40 Weeks Pregnant Symptoms: Week 40 Of Pregnancy And Prenatal Care
40 weeks pregnant symptoms include forgetfulness, crowning, contractions, diarrhea, and pelvic pain. Forgetfulness (pregnancy brain) occurs as glucose redirects to the 40 week fetus, affecting memory and focus. Braxton-Hicks and real contractions occur more frequently. True labor contractions progress regularly and cause pain, while Braxton Hicks remain irregular and less painful. Crowning occurs when the baby’s head becomes visible, creating a burning sensation (ring of fire).
Diarrhea signals labor as prostaglandins stimulate the intestines. Pelvic pain worsens as the baby descends, loosening joints and causing discomfort in the hips and lower back. Leg cramps often occur at night due to pressure from the baby and lower calcium levels. Insomnia, caused by discomfort and hormonal changes, leads to fatigue. Nesting, a sudden energy surge, prompts preparation for the baby at 40 weeks. Swelling (edema) in the legs and feet increases as fluid retention rises. Amniotic sac rupture (water breaking) signals labor onset.
Natural labor induction at 40 weeks includes nipple stimulation, oxytocin, exercise, cervical ripening, membrane stripping, and prostaglandin. An OBGYN or midwife administers oxytocin to start labor. Walking or light activity helps trigger contractions. Cervical ripening methods like balloon catheters or medications aid cervical dilation. Membrane stripping, performed by an OBGYN, releases hormones to encourage labor. Prostaglandin medications soften and dilate the cervix. Approval from an OBGYN (obstetrician-gynecologist or OB-GYN) is required before proceeding with any method.
Labor stimulation is sometimes initiated when pregnancy extends beyond 40 weeks due to risks like fetal macrosomia, meconium-stained fluid, and fetal distress. Around 4.1% of pregnancies go overdue, requiring interventions like membrane sweeps or C-sections.
Labor preparation includes regular prenatal appointments, a diet rich in calcium and iron, and Kegel exercises to strengthen the pelvic floor. Moderate physical activity, like walking, reduces discomfort and promotes smoother labor. Rest and relaxation help manage stress and support emotional readiness for delivery.
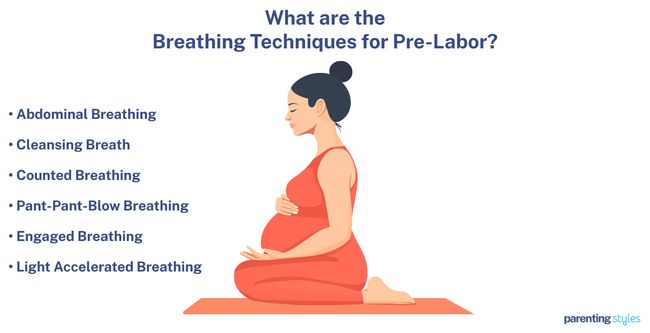
Managing pain and discomfort at 40 weeks involves resting in comfortable positions. Stretching relieves cramps and muscle tension. Breathing techniques like abdominal or cleansing breaths help manage pain from pre-labor contractions.
Complications at 40 weeks include gestational diabetes, stillbirth, hypertension (preeclampsia), placenta previa, and placental abruption. Gestational diabetes increases the risks of delivery complications, fetal macrosomia, and long-term health issues for mother and baby. Stillbirth, or week 40 pregnancy loss after 20 weeks, results from fetal abnormalities, placental problems, or maternal health issues. Hypertension and preeclampsia cause high blood pressure, elevating risks of kidney failure and seizures. Placenta previa, where the placenta blocks the cervical opening, often requires cesarean delivery due to heavy bleeding. Placental abruption, the early separation of the placenta from the uterus, causes significant bleeding and requires immediate medical attention.
Partner support at 40 weeks includes assisting with physical tasks, attending prenatal appointments, maintaining open communication, offering physical affection, and encouraging healthy habits. Partner involvement reduces stress, ensures comfort, and prepares for labor.
Prenatal tests at 40 weeks include routine checkups, blood tests, and biophysical profiling. Prenatal tests monitor fetal health, detect complications like Rh incompatibility, and ensure the 40 week baby receives enough oxygen and nutrients.
Contact your OBGYN for extreme swelling, reduced fetal movement, severe headaches, excessive vaginal bleeding, or intense abdominal pain, which signals serious complications.
Key prenatal vitamins like calcium, iron, iodine, choline, vitamins A, C, D, B6, B12, and folic acid remain essential for maternal health and fetal development.
What is 40 weeks pregnant in months? 40 weeks pregnant is 10 months in pregnancy within the third trimester. You’ve finished the tenth month of pregnancy.
What Are The Pregnancy Symptoms During Week 40?
40 weeks pregnant symptoms not to ignore include forgetfulness, crowning, contractions, diarrhea, and pelvic pain. 40 weeks pregnancy symptoms are listed below.
- Forgetfulness (Pregnancy Brain): Pregnancy brain refers to pregnancy-related cognitive decline, which includes forgetfulness, confusion, reading difficulties, disorientation, poor concentration, and increased absentmindedness. Glucose, the main energy source for maternal brain function, is redirected to the fetus to support growth and development. The fetus’ demand for glucose substantially increases during the third trimester, leaving fewer energy resources for the mother’s cognitive functions. Elevated cortisol levels enhance the redirection of glucose, further affecting brain regions involved with memory. Pregnancy brain affects about 81% of pregnant women, with symptoms most common during the third trimester.
- Baby’s Head Crowns: Crowning occurs when the baby’s head becomes visible at the vaginal opening, indicating the second stage of labor and birth nearing. Some women experience a burning or stinging sensation during crowning (“ring of fire”) as the vaginal tissue stretches to accommodate the baby’s head.
- Contractions: Contractions during week 40 of pregnancy are either Braxton Hicks or true labor contractions. Braxton Hicks contractions are practice contractions preparing the body for labor, but without causing cervical changes. Braxton Hicks are irregular, painless, and do not intensify over time. True labor contractions are more painful, regular, and rhythmic, leading to cervical dilation (opening) and signaling the onset of labor. Real contractions are often accompanied by pain around the bump and the back.
- Diarrhea: Diarrhea involves frequent, loose, and watery stools, affecting about 34% of pregnant women, according to a 2016 study titled “Gastrointestinal diseases in pregnancy: nausea, vomiting, hyperemesis gravidarum, gastroesophageal reflux disease, constipation, and diarrhea,” by Cameron Body et al., published in Gastroenterology Clinics of North America. