step in lung development, begins at 36 weeks. Babies at 36-40 weeks often breathe through the abdomen, according to a 2003 study, “Ultrasonographic patterns of fetal breathing movements in normal pregnancy,” conducted by E. Cosmi et al. The study further found nasal fluid flow during breathing was 91.2% regular for inhalation and exhalation, indicating the baby’s breathing patterns were consistent and well-coordinated in the 36th week.
- Fetal Movement: Fetal movement increases in strength, frequency, and variation throughout pregnancy. The baby performs various actions in the womb, including sucking motions and whole-body movements like stretching, wiggling, and twisting. The baby, at 36 weeks, responds to the mother’s voice with active movements, such as head-turning.
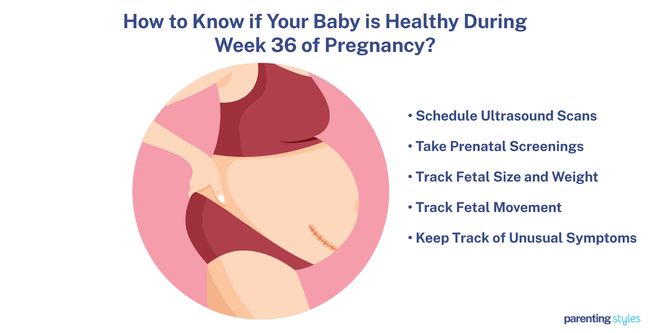
How To Know If Your Baby Is Healthy During Week 36 Of Pregnancy?
To know if your baby is healthy during week 36 of pregnancy, schedule ultrasound scans, take prenatal screenings, track fetal size and weight, track fetal movement, and keep track of unusual symptoms. Here are 5 ways to know if your baby is healthy during week 36 of pregnancy.
- Schedule Ultrasound Scans: An ultrasound exam provides a detailed look at your baby’s anatomy, including the baby’s bones, skull, brain, lungs, liver, and other organs. Ultrasounds help to measure your baby’s size from head to heel, track fetal weight, and monitor the progress of organ development during the last few weeks of pregnancy. Ultrasound results help healthcare providers note any potential abnormalities and issues early on, ensuring your baby’s body is developing and maturing as expected.
- Take Prenatal Screenings: Cell-free DNA (cfDNA) testing is a blood test performed in any trimester to regularly check the baby’s growth and development. cfDNA tests examine the baby’s DNA through the mother’s bloodstream and detect conditions such as Down Syndrome, trisomy 18, and other potential birth defects. Additional prenatal screening and diagnostic tests assess the risk of birth defects and guide further medical testing if needed, ensuring the baby’s healthy development.
- Track Fetal Size and Weight: A 36-week-old baby is approximately the size of a romaine lettuce, weighing around 2745 grams. Regularly attend prenatal checkups, allowing your OBGYN to assess your baby’s size, body proportions, and weight, and to monitor healthy development.
- Track Fetal Movement: Monitoring fetal movement is one of the oldest methods to assess your baby’s health, especially during the last few weeks of pregnancy. Women at 36 weeks of pregnancy are encouraged to regularly check baby movements by counting and recording any dramatic changes. Your OBGYN monitors fetal movement to assess risk factors. Regular fetal movements (10 movements within 2 hours) indicate a healthy baby, while decreased fetal movement is associated with stillbirth, and must be reported to your healthcare provider immediately.
- Keep Track of Unusual Symptoms: Feeling uncomfortable is common as your due date approaches. Cramping at 36 weeks pregnant needs to be evaluated by your OB/GYN. 36 weeks pregnant symptoms not to ignore include cramping, headaches, abnormal vaginal discharge, dizziness, and pelvic pain. Your OBGYN or midwife are the best resources for relieving symptoms, assessing potential issues, and providing appropriate guidance and care for you and your baby.
What Is The Position Of Your Baby At 36 Weeks Pregnant?
Your baby’s position at 36 weeks pregnant is likely cephalic (head-down), according to a 1985 study titled “Fetal position during pregnancy,” conducted by Michael John Hughey at Evanston Hospital and published in the American Journal of Obstetrics and Gynecology. 93% of fetuses in the study were in a cephalic presentation between 33–36 weeks, 6% were in a breech (bottom-down) position, and 1% were in transverse or other positions. Babies in an occiput anterior head-down position face the spine, with the chin tucked into the chest, legs bent, and curled up near the chest, often causing a heavy, tightening feeling in your lower tummy and pelvis. The head-down positioning relieves pressure on the diaphragm and lungs, making breathing easier, although powerful kicks to the rib cage and pressure in the pelvis are common sensations.
Most babies settle into the ideal, safest position of occiput anterior during the 33- to 36-week range in preparation for birth, and the final birth position of your baby is usually identified at 36 weeks. Babies in a non-cephalic position have a 75% chance of turning into a vertex position, while babies in a cephalic position have a 1% chance of changing positions before delivery. Your OBGYN will likely consider options like an external cephalic version (ECV) if the baby remains in a breech or non-cephalic position to help turn the baby into the correct position for a vaginal birth.
Is Your Baby’s Digestive System Fully Matured At 36 Weeks Pregnant?
No, your baby’s digestive system is not fully mature at 36 weeks pregnant since fetal gastrointestinal development continues after birth, with key milestones still in progress. The muscularis externa (the muscle layer in the esophagus) thickens until around 40 weeks. Even after birth, your baby’s stomach produces limited gastric acid due to resistance to pentagastrin, a short peptide. The pancreas, responsible for digestive enzymes, only begins functioning fully in the first few months after birth, according to a 1999 study titled “Development of the human gastrointestinal tract: Twenty years of progress,” by Richard J. Grand et al., published in Gastroenterology.
Some parts of your baby’s digestive system are developed and functional by 36 weeks, such as the stomach, intestines, liver, and pancreas, though not fully mature. The intestines are fully formed by week 13, and swallowing begins as early as 11 weeks, with suckling movements noticeable between weeks 18 and 20.
What Are The Changes In The Mother’s Body At 36 Weeks Pregnant?
Changes in the mother’s body at 36 weeks pregnant include overactive bladder, forgetfulness, Braxton-Hicks contractions, insomnia, and lightning crotch. Here are 9 changes in the mother’s body at week 36 of pregnancy.
- Overactive Bladder (OAB): Increased urination frequency and urgency are common due to pressure on the bladder. Stress incontinence, where urine leaks during physical activity, coughing, or sneezing, becomes more frequent.
- Forgetfulness (Pregnancy Brain): Cognitive changes, often called “pregnancy brain,” lead to forgetfulness and difficulty concentrating. Memory lapses are often due to the redirection of glucose from the mother to the baby and elevated cortisol levels.
- Braxton-Hicks Contractions: Irregular, painless uterine contractions increase in frequency. Braxton-Hicks contractions prepare the body for labor but do not cause cervical dilation or progress to true labor.
- Insomnia: Sleeping difficulties arise from physical discomfort and hormonal changes. Frequent awakenings, bladder pressure, and disrupted sleep cycles lead to increased fatigue.
- Lightning Crotch: Sharp, shooting pelvic pain intensifies as the baby moves lower into the pelvis. Increased pelvic pressure makes certain movements, like turning or bending, more painful.
- GERD (Heartburn): Heartburn and regurgitation become more persistent due to the growing uterus pressing on the stomach. GERD often persists if experienced earlier in pregnancy.
- Edema (Swollen Ankles and Feet): Swelling in the feet and legs is caused by increased venous pressure and water retention. The expanding uterus and rising blood volume contribute to the discomfort.
- Vaginal Discharge: Clear or milky discharge increases, with a thicker, mucus-like consistency possibly signaling the loss of the mucus plug, a sign the body is preparing for labor.
- Leaky Breasts: Breasts sometimes leak colostrum (a thick, yellow fluid preparing the body for breastfeeding) due to increased prolactin, although full milk production is still inhibited by high progesterone levels.
How Big Is A 36 Weeks Pregnant Belly?
A 36 weeks pregnant belly has a fundal height of around 36 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height typically correlates with the gestational age. Therefore, a 36-week baby bump measures around 36 centimeters, between 34 and 38 centimeters. The expanding uterus grows to accommodate the growing fetus. The 36-week pregnant uterus has grown enough to be palpated above the navel level.
The uterine size and growth rate are affected by several factors, such as the mother’s body mass index (BMI), number of pregnancies, variations in amniotic fluid levels, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than women with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. Still, the 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence for using the SFH to predict fetal health.
Do Baby Drops Start At 36 Weeks Pregnant?
Yes, baby “drops” (lightening) typically occur around 38 to 40 weeks of pregnancy, but often happen about two weeks before labor begins for first-time mothers, including week 36, according to a 2006 study titled “Anatomy and Physiology of Pregnancy,” by D.L. Lowdermilk et al., published in Maternity Nursing. Lightening takes place as the baby settles into the pelvis in preparation for birth, relieving pressure on the lungs and stomach while increasing pressure on the pelvis and bladder. Dropping usually occurs closer to labor in women who have previously given birth (multiparas).
Does Baby Drop Lead to Pelvic Pain?
Yes, your baby dropping leads to pelvic pain due to the increased pressure from the growing fetus and expanding uterus, according to a 2020 study from Spain titled “Physiology of intra-abdominal volume during pregnancy,” conducted by Camil Andreu Castelo Branco Flores et al. at the University of Barcelona and published in Journal of Obstetrics and Gynaecology. Discomfort is caused by resistance in the abdominal wall and pressure from the diaphragm, which transfers to the pelvis and the baby’s head. The abdominal cavity reaches capacity as the baby descends, increasing pelvic pain, especially as the baby presses against the pelvic entrance.
Do Contractions Get Stronger At 36 Weeks Pregnant?
Yes, contractions sometimes get stronger at 36 weeks pregnant. However, strong, regular, and increasingly long contractions are signs of active labor. Preterm labor is likely if the mother experiences more than 4 contractions per hour, low back pain, and a mucous-like bloody discharge”, according to a 2004 study from The United States titled “Frequency of uterine contractions in asymptomatic pregnant women with or without a short cervix on transvaginal ultrasound scan,” by Vincenzo Berghella, MD, et al., published in American Journal of Obstetrics and Gynecology.”
True labor contractions happen at regular intervals, whereas Braxton-Hicks (false labor contractions) occur irregularly and are not as intense. Braxton-Hicks contractions help soften the cervix in preparation for labor but are not typically accompanied by other symptoms.
Preterm labor at 36 weeks is linked to complications such as vision and hearing problems, according to a 2023 report by the World Health Organization. Contact your OBGYN immediately if contractions become more frequent, painful, and regular.
What Are The Tips for Prenatal Care During Week 36?
Tips for prenatal care during week 36 include attending prenatal appointments, attending childbirth classes, reporting symptoms, maintaining a healthy diet and lifestyle, and preparing for labor and delivery. Here are 5 tips for healthy pregnancy during week 36.
- Attend Prenatal Appointments: Regular check-ups with an OBGYN, doctor, or midwife assess fetal development and detect any signs of complications such as hypertension and preeclampsia. Antenatal appointments are typically rescheduled every 1 to 2 weeks during the third trimester and involve checking maternal blood pressure and weight, and the baby’s heartbeat and movements. Other prenatal assessments such as ultrasound, blood tests, and urinalysis help identify potential issues and adjust treatment plans as needed until delivery.
- Attend Childbirth Classes: Childbirth classes provide you and your partner with essential knowledge about labor, delivery, and the weeks leading up to childbirth. Childbirth classes often involve discussions with a midwife or OBGYN covering topics such as pain management, the use of medicines during labor, and warning signs to watch for. Choose childbirth classes which prepare you for breastfeeding, parenting, and managing labor-related discomforts. Regular attendance in childbirth classes significantly reduces anxiety and increases confidence in natural childbirth.
- Report Symptoms: Report concerning symptoms like severe morning sickness, vaginal bleeding, contractions, fluid leaks, or unusual pain to your medical provider. Your OBGYN will monitor your blood pressure, weight, and the baby’s heartbeat and movements during prenatal visits. Assessment of pregnancy-related issues and appropriate treatment and support are crucial for ensuring your well-being and the baby’s healthy development as you approach labor.
- Maintain a Healthy Diet and Lifestyle: Eat a varied diet, including all food groups, to support your health and baby’s growth with essential fats, protein, vitamins, and minerals. Be cautious about consuming unpasteurized dairy products, raw or undercooked meat, poultry, eggs, and certain fish to prevent foodborne illnesses. Avoid alcohol use and smoking, which increase the risks of miscarriage, early delivery, and fetal alcohol syndrome. Adequate calcium intake is crucial for your baby’s bone development. Stay hydrated by drinking plenty of liquids, and incorporate fiber-rich foods into your meals to maintain digestive health. Adjust your daily routine by shifting your work posture and avoiding heavy lifting to help ease pregnancy-related discomforts.
- Prepare for Labor and Delivery: Active participation in antenatal education classes as part of prenatal care provides realistic insights into parenting, labor, and pain relief options. Expecting parents must preregister at the hospital, organize key items such as your hospital bag, baby’s clothes, and any necessary medicines, and have important numbers readily accessible, like your OBGYN or midwife’s contact. Avoid airplane travel during the final weeks, and know when to call your OBGYN if labor starts.

What Types Of Foods Are Beneficial To Eat During Week 36 Of Pregnancy?
Types of foods beneficial to eat during week 36 include foods rich in calcium, iron, iodine, choline, vitamins A, B6, B12, C, D, and folate to ensure your health and baby’s growth. Here are 15 beneficial foods to eat at week 36 of pregnancy.
- Calcium-rich Foods: Support strong bones and teeth for your baby, and helps with muscle function and nerve transmission. Try cheese, yogurt, milk, and dark green leafy vegetables.
- Iron-rich Foods: Important for making red blood cells, which transport oxygen to the baby. Common sources of iron include lean red meat, fish, poultry, beans, and prune juice.
- Iodine-rich Foods: Vital for the baby’s brain and thyroid development. Try dairy products, seafood, and eggs.
- Choline-rich Foods: Essential for fetal brain and spinal cord development. Try milk, eggs, beef liver, and tofu.
- Vitamin A-rich Foods: Support vision, immune function, and cell growth. Sources of Vitamin A include sweet potatoes, green leafy vegetables, carrots, and fortified cereals.
- Vitamin C-rich Foods: Aids in the absorption of iron and boosts the immune system. Try broccoli, citrus fruit, tomatoes, and strawberries.
- Vitamin D-rich Foods: Critical for bone health and helps regulate calcium and phosphate. Try fortified milk and fatty fish like salmon and sardines.
