37 Weeks Pregnant Symptoms: Week 37 Of Pregnancy And Prenatal Care
37 weeks pregnant symptoms include pregnancy brain, prodromal labor, abdominal and pelvic pressure, body aches, and water breaking. Week 37 Pregnancy symptoms consist of cognitive decline due to hormonal changes, forgetfulness affecting around 80% of pregnant women, and irregular Braxton-Hicks contractions that help prepare the body for labor.
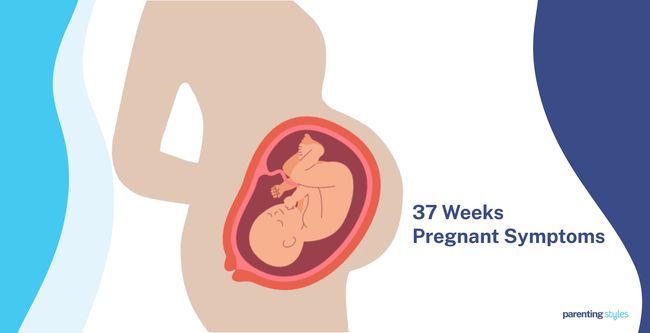
Baby at 37 weeks has reached full-term pregnancy and drops into the pelvis, often causing discomfort and pressure in the abdomen and pelvic region. A 37-week baby has likely settled into the head-down (cephalic) position. The 37-week fetus shows more coordinated, stronger movements.
Back pain and body aches are common as the uterus shifts the body’s center of gravity, loosens joints, and strains the spine. Water breaking signals labor is near when the amniotic sac ruptures, often accompanied by uterine contractions.
Increased bladder pressure leads to frequent urination, and constipation sometimes persists due to hormonal changes and pelvic floor pressure. Indigestion and rib pain are typical as the expanding uterus pushes against the stomach and ribs. These physical changes indicate the body is nearing childbirth.
What is 37 weeks pregnant in months? 37 weeks pregnant is 9 months and 1 week within the third trimester of pregnancy. You now enter the tenth month of pregnancy.
What Are The Pregnancy Symptoms During Week 37?
37 weeks pregnant symptoms include pregnancy brain, prodromal labor, abdominal and pelvic pressure, body aches and pains, and water breaking. 37 weeks pregnancy symptoms are listed below.
- Forgetfulness (Pregnancy Brain): Pregnant women experience a cognitive decline due to hormonal fluctuations, sleep changes, stress, and physiological changes. Forgetfulness is the most reported cognitive symptom, affecting around 80% of pregnant women. High levels of progesterone in the third-trimester account for the decline in memory performance, according to a 2020 study titled “A Pregnant Woman Presenting With Progressively Worsening Dyspnea and Pneumothorax,” conducted by Ramez Sunna et al. at the University of Missouri School of Medicine and published in Chest.
- Prodromal Labor (Braxton-Hicks): Braxton-Hicks contractions are irregular contractions that start around 6 weeks of pregnancy but are only felt in the second and third trimesters. Braxton-Hicks contractions resemble mild menstrual cramps and are not painful but help prepare the body for true labor. Braxton-Hicks contractions are irregular, not felt in the pelvic area, and do not increase in intensity or duration, unlike actual labor contractions.
- Abdominal and Pelvic Pressure: The growing fetus becomes too large for the abdomen during week 37 of pregnancy, causing the baby to drop near the pelvic entrance. The expanding uterus puts pressure on the diaphragm, leading to discomfort in the spine and pelvis. The abdominal wall resists the growing uterus, causing pressure in the abdomen.
- Body Aches and Pains: Low back pain is common and reported by 70.7% of pregnant women in the 2018 study “Musculoskeletal pain and symptoms in pregnancy: a descriptive study,” conducted by Kesikburun et al., making back pain the most common symptom of pain. Physical, hormonal, and vascular changes cause body aches and pains. The growing uterus causes the body’s center of gravity to shift, straining the spine and pelvis. The hormone relaxin loosens the joints, and fluid buildup adds pressure to body tissues. Braxton-Hicks contractions cause uncomfortable tightening or cramping at 37 weeks pregnant. However, painful or frequent cramping is one of the 37 weeks pregnant symptoms not to ignore as it signifies the start of labor.
- Waters Break: Water breaking signals that labor is near. The amniotic membrane surrounding your baby breaks, causing a gush of liquid from the vagina. Water breaking is typically accompanied by contraction in the uterus and discharge of a plug of mucus in the cervix, resulting in bloody discharge.
- Overactive Bladder (Frequent Urination): Overactive bladder (OAB) is a urologic condition characterized by a sudden and frequent urge to pee. OAB is more common in late pregnancy, affecting approximately 88% of pregnant women, according to a 2022 study, “Overactive Bladder during Pregnancy: A Prospective Longitudinal Study,” conducted by Hung-ju Chen et al. Frequent urination with urinary incontinence was most common in the third trimester, affecting approximately 48% of women in the study. Causes of OAB include uterine pressure, fluid overload, increased blood flow in the kidneys, and hormonal changes.
- Constipation: Constipation refers to difficulty passing stool. Dehydration, poor fiber intake, hormonal fluctuations, and pelvic floor changes typically cause constipation during pregnancy. Constipation is associated with hemorrhoids, pelvic floor looseness, and bloating. Constipation is less prevalent during the third trimester, affecting only 21% of women compared to the first and second trimesters, where 35% and 39% of women reported the symptom, respectively, in a 2015 study titled “Pregnancy and postpartum bowel changes: constipation and fecal incontinence,” by Grace Hewon Shin et al., published in the American Journal of Gastroenterology.
- Indigestion (Dyspepsia): Indigestion is pain and discomfort in the upper abdomen. Symptoms include nausea, vomiting, and dull and burning pain. Indigestion in week 37 is likely due to hormone levels and the pressure placed on the stomach and esophagus by the enlarging uterus. Symptoms of indigestion typically occur 1 to 3 hours after eating and worsen at night.
- Rib Pain: Pain in the ribs at 37 weeks pregnant is caused by hormonal and physiological changes. Fluctuations in the hormone relaxin loosen the rib cage, leading to discomfort. The growing uterus further adds pressure to the ribs, causing rib pain. Fetal movement exacerbates the pain by kicking while in a head-down position, according to a 2012 study from Sweden titled “Women’s perceptions of fetal movements in a full-term pregnancy,” conducted by Ingela Radestad et al. in Sweden and published in Sexual & Reproductive Healthcare.

What Is The Importance Of Understanding Being 37 Weeks Pregnant?
The importance of understanding being 37 weeks pregnant lies in recognizing the start of labor is possible at any point. The baby reaches full-term pregnancy status, and the body actively prepares for childbirth. Pregnancy week by week tracking highlights that key signs of labor include contractions, water breaking, or a bloody show. Distinguishing between false labor (prodromal labor) and actual labor is essential for determining when to go to the hospital.
The development of the 37-week fetus nears completion by week 37 pregnancy, with milestones such as a head-down position (ideal for delivery) and fully functioning lungs. Monitoring fetal movements of the 37-week baby, attending prenatal checkups, and undergoing tests like the Group B strep screening are vital for maintaining the baby’s health. Fetal movements change but remain regular and strong.
Physical changes in the mother’s body, including abdominal pressure, body aches, and frequent urination, are common as the uterus expands. Pressure from the growing baby causes discomfort in the pelvic area. Potential complications like preeclampsia, which manifests as sudden swelling or high blood pressure, require close monitoring.
Prenatal care during the 37th week remains essential. Relaxation techniques, childbirth classes, and a diet rich in nutrients like calcium and iron support the well-being of the mother and baby. Gentle exercises such as walking or pelvic floor exercises (Kegels) ease discomfort and improve circulation.
Recognizing the physical and emotional changes and preparing for labor contributes to a smoother transition into delivery and postpartum care.
What To Expect At 37 Weeks Pregnant?
The 37 weeks pregnant mother should expect common symptoms as the body prepares for labor. Forgetfulness, often called “pregnancy brain,” occurs frequently during the third trimester of pregnancy due to hormonal shifts, sleep disturbances, and stress. Prodromal labor, or Braxton-Hicks contractions, are irregular, painless contractions that aid in preparing the body for actual labor. Increased abdominal and pelvic pressure arises as the baby drops lower into the pelvis, causing discomfort in the spine and pelvic region.
Body aches, particularly in the back and pelvis, result from the growing uterus shifting the center of gravity and loosening joints. Water breaking at full-term pregnancy signals the start of labor when the amniotic sac ruptures. Frequent urination, caused by bladder pressure as the baby’s head presses down, remains typical.
Constipation persists for some, though less prevalent at this stage, alongside indigestion caused by the enlarged uterus pressing on the stomach. Rib pain occurs as the uterus pushes against the ribs, with fetal movements potentially intensifying the discomfort. All these third-trimester symptoms indicate the body’s natural progression toward childbirth at 37 weeks pregnant.
How Is The Baby Developing At 37 Weeks Pregnant?
The 37-week baby is about the size of a Swiss chard, weighing roughly 2966 grams (104.62 ounces or 6.54 pounds). Important measurements, such as biparietal diameter (BPD), head circumference (HC), and femur length (FL), are tracked, reflecting continued growth and development. Most babies have settled into a head-down position, ideal for birth, with the head resting in the pelvis, facilitating a smoother delivery. Some babies remain in a breech position, with the head up.
Movements of the fetus at 37 weeks are strong and purposeful, including sucking, swallowing, and practicing breathing. The frequency of movement sometimes seems reduced, yet each movement feels more powerful as space inside the womb decreases. The skin has matured, with all five layers fully developed. A waxy substance called vernix caseosa covers the skin for protection and regulating body temperature after birth. Hair growth is ongoing, with well-formed follicles producing hair.
Major organs, including the kidneys and lungs, are nearly fully developed. The lungs continue preparing for breathing outside the womb. Body systems are maturing, and the endocrine system produces vital hormones that assist with lung development and regulate body temperature. The brain continues developing rapidly, with nerve fibers coated in myelin to enhance communication between brain cells, crucial for controlling movement and other functions after birth. The baby is almost ready for life outside the womb.
How Big Is Your Baby At Week 37 Of Pregnancy?
Your 37-week-old baby is better measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The baby size at 37 weeks is about the size of a Swiss chard. The 50th percentile measurements for 37-week fetal growth are as follows: the biparietal diameter (BPD) is 90 millimeters, the head circumference (HC) is 326 millimeters, the abdominal circumference (AC) is 328 millimeters, the femur length (FL) is 70 millimeters, and the humerus length (HL) is 62 millimeters.
The 37-week fetus weighs 2966 grams (104.62 ounces or 6.54 pounds), according to the 2017 World Health Organization Fetal Growth Charts published in PLoS Medicine.

What Are The Key Developmental Milestones Of Babies At Week 37 Of Pregnancy?
Key developmental milestones of babies at week 37 of pregnancy include position, movement, skin, hair, and major organs. Here are 7 key developmental milestones of babies in week 37.
- Position: Most babies have settled into the head-down (cephalic) position by week 37, which is ideal for birth. The safest position for delivery is when the baby’s head is down in the pelvis and facing the mother’s back (anterior position). Breech positions, where the baby’s head is up and the bottom is down, become less common as pregnancy progresses.
- Fetal Movement: The 37-week fetus shows more coordinated, stronger movements, including stretches, sucking, swallowing, breathing, and grasping. The total number of fetal movements remains steady, though mothers often notice fewer but larger, slower, and more powerful sensations as the baby prepares for birth.
- Skin: Fetal skin reaches full maturity, with all five layers present at 37 weeks. The skin now regulates body temperature, protects against infections, and holds in moisture. The skin thickens as collagen builds up, making it stronger. A protective layer called vernix caseosa, produced by glands, covers the baby to help the skin adjust outside the womb.
- Hair: Hair follicles start forming around 14 weeks as small buds in the skin’s basal layer (outermost layer) and elongate by 18 weeks, alongside the appearance of sebaceous glands, which help the skin lock in moisture. A protective layer of vernix caseosa grows to cover the skin and hair, and fully developed hair follicles grow at 37 weeks in preparation for the baby’s birth.
- Major Organs: Significant growth and functional maturity in the baby’s organs are observed at 37 weeks of pregnancy. The kidneys, weighing around 27 grams (approximately 1 ounce), reach near full development and prepare to regulate fluid balance after birth. The lungs, weighing around 59 grams (approximately 2 ounces), continue developing in preparation for breathing.
- Body Systems: Many of your baby’s body systems have matured significantly in preparation for birth by week 37 of gestation. The endocrine system (controlling hormone release) causes an increase in hormone cortisol levels around 30 weeks, which peaks just before labor. The “cortical surge” helps the baby’s lungs mature and prepares the body to regulate temperature, produce energy, and produce digestive enzymes. The renal system is well-developed, with the fetal kidneys producing urine at 16 weeks and nephrogenesis (kidney formation) typically complete between weeks 34 and 36, preparing the baby for independent kidney function after birth.