- Vitamin B6-rich Foods: Important for brain development and helps metabolize proteins. Consume bananas, pork, whole-grain cereals, and poultry.
- Vitamin B12-rich Foods: Help form red blood cells and maintain the nervous system. Adequate sources of Vitamin B12 include meat, milk, poultry, fish, and eggs.
- Folic Acid-rich Foods: Help prevent neural tube defects and support the placenta. Consume enriched bread, beans, and dark green leafy vegetables.
- Grains: Provide folic acid, fiber, and B vitamins. Try brown rice, millet, oats, quinoa, whole-wheat bread, and bulgur.
- Fruits: Rich in vitamins, minerals, and antioxidants. Choose from fresh fruit, dried fruit, and frozen fruit.
- Vegetables: Provide essential vitamins and minerals. Consume canned vegetables, frozen vegetables, raw vegetables, cauliflower, and green beans.
- Protein: Supports growth and development of tissues. Try poultry, processed soy products, seafood, lean meats, eggs, beans, tofu, soy milk, and organ meats like liver and tongue.
- Dairy: Source of calcium and vitamin D. Try cheese, pasteurized milk, and yogurt.
Why is Vitamin B6 Important?
Vitamin B6 (pyridoxine) is important during pregnancy for supporting fetal brain development, promoting brain health, and helping prevent certain types of anemia and other complications, according to a 2012 study titled “Interventions with Vitamins B6, B12 and C in Pregnancy,” by Lindsay H. Allen et al., published in Paediatric and Perinatal Epidemiology. A vitamin B6 deficiency is not often reported with clinical symptoms, but maintaining adequate levels of vitamin B6 is still important for overall health during pregnancy, including the functioning of the nervous system and the immune system.
Vitamin B6 helps ensure proper fetal brain development during pregnancy and aids in hemoglobin formation and red blood cell production, which helps prevent anemia when iron supplementation alone is inadequate. Vitamin B6 further reduces the risk of complications for the mother, such as hyperhomocysteinemia, a condition associated with pre-eclampsia and preterm birth. Including vitamin B6-rich foods, such as poultry, fish, potatoes, chickpeas, bananas, and fortified cereals, helps the pregnant mother maintain important health benefits in week 36.
What Exercises Can You Do During Week 36 Of Pregnancy?
Exercises you can do during week 36 of pregnancy include walking, swimming, stationary bicycling, stretching, and kegel exercise, according to the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Here are the 5 exercises you can do during week 36 of pregnancy.
- Walking – A simple and effective way to maintain cardiovascular health and ease muscle strain in the joints.
- Swimming – A low-impact exercise relieving joint pressure and providing a safe environment due to the supportive nature of water.
- Stationary Bicycling – A safe alternative to traditional cycling, allowing you to maintain balance and avoid complications from potential falls.
- Stretching – Keeps your muscles flexible and helps reduce aches, especially in areas like the pelvic floor.
- Pelvic Floor Muscle Training (Kegels) – Strengthens the muscles which support the bladder and uterus, reducing the risk of urine leakage and preparing for pushing during delivery.
Aim for at least 150 minutes of moderate-intensity activity each week to maintain cardiorespiratory fitness and muscular strength. Exercises must be done with caution, especially avoiding excessive heat, dehydration, and activities with a high fall risk. Adjust intensity as needed and listen to your changing body, especially regarding your limits.
What Are The Things To Avoid At 36 Weeks Pregnant?
Things to avoid at 36 weeks pregnant include alcohol, smoking, recreational drugs, caffeine, certain medications and supplements, and high-mercury fish. Here are 16 things you must avoid at 36 weeks pregnant.
- Alcohol: Avoid alcohol which causes developmental issues and birth defects, including fetal alcohol syndrome. Even small amounts of alcohol harm your baby, leading to cognitive and behavioral issues, according to a 2020 study titled “Alcohol Use in Pregnancy,” conducted at Oregon Health and Science University and Oregon State University and published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Smoking during pregnancy raises the risks of premature labor, early delivery, low birth weight, and other complications. Severe impacts of smoking and secondhand smoke on maternal and fetal health are outlined in a 2020 study titled, “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy: A Pragmatic Overview of Reviews of Maternal and Child Outcomes, Effectiveness of Interventions and Barriers and Facilitators to Quitting,” by Gillian S. Gould et al. published in the International Journal of Environmental Research and Public Health.
- Recreational Drugs: Recreational drugs continue to pose dangers during pregnancy, leading to long-term health issues for your baby, such as developmental delays and miscarriage.
- Cannabis: Similar to other drugs, cannabis use often causes complications like lower birth weight and affects your baby’s brain development.
- Excessive Caffeine: Limit your caffeine intake to 200mg per day. Too much caffeine increases the risk of low birth weight and complications.
- Certain Medications and Supplements: Ask your OBGYN before taking any medications, over-the-counter supplements, or herbal remedies to ensure safety at 36 weeks. Continue taking prenatal vitamins as recommended to support your baby’s development.