- Brain Development: All brain cells originate from a layer of cells called the “germinal matrix,” which surrounds the brain’s ventricles (fluid-filled spaces). The germinal matrix breaks into smaller cell clusters between weeks 36 and 39. Myelination, the process of insulating nerve fibers to improve signal transmission, continues in key areas like the corticospinal tract (responsible for movement) and central white matter (which connects different brain regions) between weeks 33 and 38. The brain’s ventricles are large early in development but shrink as the brain grows, becoming too small to be seen on an MRI by week 35.

How To Know If Your Baby Is Healthy During Week 37 Of Pregnancy?
To know if your baby is healthy during week 37 of pregnancy, monitor fetal size, take prenatal screenings, monitor fetal movement, check fetal heartbeat, and monitor and report suspicious symptoms. Here are 5 ways to know if your baby is healthy during week 37 of pregnancy.
- Monitor Fetal Size: A 37-week-old baby is about the size of a Swiss chard, weighing around 2966 grams (104.62 ounces or 6.54 pounds). Ultrasound consultations with your OBGYN help assess fetal weight and ensure your baby develops as expected.
- Take Prenatal Screenings: Prenatal tests are crucial for monitoring your baby’s health. Cell-free DNA (cfDNA) testing helps track your baby’s growth and development and checks the baby’s DNA through the mother’s bloodstream to detect conditions such as Down Syndrome and trisomy 18. Maternal serum alpha-fetoprotein (MSAFP) screening, or the quad screen, assesses the risk of chromosomal abnormalities or neural tube defects. Prenatal screenings help guide further decisions and discussions with your OBGYN.
- Monitor Fetal Movement: Tracking fetal movement through kick counts is vital for assessing the baby’s health. Recording at least ten movements within 2-3 hours indicates normal development. Be sure to report any significant changes in movement to your OBGYN.
- Check Fetal Heartbeat: Monitoring fetal heart rate (FHR) during prenatal visits helps determine whether your baby receives adequate oxygen and nutrients. Doppler ultrasound and physical examinations assess fetal well-being by ensuring the FHR is within the normal range.
- Monitor and Report Suspicious Symptoms: Symptoms like vaginal bleeding, vision problems (such as blurring or flashing lights), severe vomiting, and extreme swelling in the face, hands, or feet are signs of severe complications like preeclampsia or placenta previa. Uterine contractions occurring six or more times in an hour, with or without other warning signs, suggest preterm labor. Pay close attention to unusual symptoms and immediately report to your healthcare provider for prompt medical attention.
What Is The Position Of Your Baby At 37 Weeks Pregnant?
Your baby is likely in a head-down position at 37 weeks pregnant, known as the cephalic or occiput anterior (OA) position, which is ideal for delivery. Most babies (about 94%) have moved into the OA position by week 37. A baby is not likely to shift from breech (feet or bottom down) to head-down after 36 weeks, according to a 2015 study from Poland titled “The evolution of fetal presentation during pregnancy: a retrospective, descriptive cross-sectional study,” by Piotr Wegrzyn et al., published in ACTA Obstetricia et Gynecologica.
An ultrasound or pelvic exam assesses the baby’s position, including posterior, lateral, or transverse lie positions. Your healthcare provider will likely recommend interventions if your baby is still in a breech position at 37 weeks, such as an external cephalic version (ECV), to help turn the baby into the cephalic position. The baby’s head settles deeper into the pelvis in the cephalic position, a sign that the body is preparing for labor.
Does Your Baby Move More Frequently At 37 Weeks Pregnant?
Yes, fetal movements become more frequent at 37 weeks. Mothers often find movements more noticeable due to the baby’s size and limited uterine space. Fetal movements increase as the baby grows, but the mother’s perception of movement changes as the baby makes more coordinated and slower movements, feeling strong and powerful.
What Are The Changes In The Mother’s Body At 37 Weeks Pregnant?
Changes in the mother’s body at 37 weeks pregnant include rib pain, indigestion, constipation, frequent urination, and pregnancy brain. Here are 9 changes to the mother’s body at week 37 of pregnancy.
- Forgetfulness (Pregnancy Brain): Cognitive decline due to hormonal fluctuations, sleep changes, and stress. High progesterone levels affect memory, with up to 80% of women experiencing forgetfulness.
- Prodromal Labor (Braxton-Hicks Contractions): Irregular, mild contractions resembling menstrual cramps. Braxton-Hicks helps prepare the body for labor but does not increase intensity or regularity.
- Abdominal and Pelvic Pressure: The growing uterus causes pressure on the diaphragm, spine, and pelvis as the baby drops into the pelvic area, resulting in discomfort.
- Body Aches and Pains: Back pain and body aches are common due to changes in posture, loosened joints (from the hormone relaxin), and added pressure from the growing uterus.
- Waters Break (Amniotic Sac Rupture): The rupture of the amniotic sac signals labor is imminent, leading to a gush of fluid from the vagina.
- Overactive Bladder (Frequent Urination): Increased uterine pressure and fluid buildup cause more frequent and urgent urination.
- Constipation: Hormonal changes, pelvic floor pressure, and dehydration lead to difficulty passing stool, often associated with bloating and hemorrhoids.
- Indigestion (Dyspepsia): Hormonal shifts and the enlarged uterus pressing on the stomach cause discomfort, nausea, and burning pain, especially after meals.
- Rib Pain: Relaxin loosens the rib cage, while the growing uterus and fetal movements increase pressure and discomfort in the rib area.
How Big Is A 37 Weeks Pregnant Belly?
A 37-week pregnant belly has a fundal height of around 37 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height typically correlates with the gestational age. Therefore, a 37-week baby bump measures around 37 centimeters, between 35 to 39 centimeters. The expanding uterus grows to accommodate the growing fetus. The 37-week pregnant uterus has grown enough to be palpated above the navel level.
Several factors affect uterine size and growth rate, such as the mother’s body mass index (BMI), the number of pregnancies, variations in amniotic fluid levels, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than women with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. Still, the 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence for using the SFH to predict fetal health.
What Are The Tips For Prenatal Care During Week 37?
Tips for prenatal care during week 37 include attending childbirth classes and regular checkups, engaging in physical activity, practicing relaxation techniques, finding a comfortable sleep position, and preparing for labor and delivery. Here are 6 tips for healthy pregnancy at week thirty-seven.
- Attend Childbirth Classes: Childbirth classes provide essential information about the stages of labor, helping reduce anxiety about the approaching due date. Childbirth classes emphasize the importance of building a support system to assist you through labor and postpartum recovery. Parents often learn about different birthing options, such as natural delivery and epidurals, and various pain management techniques, contributing to informed decisions when creating a birth plan.
- Attend Regular Checkups: Regular prenatal appointments and checkups help monitor fetal growth and maternal health. Your OBGYN checks your weight, blood pressure, and uterine size to address potential issues. Monitoring the baby’s heart rate, growth, and movement helps ensure healthy fetal development. Prenatal tests like a complete blood count, alpha-fetoprotein (AFP), nonstress test, and glucose screening help detect fetal or maternal complications.
- Engage in Physical Activity: Staying active during pregnancy positively impacts the mother’s physical and psychological well-being. Walking, working out, and pelvic floor exercises help improve circulation and alleviate discomfort, such as back pain. Start an exercise routine with gradually increasing intensity to ensure safety and avoid strain.
- Practice Relaxation Techniques: Relaxation helps you stay calm and manage stress at 37 weeks of pregnancy. Find a comfortable spot to sit with your hands on your abdomen. Techniques like mindfulness help lower maternal heart rate, blood pressure, and stress hormones, improving emotional health and promoting better sleep during pregnancy. Relaxation practices help regulate fetal heart rate and motor activity, contributing to a calmer environment inside the uterus and promoting safe sleep habits for the mother and baby.
- Find a Comfortable Sleeping Position: Sleep problems are common during the last few months of pregnancy. Feeling tired and needing more rest is natural as the body prepares for childbirth. Leg cramps, urinary incontinence, shortness of breath, and back pain lead to poor sleep, according to a 2016 study, “The relationship between sleep disturbance in late pregnancy and labor outcomes.” Use pillows to find a comfortable position and increase sleep quality. Sleeping on your side is particularly helpful as your uterus continues to grow and promotes safe sleep.
- Prepare for Labor and Delivery: Key preparations must be made as your due date approaches. Ensure your hospital bag is packed with essentials, including baby’s clothes, and have important numbers readily accessible, like your OBGYN’s contact information. Stay hydrated and familiarize yourself with pain management options as part of your birth plan. Know when to call your OBGYN if labor starts, and explore different birthing centers or hospital options.

What Types Of Foods Are Beneficial To Eat During Week 37 Of Pregnancy?
Types of foods beneficial to eat during week 37 of pregnancy include foods rich in calcium, iron, iodine, choline, vitamins A, C, D, B6, B12, and folate to support your health and your baby’s development. Here are 15 beneficial foods to eat during week 37 of pregnancy.
- Calcium-rich Foods: Calcium helps build strong bones and teeth. Great sources of Vitamin C include sardines, pasteurized milk (low-fat or fat-free), and dark green leafy vegetables (like spinach).
- Iron-rich Foods: Iron helps deliver oxygen to your baby. Find iron in lean red meat, iron-fortified cereals, dried beans, and lentils.
- Iodine-rich Foods: Iodine is important for your baby’s brain development. Try consuming dairy products (like cheese or yogurt), iodized table salt, and eggs.
- Choline-rich Foods: Choline is essential for brain and spinal cord development. Try peanuts, eggs, and soy products (like tofu and fortified soy beverages).
- Vitamin A-rich Foods: Vitamin A helps with cell growth and immune function. Consider sweet potatoes, carrots, and green leafy vegetables.
- Vitamin C-rich Foods: Vitamin 6 helps the immune system absorb iron. Good sources of Vitamin C include strawberries, broccoli, and citrus fruits (like oranges).
- Vitamin D-rich Foods: Vitamin D aids bone health and immune function. Consume fortified milk (including soya milk) and salmon.
- Vitamin B6-rich Foods: Vitamin B6 helps form red blood cells and maintain energy levels. Excellent sources of Vitamin B6 include bananas, pork, and hole-grain cereals (like oatmeal and whole-wheat bread).
- Vitamin B12-rich Foods: Vitamin B12 maintains your nervous system. Try poultry, fish, and meat.
- Folic Acid-rich Foods: Folic acid supports fetal development and helps prevent birth defects. Sources of folic acid include orange juice, dark green leafy vegetables, and enriched bread and pasta.
- Grains: Grains supply energy and fiber. Consume barley, brown rice, quinoa, millet, and bulgur during week 37.
- Fruits: Fruits provide vitamins and minerals for your baby’s growth. Try dried fruit, fresh apples, canned peaches, and bananas.
- Vegetables: Vegetables supply vitamins, minerals, and fiber. Choose from canned vegetables, raw carrots, frozen spinach, and colorful vegetables like bell peppers.
- Protein: Protein supports growth and muscle development. Consume seafood, processed soy products, lean meats, eggs, nuts, and seeds.
- Dairy: Dairy provides calcium and protein. Try pasteurized yogurt, cheese, and low-fat or fat-free pasteurized milk.
What Exercises Can You Do During Week 37 Of Pregnancy?
Exercises you can do during week 37 of pregnancy include walking, swimming, stationary bicycling, stretching, and kegel exercise, according to the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Here are the 5 exercises you can do during week 37 of pregnancy.
- Walking: Walking is a low-impact way to maintain cardiovascular fitness and stay active. It helps strengthen your abdominal muscles and relieve backache.
- Swimming: Swimming reduces strain on joints, strengthens muscles, and helps relieve swelling. Swimming is a great way to engage in muscle-strengthening activity.
- Stationary bicycling: Stationary bicycling is a safe, non-impact cardio workout that reduces the risk of falls and tones muscles without straining joints.
- Stretching: Stretching helps improve flexibility, reduces muscle tension, and relaxes your pelvic floor muscles, which is beneficial for labor.
- Pelvic floor muscle training (Kegels): Kegel exercises strengthen the pelvic muscles, lower the risks of urinary incontinence, and help relax and stretch the perineum in preparation for delivery.
Aim for 150 minutes of moderate-intensity aerobic activity and muscle-strengthening exercises during week 37, but avoid over-exertion. If you have not been active, start with shorter, easier sessions and gradually increase as you feel comfortable. Stay hydrated and avoid high-risk activities like contact sports.
Is it Important to Stay in Bed at 37 Weeks Pregnant?