- High Mercury Fish: Continue to avoid fish high in mercury, like swordfish, shark, king mackerel, and tilefish, as mercury exposure impairs your baby’s nervous system. Opt for cooked fish low in mercury for essential nutrients.
- Undercooked or Raw Meat: Stay away from raw or undercooked meats to avoid infections such as toxoplasmosis or salmonella, which are harmful to you and your baby. Make sure all poultry, meat, and eggs are fully cooked.
- Unpasteurized Foods: Avoid unpasteurized dairy, including milk and soft cheeses like brie and feta containing harmful bacteria like Listeria, posing serious risks during pregnancy.
- Deli Meats and Pre-Packaged Salads: Refrain from eating deli meats unless reheated thoroughly. Avoid pre-packaged salads, which often carry harmful bacteria.
- Hot Tubs and Saunas: Avoid hot tubs and saunas as prolonged exposure to high temperatures often increases the risk of overheating, posing risks to you and your baby.
- Strenuous Activities or Contact Sports: Avoid activities with a risk of falling, injury, or abdominal trauma, as your body shape has changed, your center of gravity has shifted, and your balance is likely off at 36 weeks.
- Heavy Lifting: Avoid lifting heavy objects to prevent straining your body, which sometimes leads to preterm labor or back injury.
- Exposure to Harmful Chemicals: Stay away from harsh cleaning products, pesticides, and other toxic substances, as exposure negatively affects your baby’s development.
- Gardening Without Gloves: Wear gloves to avoid contact with soil contaminated with harmful bacteria or parasites, like toxoplasmosis, if you garden.
- Cat Litter: Continue practicing hygiene precautions when dealing with cat litter to avoid toxoplasmosis, especially if you have outdoor cats. Toxoplasmosis poses a risk of infection during pregnancy if proper precautions aren’t taken.
Always follow your OBGYN’s advice and precautions and avoid harmful influences to ensure a safe and healthy pregnancy.
How Important Are Prenatal Classes At 36 Weeks Pregnant?
Prenatal classes at 36 weeks pregnant are highly important for gaining knowledge and confidence about labor and parenting. Parents learn what to expect during childbirth, reducing anxiety and enabling informed decisions, as mothers learn to take control, according to a 2017 study titled, “Perceived Benefits of Childbirth Education on Future Health-Care Decision Making,” by Jane Leach et al.
Prenatal education covers topics such as breastfeeding, newborn care, and the transition into parenthood, offering practical advice for new parents to adapt to life with a newborn. Hearing other women’s perceptions and experiences allows mothers to gain valuable insights and reassurance about the baby’s birth and life afterward.
What Can You Do To Prepare For Labor At 36 Weeks Pregnant?
You can prepare for labor at 36 weeks by attending prenatal classes, choosing a support partner, keeping yourself healthy, and preparing your hospital bag.
Prenatal classes help prepare you for labor and delivery by providing information about what to expect and easing anxiety and uncertainty. Choose a support partner, whether your partner, a family member, or a doula, to assist you in gathering information from your healthcare provider and making a plan for managing labor pain and discomfort.
Ensure you’re getting plenty of rest, eating nutritious foods, and taking the prenatal vitamins recommended by your OBGYN to help your body prepare in the weeks leading up to labor. Pack a hospital bag with essentials such as clothes, toiletries, your birth plan, and important hospital documents to save time and reduce stress when labor begins. Keep in touch with your OBGYN to monitor your health and prevent complications like preterm labor or placental issues, sometimes requiring a cesarean delivery.
What Are The Possible Complications That Can Happen At 36 Weeks Pregnant?
Possible complications that can happen at 36 weeks pregnant include preterm labor, hypertension and preeclampsia, swelling, gestational diabetes mellitus, and vaginal bleeding. Here are 5 possible complications that can happen at 36 weeks.
- Preterm Labor: Preterm labor occurs when the mother gives birth before 37 weeks. Newborn babies born between weeks 35-36 are considered late preterm and often face challenges into childhood, such as health complications and developmental delays. Late preterm infants face a higher risk for developmental problems compared to full-term babies. Preterm labor is often caused by infection-induced inflammation, which triggers contractions, membrane rupture, and cervical changes, leading to early delivery.
- Hypertension (High Blood Pressure) and Preeclampsia: Preeclampsia (PE) is a multi-system disorder typically marked by high blood pressure (140/90 or higher) and protein in the urine. PE is associated with an increased risk for complications like preterm birth. Early detection and management of PE involve regular monitoring, blood pressure control, and other interventions to reduce complications for the mother and baby.
- Severe Swelling (Edema): Edema occurs in the feet, ankles, and legs, causing noticeable puffiness. Increased blood volume, pressure on the inferior vena cava, and body weight result in salt and water retention, leading to swelling. Sudden and severe swelling typically indicates pre-eclampsia.