Yes, it is important to stay in bed at 37 weeks pregnant for high-risk pregnancies and complications like high blood pressure, preeclampsia, or signs of preterm labor. Staying in bed at 37 weeks is not necessary for healthy pregnancies, though taking time to rest as you near term is encouraged. Women on bed rest experience increased fatigue, muscle weakness, and a longer recovery period after birth compared to those who stay active, according to a 2011 study titled “Pregnancy Bed Rest and the Disciplining of the Maternal Body,” conducted by Cristina Alcalde at the University of Kentucky and published in Journal of Gender Studies. Healthy and low-risk pregnant women are encouraged to stay active with gentle activities like light walking to improve circulation, manage pregnancy symptoms, and prepare for labor.
What Can You Do While Staying In Bed At 37 Weeks Pregnant?
You can do a few things while staying in bed at 37 weeks, including creative activities, digital distractions, organizing, relaxing, and supporting your belly. Here are 5 things to do if you are taking bed rest in the 37th week.
- Creative Activities: Engaging in creative activities during pregnancy enhances the mother’s emotional well-being. Singing helps build a bond with the baby, while gentle dancing promotes relaxation and positive emotions through movement. Weaving offers a calming experience and allows the mother to create something meaningful for the baby.
- Digital Distractions: Video calls with friends and family help maintain social connections. Apps provide regular pregnancy updates, help to monitor symptoms, and track fetal development. Online forums offer emotional support and a space to discuss sensitive topics. Digital platforms deliver entertainment through articles, baby name suggestions, and social media groups. Practical tools like hospital checklists and sleep trackers help organize and prepare for birth. Sharing updates and photos on social media enhances connection and excitement.
- Organization Tasks: Several organizational tasks are manageable, from bed for the pregnant mother, such as creating or updating your birth plan and outlining preferences for labor, pain relief options, and infant care. Organizing a hospital bag includes preparing essential items for delivery and postpartum recovery. Researching and compiling information on newborn care, breastfeeding, and postpartum support resources enhances preparedness.
- Relax: Deep breathing exercises and guided meditation help reduce stress and anxiety during week thirty-seven of pregnancy. Calming music creates a soothing environment. Light stretching and gentle movements, like arm circles and pelvic tilts, enhance comfort and relaxation.
- Support Your Belly: Supporting the belly while sleeping reduces the risk of compressing the large vein transporting blood to the heart. Lying on the side, particularly on the left, supports the belly and improves fetal blood flow. Wedge or pregnancy pillows provide additional support in maintaining a comfortable side-sleeping position. Propping up with pillows to achieve a semi-reclined position further improves comfort by alleviating back pressure.
What are the Benefits of Perineal Massage?
The benefits of perineal massage at the 37th week are associated with preparing the mother’s body for childbirth. Perineal massage is a technique used to prepare the perineum (the area between the anus and the vagina) for childbirth by increasing blood flow to the perineum, improving the elasticity of the tissues needed for the delivery. Perineal massage is usually recommended to begin around the 34th week of pregnancy but is not a mandatory part of pregnancy care.
Perineal massage is typically performed by the pregnant woman or by the partner under the guidance of a healthcare provider. The perineum is gently stretched using the fingers for 5 minutes once or twice daily, using a small amount of lubricant to reduce friction and discomfort. Stretching the perineum mimics the effect of the baby’s head and body during vaginal childbirth.
Massaging the perineum lowers the risk of severe perineal tears, according to a 2020 study titled “Antenatal perineal massage benefits in reducing perineal trauma and postpartum morbidities: a systematic review and meta-analysis of randomized controlled trials,” by Ahmed Mohamed Abdelhakim et al., published in International Urogynecology Journal. The study further reported a decreased incidence of episiotomies (a surgical cut made in the perineum to control tearing during childbirth).
Consult your OB/GYN before deciding to do a perineal massage. Your healthcare provider will assess potential risks and benefits before making a recommendation.
What Are The Things To Avoid At 37 Weeks Pregnant?
Things to avoid at 37 weeks pregnant include alcohol, smoking, recreational drugs, certain medications and supplements, and caffeine. Here are 18 things to avoid at 37 weeks pregnant.
- Alcohol: Avoid all alcohol consumption to prevent severe birth defects like fetal alcohol spectrum disorders (FASD). Even small amounts of alcohol negatively affect cognitive and behavioral development, according to a 2020 study, “Alcohol Use in Pregnancy”, by Oregon Health and Science University.
- Smoking and Secondhand Smoke: Smoking increases the risks of premature birth and low birth weight, according to a 2020 study, “Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy”, led by Gillian S. Gould and others. Seek help to quit if necessary.
- Recreational Drugs: Recreational drugs cause serious harm to your baby’s development and lead to birth defects such as developmental issues.
- Cannabis: Cannabis use is linked to low birth weight and developmental delays.
- Excessive Caffeine: Limit caffeine intake to 200 mg per day to reduce risks of miscarriage and low birth weight.
- Certain Medications and Supplements: Always consult your doctor before taking new medications, including herbal supplements, to ensure your baby’s safety.
- High Mercury Fish: Avoid fish high in mercury, like swordfish, sharks, and king mackerel, as mercury harms your baby’s developing nervous system.
- Undercooked or Raw Meat: Uncooked or undercooked meat exposes you to harmful bacteria and increases your risk for infections like toxoplasmosis. Ensure all meat is thoroughly cooked.
- Unwashed Vegetables and Fruits: Thoroughly wash all produce to prevent exposure to parasites and harmful bacteria.
- Deli Meats: Avoid deli meats unless heated until steaming to reduce the risk of listeria, which causes complications.
- Unpasteurized Foods: Avoid unpasteurized dairy products, soft cheeses like brie and feta, and raw eggs, to avoid harmful bacteria.
- Hot Tubs and Saunas: Avoid hot tubs and saunas, as high temperatures harm your developing baby.
- Exposure to Chemicals: Minimize contact with household cleaners, pesticides, and other toxic chemicals.
- Cat Litter: Wear gloves when handling cat litter to avoid toxoplasmosis, a parasite causing pregnancy complications.
- Stress: Emotional and physical stress have negative effects on your pregnancy. Practice stress management techniques to stay relaxed.
- Hair Dye: Hair dye exposure, especially during early pregnancy, has been linked to concerns about birth weight, according to a 2018 study published in BMC Pregnancy and Childbirth. Try looking for safer alternatives if dying your hair is necessary.
- Spicy Foods: Avoid spicy foods and certain gas-triggering foods to prevent heartburn, nausea, and discomfort, common at 37 weeks of pregnancy.
- Lifting Heavy or Bulky Items: Avoid lifting heavy items, carrying bulky items, and placing strain on your body, which causes back pain and contributes to other issues like preterm labor.
Being well-informed about risky substances contributes to a healthy and safe pregnancy. Keep in close touch with your OB-GYN for guidance during the thirty-seventh week of pregnancy.
How Important Are Prenatal Classes At 37 Weeks Pregnant?
Prenatal classes in the third trimester are essential for gaining knowledge and confidence about labor and delivery. Mothers learn about the options for positions during labor and possible delivery methods, helping prepare for childbirth.
Pregnant women who attend prenatal classes have lower hospital anxiety, according to a 2014 study from Iran titled “The Effect of Prenatal Education on the Process of Childbirth,” conducted by Mozhgan Firouzbakht et al. and published in Scimetr. Learning various breathing techniques and massages reduces the fear and pain of delivery, resulting in a lower rate of cesarean deliveries.
The impact of prenatal classes extends into the postpartum period. Mother’s Healthcare decisions are influenced by the values learned during prenatal classes, such as control and trust. Prenatal classes further provide information about the benefits of breastfeeding and how to get started, helping parents better transition into parenthood.
What Can You Do To Prepare For Labor At 37 Weeks Pregnant?
You can prepare for labor at 37 weeks by attending prenatal classes, keeping yourself healthy, contacting a doula, creating a childbirth plan, and preparing a hospital bag.
Prenatal classes teach relaxation techniques that are helpful during labor and delivery. Eating healthy foods and doing moderate exercises prepare your body for labor. Kegel exercises strengthen the pelvic floor muscles, improving muscle control during delivery. Consider contacting a labor coach like a doula for guidance on optimal labor positions. Create a childbirth plan ahead of delivery, including your requests and preferences for giving birth. Prepare a hospital bag containing clothes, toiletries, nursing supplies, and hospital documents to make the start of labor and the journey to the hospital less stressful.
What are the Signs of Labor to Look Out for at 37 Weeks Pregnant?
Signs of labor not to be ignored in the 37th week include a bloody show, pelvic pressure, nausea and vomiting, lower back pain, and uterine contractions. Here are 5 signs of labor to watch out for at 37 weeks pregnant.
- Bloody Show: A “bloody show” is a sign of labor nearing, caused by the release of the mucus plug from the cervix. The mucus plug, which seals the cervix during pregnancy to help prevent infections, is discharged as the cervix softens and dilates. The discharge is usually a mix of mucus, blood, and sometimes light spotting, signaling the body is preparing for labor. Noticing an increase in vaginal discharge or watery fluid is normal as labor approaches, but differentiating bloody show from heavy bleeding, which requires medical attention, is critical.
- Pelvic Pressure: Pelvic pressure is typically an early sign of approaching labor, often felt as a heaviness or discomfort in the pelvis and lower belly. Pelvic pressure increases as the baby drops lower into the pelvis in preparation for birth. The baby’s head presses down into the pelvis as labor approaches, causing pain and discomfort in the abdominal area, too. The process of your baby dropping is called “lightening,” and it typically occurs in the final weeks of pregnancy.
- Nausea and Vomiting: Nausea and vomiting are common during labor, though symptoms are usually mild and subside after emptying the stomach. Discomfort is typically felt in the chest and abdomen, with an urge to vomit building up in the back of the throat. Stomach cramps, which sometimes mimic the feeling of digestive upset, often accompany the onset of labor. Nausea sometimes persists throughout labor but is more likely to occur in the earlier stages. Persistent vomiting, especially later in labor, leads to exhaustion and affects uterine contractions, often requiring medical intervention.
- Lower Back Pain: Many women experience a steady, aching pain in their lower back as labor begins. The pain differs from abdominal contractions, persisting between contractions, and is described as “unrelenting” and “exhausting”. Constant lower back pain close to the end of pregnancy is typically caused by the pressure and stretching in the pelvic area as your body gets ready for birth rather than directly from contractions. Discomfort caused by contractions further contributes to existing lower back pain, intensifying overall discomfort. Continuous lower back pain was reported by around 33% of women as the most severe aspect of labor in a 1987 study from Canada titled “Low-back pain during labor,” by Ronald Melzack et al., published in the American Journal of Obstetrics and Gynecology.
- Uterine Contractions: Regular contractions are one of the most common signs that labor is beginning. Early labor often starts with mild cramps similar to period pain, gradually intensifying as the cervix dilates. The labor process is divided into different stages, with the first stage including a latent and active phase. The latent phase of labor is marked by the onset of intense, regular, painful contractions, according to a 2015 study from Canada titled “Diagnosing onset of labor: a systematic review of definitions in the research literature,” conducted by Gillian E. Hanley et al. at the University of British Columbia and published in BMC Pregnancy and Childbirth. The primary role of contractions during labor is to help the cervix thin out (efface) and open up (dilate) to around 10 cm, allowing the baby to pass through the birth canal.
What Is Dilation In Pregnancy?
Dilation in pregnancy is the widening of the cervix during labor to prepare for childbirth. Proper cervical dilation is crucial for ensuring a smoother passage of the baby through the birth canal and preventing birth complications like protracted labor (progressing slower than usual) or arrested labor (stopping progression after some time). Cervical dilation is often accompanied by pain and menstrual-like cramps, mainly as the lower part of the uterus works to assist in the baby’s descent.
The cervix connects the endometrial cavity to the vagina, playing a vital role in reproduction and childbirth. The cervix must thin (effacement) and widen (dilation) to facilitate the baby’s delivery. Cervical dilations during labor are assessed through a digital cervical exam, in which an OBGYN inserts two fingers in the vagina to estimate the width of the cervical opening. Dilations are measured from 0 to 10 centimeters, with 10 centimeters indicating full dilation, according to a 2024 study titled “Physiology, Cervical Dilation,” conducted by Osarieme Evbuomwan et al. at the State University of New York and published in StatPearls. The cervix is fully open when dilated at 10 cm, signaling that your baby is ready to be pushed out.
How To Distinguish Normal Contractions From Labor Contractions?
To distinguish normal contractions from labor contractions, learn about prodromal labor (Braxton-Hicks contractions) and true labor.
Braxton-Hicks at 37 weeks are sporadic uterine contractions that help prepare the body for labor by softening the cervix without causing cervical shortening. Braxton-Hicks are mild and irregular, resembling menstrual cramping or abdominal tightening, and often subside after resting or changing positions.
True labor pains are stronger and more painful than Braxton Hicks. The contractions start in the lower back and radiate to the front of the abdomen, occurring at regular, gradually shortening intervals. Labor contractions are described as having a “crescendo” pattern as the intensity increases. Labor contractions lead to cervical dilation to allow the baby to pass through the birth canal and are typically accompanied by water breaking, lower back pain, and bloody mucus discharge.