- Gestational Diabetes Mellitus (GDM): Gestational Diabetes Mellitus (GDM) is a condition characterized by high blood sugar (glucose) levels. Screening for GDM is crucial, affecting approximately 15% of pregnancies worldwide, according to a 2022 study titled “Gestational Diabetes Mellitus – Recent Literature Review.” GDM is associated with obesity and type 2 diabetes in the mother and baby, and if left untreated, leads to complications such as preeclampsia, macrosomia (when the baby grows larger than average), cesarean section births, and fetal issues like respiratory distress or becoming clinically jaundiced after birth. Regular monitoring and management of glucose levels are essential for minimizing risks.
- Vaginal Bleeding: Vaginal bleeding is associated with higher risks of preterm delivery. Early signs of labor, such as contractions and lower back pain, along with bleeding, raise concern for maternal well-being. Multiple episodes of heavy or prolonged bleeding increase the risk of low birth weight and perinatal death, making prompt medical care essential if bleeding occurs.
What are the Chances of Having Preterm Labor at 36 Weeks Pregnant?
There is a reasonable chance of experiencing preterm labor at 36 weeks pregnant. Premature birth is defined as birth before 37 weeks of pregnancy, and the earlier a baby is born, the higher the risks involved. Births between 34 and 36 weeks are called “late preterm” or “near-term”, and make up 71% of all preterm births and about 8% of total births in the United States, according to a 2010 study titled “Late Preterm Birth,” by Ryan W. Loftin et al., published in Reviews in Obstetrics & Gynecology. Babies born at 36 weeks are more developed than infants born earlier, but still face a higher risk of health complications compared to full-term infants, including respiratory distress syndrome (RDS), sepsis, and higher rates of admission to a neonatal intensive care unit (NICU).
Despite the higher risk for health problems in late preterm babies born between 34 and 36, premature birth statistics indicate the risk is much lower than for babies born earlier, with rates of NICU admission decreasing from 16.3% at 34 weeks of gestation to 4.8% by 36 weeks.
Signs of preterm labor at 36 weeks include regular contractions, vaginal bleeding, breathlessness, sudden swelling, premature preterm rupture of membranes (PPROM), severe pains, and preeclampsia.
How Can A Partner Support The Mother At 36 Weeks Pregnant?
A partner can support the mother at 36 weeks pregnant through physical task assistance, lifestyle changes, pregnancy education, physical affection and bonding, and partner communication. Here are 5 ways a partner can support the mother at 36 weeks.
- Physical Task Assistance: Help with chores, errands, and tiring tasks, especially since your partner’s belly is quite large at week 36 of pregnancy. Take responsibility for grocery shopping, meal preparation, and the majority of the housework to lighten your partner’s daily load. Avoid having the mother take on any physical tasks, especially lifting heavy items. Ensure the mother has ample time to rest as the due date approaches.
- Lifestyle Changes: Encourage healthy changes to ensure the mother and baby’s well-being. Support your partner by making healthy changes together, such as giving up smoking and alcohol and maintaining a balanced diet rich in nutrients. Avoid harmful substances and prioritize adequate rest. Do physical activities together, such as brisk walking, to provide support and motivation throughout the final weeks of pregnancy.
- Pregnancy Education: Show an interest in understanding the mother’s experiences to make her feel loved and cared for. Consider joining childbirth classes, touring the birth hospital or birth center, and accompanying the mother to doctor visits. Help with prenatal tests, ask questions, and familiarize yourself with the signs of labor, including how to help time contractions. Assist with practical preparations, such as planning your route to the hospital, getting the necessary admin sorted, and choosing a pediatrician. Learning about pregnancy and childbirth ensures you are well-prepared to support your partner during labor and delivery.
- Physical Affection and Bonding: Offer intimate gestures to alleviate anxiety and enhance feelings of care. Help the mother sit with her feet raised and offer hugs, kisses, and gentle touches to her and the baby bump. Encourage bonding by talking with your baby, and take time to rest together. Play with your baby by gently interacting with the baby bump, creating a connection before birth.
- Partner Communication: Initiate open and honest conversations to understand each other’s feelings, ask questions, and share what you’re experiencing with eac hother. Learn about pregnancy and how to help your partner, and give each other support. Don’t hesitate to reach out to others for additional guidance and advice.
What Prenatal Tests Are Needed At 36 Weeks Pregnant?
Prenatal tests necessary at 36 weeks include GBS screening, blood tests, Hepatitis B screening, ultrasound, and pre-eclampsia screening.
A Group B Streptococcus (a bacteria causing harmful infection in newborns) test is typically taken between 35-37 weeks of gestation. Swabs taken from the lower vagina and rectum of the mother are more effective than cervical swabs alone.
Monitoring maternal iron status is crucial due to the significant role of iron in fetal development in the third trimester. Blood tests like complete blood count (CBC) and antibody screening assess iron absorption and transfer to the fetus, and detect immune reactions affecting iron levels, providing insights into hemoglobin and overall iron reserves. Regular blood tests ensure your baby receives adequate iron from the mother, especially when iron reserves deplete.