What Are The Possible Complications That Can Happen At 37 Weeks Pregnant?
Possible complications that can happen at 37 weeks pregnant include hypertension and preeclampsia, gestational diabetes, placenta previa, stillbirth, and sudden or severe swelling. Here are 5 possible complications that occur during week 37.
- Hypertension (High Blood Pressure) and Preeclampsia: Preeclampsia (PE) is a pregnancy-related hypertensive disorder occurring after week 20. Symptoms of PE include hypertension (high blood pressure) of 140/90 or higher, protein in the urine, sudden weight gain, persistent headaches, and vision changes. Monitoring and controlling blood pressure is crucial for managing preeclampsia.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) involves having elevated blood sugar levels during pregnancy. GDM increases maternal risks for conditions such as gestational hypertension, pre-eclampsia, cesarean section births, and delivery complications. GDM often results in excessive growth of the baby (macrosomia), leading to breathing and feeding difficulties after birth. Monitor your glucose levels for early detection and effective management of GDM.
- Placenta Previa (Placental Abruption or Abruptio Placentae): Placenta previa is a serious pregnancy complication characterized by a low-lying placenta covering a part or all of the cervical opening. The likelihood of cesarean delivery often increases due to risks associated with severe bleeding and shock, leading to postpartum hemorrhage and maternal death. Signs of placenta previa include painless or heavy vaginal bleeding during the second or third trimester, sometimes triggered by intercourse or medical examinations. Consult your OBGYN for proper testing and management if you experience vaginal bleeding during pregnancy.
- Stillbirth: Miscarriage refers to pregnancy loss before 20 weeks, while losses after 20 weeks, including around 37 weeks of pregnancy, are called stillbirths. Symptoms of stillbirth include decreased fetal movements, cramping, and bleeding. Common factors leading to miscarriage and stillbirth include fetal abnormalities (chromosome issues), maternal health problems (incompetent cervix, hormonal imbalances, chronic conditions), and infections.
- Sudden, Severe Swelling: Swelling (edema) among pregnant women typically affects the lower extremities, including the feet, ankles, and legs. Edema is usually harmless, but sudden and severe swelling signals a more serious condition like preeclampsia, especially if accompanied by high blood pressure, severe headaches, or blurred vision.
What are the Chances of Having Preterm Labor at 37 Weeks Pregnant?
The chances of preterm labor occurring at 37 weeks are very low since preterm labor refers to labor that starts before 37 weeks of pregnancy. A baby born at 37 weeks is considered early term, not preterm, as labor at this stage is close to full term, according to a 2016 study titled “Recurrence of Preterm Birth and Early Term Birth,” by Louis J. Muglia et al., published in Obstetrics & Gynecology. The baby has had significant time to grow and develop in the womb by the 37th week, reducing the risks associated with earlier preterm birth.
Risk factors for preterm labor, such as a previous preterm birth, increase the likelihood of going into labor early. Babies born at 37 weeks generally have good outcomes but still face challenges compared to those born after 39 weeks, including the possibility of long-term issues or neonatal death. However, the chances of risks and complications are much lower than in preterm births.
Signs of early-term labor include a bloody show, pelvic pressure, nausea and vomiting, lower back pain, and uterine contractions.
How Can A Partner Support The Mother At 37 Weeks Pregnant?
A partner can support the mother at 37 weeks pregnant through active listening and communication, physical support, lifestyle changes, emotional support, physical affection, and involvement in maternal health. Here are 6 ways a partner can support the mother at 37 weeks.
- Active Listening and Communication: Focusing on the mother’s words, listening without judgment, and helping your partner feel understood and valued are crucial during pregnancy. Encourage your partner to share fears and worries openly and practice constructive communication to address concerns. Creating a supportive environment where partners feel comfortable expressing feelings helps alleviate stress and strengthen the connection between couples.
- Physical Support: Take on household chores, grocery shopping, laundry, and other physical tasks to relieve your partner of daily burdens, especially with heavy lifting or labor-intensive activities, to ensure your partner avoids unsafe physical work.
- Lifestyle Changes: Encourage and participate in healthy habits, such as preparing healthy meals together, exercising, and avoiding or quitting smoking, to protect the health of the mother and your baby. Coordinated efforts in maintaining a healthy lifestyle help create a supportive environment while waiting for your baby’s arrival.
- Emotional Support: Provide emotional support to enhance your partner’s mental health. Partners must listen, show care, and make an effort to understand the mother’s feelings to reduce anxiety. Make time for one-on-one bonding and connecting through shared experiences to strengthen your emotional connection. Practice patience and offer words of affirmation, compliments, and extra help to strengthen the relationship and decrease stress.
- Affection: Offer your partner a hug, rub her back, and encourage her to put her feet up and relax to help with discomfort and swelling. Small gestures of intimacy help your partner feel loved and cared for, reducing stress and anxiety. Affection enhances security and promotes well-being, according to a 2006 study, “Effective social support: Antecedents and consequences of partner support during pregnancy.”
- Involvement in Maternal Health: Preparing for the baby together and providing practical and emotional support strengthens the bond between partners. Be present at doctor visits, attend prenatal and childbirth classes together, and ask questions to stay informed about the pregnancy. Offer support to your pregnant partner by learning to time contractions or assist in the hospital during labor and delivery.

What Prenatal Tests Are Needed At 37 Weeks Pregnant?
Prenatal tests necessary at 37 weeks include a group B strep test, biophysical profiling, blood and urine testing, an oxytocin challenge test, and amniotic fluid assessment.
Group B Streptococcus (GBS) is a harmful bacteria causing complications like chorioamnionitis, endometritis, and newborn infection. GBS tests typically involve a vaginal and rectal swab performed between 35-37 weeks of pregnancy during a prenatal appointment.
A biophysical profile (BPP) assesses fetal movement, breathing, muscle tone, heart rate, and amniotic fluid levels by combining ultrasound monitoring and nonstress tests. BPP is typically performed in the third trimester and helps ensure the baby receives adequate oxygen and nutrient supply. Fetal health assessments like BPP are recommended to be taken once a week from week 37 until delivery.
Blood tests at a 37-week prenatal checkup include monitoring rubella IgG (antibody) levels to check for rubella immunity. A complete blood count (CBC) assesses blood type and Rh factor, which is crucial for detecting Rh incompatibility (a blood condition characterized by maternal antibodies attacking the baby’s red blood cells). Urine tests and urinalysis detect protein, sugar, and signs of infections to identify complications such as preeclampsia and anemia.