Hepatitis B screening identifies high levels of the Hepatitis B virus to help decrease the risks of passing the infection from the mother to child. High viral levels often require antiviral treatment to reduce transmission risk, necessitating testing for Hepatitis B surface antigen (HBsAg) and viral load.
Routine third-trimester ultrasound scans are typically conducted between 30-33 weeks, but are possible throughout pregnancy, including 36 weeks. Scans detect malformations not visible earlier, including urogenital and cardiac issues requiring immediate medical attention at birth. Ultrasound identifies abnormalities from infections, late-presenting neurological conditions, and fetal growth restriction (FGR). Nonstress tests (NSTs) accompany ultrasounds to assess the fetal heart rate and ensure a positive response to movements.
Pre-eclampsia screening at 36 weeks pregnant helps detect signs of high blood pressure and protein in the urine, key characteristics of pre-eclampsia, indicating potential risks for mother and baby. Screenings involve urine culture and kidney function tests, using methods like the urine protein-to-creatinine ratio or dipstick testing.
When To Call Your Doctor If Something Feels Wrong At Week 36 Of Pregnancy?
Call your doctor if something feels wrong at 36 weeks pregnant or if you experience symptoms like heavy vaginal bleeding, persistent headaches, decreased fetal movement, sudden or extreme swelling, and severe vomiting or nausea. Here are 6 symptoms you must report to your doctor at 36 weeks of pregnancy.
- Decreased Fetal Movement: Unusual changes in your baby’s movement call for immediate attention. A noticeable decrease in fetal movement sometimes signals complications, such as fetal growth restriction or stillbirth. Monitor your baby’s movements every day, and call your OBGYN or healthcare provider if you observe fewer than ten movements in an hour.
- Heavy Vaginal Bleeding: Vaginal bleeding is linked to complications including placental abruption and placenta previa. Placental abruption occurs when the placenta separates from the uterine wall before the baby is born, most commonly occurring in the third trimester. Placenta previa is the abnormal implantation of the placenta in the cervical opening, accounting for about 20% of bleeding in late pregnancy. Bleeding is often accompanied by abdominal or belly pain, lower back pain, or severe cramping. Call your OBGYN immediately to determine the cause of your bleeding and get prompt treatment.
- Persistent Headaches: Severe, persistent, headaches are often a sign of preeclampsia (high blood pressure after 20 weeks gestation), especially if accompanied by blurred vision, flashing lights, dizziness and fainting, or other changes in your vision. Preeclampsia causes a spike in the mother’s blood pressure, leading to severe complications if left untreated.
- Sudden or Extreme Swelling: Sudden, severe swelling is often a symptom of preeclampsia, a hypertensive disorder developing after 20 weeks of gestation. Call your OBGYN immediately if you notice sudden or extreme puffiness and swelling in your hands, feet, or face, especially if accompanied by symptoms like headaches and vision changes. Severe or persistent swelling typically indicates a more serious issue.
- Severe Vomiting or Nausea: Severe vomiting sometimes indicates hyperemesis gravidarum (HG), a condition beyond normal morning sickness. HG leads to dangerous levels of dehydration, often accompanied by dizziness or dry mouth, significant weight loss, and complications like electrolyte imbalances or preeclampsia. Contact your OBGYN or visit the emergency department immediately if you experience severe nausea and vomiting preventing food and fluid intake.
- Severe Abdominal Pain/Cramping: Severe abdominal pain or cramping often indicates serious conditions like uterine complications, premature labor, or a miscarriage. Seek urgent medical evaluation immediately if you experience painful abdominal cramps, especially when accompanied by bleeding and lower back pain.
What are the 36 weeks pregnant symptoms not to ignore? 36 weeks pregnant symptoms not to ignore include decreased fetal movement, heavy vaginal bleeding, persistent headaches, sudden swelling, vomiting, and severe abdominal pain. Always trust your instincts during pregnancy. If something feels off at week thirty-six, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
What are the Signs For You to Be Admitted to the Hospital at 36 Weeks Pregnant?
The signs for you to be admitted to the hospital at 36 weeks include regular contractions, vaginal bleeding, breathlessness, sudden swelling, PPROM, severe pains, and preeclampsia. Here are seven 36 weeks pregnant symptoms not to ignore.
- Regular Contractions: Regular and painful uterine contractions are signs of premature labor. Contact your OBGYN immediately if you experience more than 4 contractions in an hour with symptoms such as lower back pain, vaginal discharge, and a tight feeling in your womb. Your OBGYN will check your cervix for dilation to determine if you are experiencing labor.
- Vaginal Bleeding: Vaginal bleeding at 36 weeks is related to several complications. Heavy bleeding with excessive cramping and regular contractions is a sign of preterm delivery. Women with painless vaginal bleeding after 20 weeks of pregnancy must be admitted to the hospital to screen for placenta previa (abnormal placental implantation in the cervical opening), according to a 2012 study titled “Abnormal Placentation Evidence-Based Diagnosis and Management of Placenta Previa, Placenta Accreta, and Vasa Previa,” by Rao, Kiran Prabhaker MD et al., published in Obstetrical & Gynecological Survey.
- Breathlessness: Shortness of breath (SOB) is a common symptom in pregnancy, affecting 60-70% of healthy women. The causes of severe SOB during pregnancy vary widely, ranging from relatively benign conditions like asthma or GERD to life-threatening emergencies such as pulmonary embolism or pneumonia. Go to the nearest hospital for an accurate diagnosis to protect you and your baby’s health.
- Sudden Swelling: Extreme and sudden swelling of your hands and legs suggests pre-eclampsia, a multisystem disorder characterized by high blood pressure and protein in the urine. Preeclampsia causes blood vessels to become leaky, allowing more fluid to seep in and accumulate in other body parts. Hospitalization allows for close monitoring of the symptoms and fetal health.
- Premature preterm rupture of membranes (PPROM): Premature preterm rupture of membranes (PPROM) occurs when the pregnant woman’s waters (amniotic sac) break. PPROM is characterized by a trickle or a gush of fluid from the vagina. PPROM affects approximately 3% of all pregnancies in the United States and is commonly associated with amniotic infection. Mothers who experience PPROM must be admitted to the hospital, as most typically give birth within a week of the rupture.
- Severe Body Pains: Pains in the front and back of the pelvis are not common during pregnancy, making early intervention necessary. Radiating pain and muscle weakness in the spine are signs of lumbar disc herniation, linked to neurological defects. Symptoms of preterm labor at 36 weeks of pregnancy include severe cramping and lower back pain. Go to the nearest hospital if other symptoms such as pelvic pressure, watery vaginal discharge, and regular contractions are present.
- Preeclampsia: Preeclampsia (PE) is a hypertensive disorder during pregnancy. Symptoms of PE include high blood pressure (140/90 or higher), protein in the urine, swelling, sudden changes in vision, and persistent headaches. Preeclampsia is associated with the development of HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome and poor neonatal outcomes, making hospitalization necessary.
Never hesitate to reach out to your OB/GYN if you’re unsure about a symptom. Early intervention makes a significant difference in ensuring a safe and healthy pregnancy.
Are There Prenatal Vitamins Needed To Be Taken During Week 36 Of Pregnancy?
Yes, there are key vitamins to be taken during week 36 of pregnancy to support the mother’s and baby’s health, as recommended by the American College of Obstetricians and Gynecologists (ACOG). Taking prenatal vitamins are essential for meeting the increased nutritional needs of the mother and baby.
Calcium remains crucial, with a recommended intake of 1,000 milligrams for mothers aged 19 to 50. Calcium helps support strong bone development as the baby grows rapidly in preparation for birth and maintains the mother’s bone health.
Iron, an important nutrient throughout pregnancy for placenta development, remains essential at week 36 with a recommended 27 milligrams per day. Iron ensures the mother has enough red blood cells to transport oxygen efficiently to the baby, preventing anemia and supporting the increased blood volume needed as labor approaches.
Iodine, at 220 micrograms, plays a vital role in fetal brain development and supports the mother’s thyroid function, helping to regulate metabolism, which is important as the body prepares for delivery.
Choline, recommended at 450 milligrams daily, remains important for the brain and spinal cord development of the baby. Choline supports the healthy formation of the baby’s nervous system, which is critical in the last stages of growth.
Vitamin A, with a daily recommendation of 770 micrograms, plays an important role in supporting the development of the baby’s heart, lungs, kidneys, and other organs in preparation for birth.
Vitamin C, needed at 85 milligrams per day, helps support the mother’s immune system and aids in tissue repair. Vitamin C assists in iron absorption, helping maintain healthy blood levels.
Vitamin D, at 600 international units, supports the continued development of the baby’s bones and teeth while aiding in calcium absorption for the mother and baby.
Vitamin B6, at 1.9 milligrams, supports the formation of red blood cells and aids in metabolizing proteins and fats, ensuring the mother and baby have the energy and nutrients necessary for the final stage of pregnancy.
Vitamin B12, with a recommended intake of 2.6 micrograms, helps maintain the health of the nervous system and supports red blood cell formation. Adequate B12 intake helps prevent neural tube defects and supports overall fetal development.
Folic acid, at 600 micrograms daily, supports the proper growth of the baby’s brain and spinal cord, supports the placenta, and helps prevent birth defects.
Be sure to consult your healthcare provider to choose the best prenatal supplement for your needs, especially as you approach delivery.
What Does Parenting Styles Suggest About 36 Weeks Pregnant?
Parenting Styles suggests take more rest in week 36 of pregnancy and lean on the support system you’ve put in place over the past few months.
“You’re in the home stretch, and you’re doing an incredible job. Every ache, every sleepless night, and every flutter from your baby is a reminder of the amazing journey you’ve been on. You’re almost there, and soon you’ll be holding your baby in your arms, all of this will be worth it,” says Pamela Li, the Founder and Editor-in-Chief of Parenting Styles.
Congratulations on being 36 weeks pregnant!