The oxytocin challenge test (OCT) evaluates the baby’s response to oxytocin-induced uterine contractions. The OCT detects conditions like placental insufficiency and predicts potential labor complications, allowing for better management of high-risk pregnancies.
Prenatal care screenings at the 37th week typically include amniotic fluid analysis to measure biochemical markers like creatinine, urea, and uric acid, which indicate fetal kidney maturity.
When To Call Your Doctor If Something Feels Wrong At Week 37 Of Pregnancy?
Call your doctor if something feels wrong at 37 weeks pregnant or if you experience symptoms like heavy vaginal bleeding, fever, sudden or extreme swelling, shortness of breath, and severe vomiting or nausea. Here are 5 symptoms you must report to your doctor at 37 weeks of pregnancy.
- Decreased Fetal Movement: Unusual changes in your baby’s movement call for immediate attention in week 37. A noticeable decrease in fetal movement sometimes signals complications, such as fetal growth restriction or stillbirth. Monitor your baby’s movements daily, and call your OB-GYN or healthcare provider if you observe fewer than ten movements in an hour.
- Heavy Vaginal Bleeding: Vaginal bleeding heavier than spotting and accompanied by unusual cramping or severe pain in the lower abdomen is associated with low birth weight, perinatal mortality, placental abruption, and placenta previa. Contact your OBGYN immediately to determine the cause of your bleeding and receive prompt treatment.
- Fever Over 100°F (37.8°C): Fever, often accompanied by chills, is a sign of infection and indicates a potential underlying issue. Increased risk of fetal neural tube defects, oral clefts, and congenital heart defects occurs when the mother experiences fever during pregnancy, according to a 2014 study from Denmark titled “Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring,” conducted by Anne-Marie Nybo Andersen et al. at the University of Southern Denmark and published in Pediatrics.
- Extreme/Sudden Swelling: Extreme swelling or puffiness in the face, lower extremities, or hands often indicates preeclampsia, a serious pregnancy condition characterized by high blood pressure and protein in the urine. Monitor swelling, especially with persistent headaches, confusion, and vision problems.
- Shortness of Breath: Shortness of breath (SOB) is common during pregnancy, occurring in 60% to 70% of healthy pregnant women. However, severe SOB, especially when accompanied by a racing heart and extreme breathing difficulties, must be checked to rule out underlying heart or lung disorders. Contact your healthcare provider if you notice significant changes in your breathing.
- Severe Vomiting or Nausea: Severe vomiting sometimes indicates hyperemesis gravidarum (HG). HG is characterized by persistent vomiting beyond 20 weeks and is often associated with dehydration, dizziness, significant weight loss, and complications like electrolyte imbalances or preeclampsia. Contact your OBGYN or visit the emergency department immediately if you experience severe nausea and vomiting, preventing food and fluid intake.
What are the 37 weeks pregnant symptoms not to ignore? 37 weeks pregnant symptoms not to ignore include decreased fetal movement, heavy vaginal bleeding, fever, sudden swelling, shortness of breath, and vomiting. Always trust your instincts during pregnancy. If something feels off, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
What are the Reasons for Mothers to be Admitted at 37 Weeks Pregnant?
Reasons for mothers to be admitted at 37 weeks include the onset of labor or pregnancy complications.
Spontaneous labor at 37 weeks requires hospital admission and a closely monitored delivery due to an increased risk of issues during birth, such as the need for intensive care and a higher rate of infant death.
Mothers at 37 weeks pregnant are often admitted due to complications requiring close monitoring, like high blood pressure, often indicating preeclampsia or gestational diabetes.
Are There Prenatal Vitamins Needed To Be Taken During Week 37 Of Pregnancy?
Yes, essential vitamins need to be taken during week 37 of pregnancy to support maternal health and fetal development. Prenatal vitamins play a crucial role throughout pregnancy, according to the American College of Obstetricians and Gynecologists (ACOG).
Calcium is highly recommended, with a daily intake of 1,000 milligrams. Calcium is vital for maintaining the mother’s bone strength and helping the baby’s skeletal system prepare for birth. Calcium demands remain constant as the baby continues to develop strong bones.
Iron, at 27 milligrams, is essential for supporting red blood cell production and ensuring the baby receives adequate oxygen. Iron helps prevent anemia and maintains energy levels as delivery approaches.
Iodine, recommended at 220 micrograms daily, is crucial to support the development of your baby’s brain. Iodine aids in maintaining proper thyroid function and supports the final stages of neurological development.
Choline, at 450 milligrams daily, continues to be important for the baby’s brain and spinal cord health, supporting cognitive functions crucial after birth. Choline helps reduce the risk of birth defects related to the brain and spine.
Vitamin A is needed at 770 micrograms to support the baby’s skin, eyes, and organs development. Vitamin A aids the baby’s lung maturation, which is critical as the baby prepares for independent breathing after birth.
Vitamin C, at 85 milligrams, remains vital to strengthen the mother’s immune system and support tissue repair, especially as the body prepares for labor. Vitamin C assists in the absorption of iron, reducing the risk of anemia.
Vitamin D, recommended at 600 international units, ensures the mother and baby continue to absorb calcium effectively, contributing to healthy teeth and bones.
Vitamin B6, at 1.9 milligrams, supports the development of the baby’s brain and helps regulate the mother’s metabolism.
Vitamin B12, at 2.6 micrograms, assists in red blood cell formation and supports the development of the baby’s nervous system.
Folic acid, recommended at 400 micrograms, supports cell division and tissue growth as the baby prepares for birth.
Consult your healthcare provider for the right 37-week prenatal vitamins or additional supplements you need.
What Does Parenting Styles Suggest About 37 Weeks Pregnant?
Parenting Styles highlights the importance of recognizing nesting behavior as a sign of impending labor. Oxytocin levels rise in early labor, often prompting social interactions like sharing with family or engaging in care-taking and nest-building activities, according to a 2020 study titled “Birth as a neuro-psycho-social event: An integrative model of maternal experiences and their relation to neurohormonal events during childbirth,” by Kerstin Uvnas-Moberg et al., published in Plos One.
“Right before labor began, I suddenly felt the urge to organize my entire closet at midnight. It was amusing. Now I understand it was an early labor sign,” says Pamela Li, Founder and Editor-in-Chief of Parenting Styles.
Congratulations on reaching 37 weeks of pregnancy and preparing for your baby’s arrival!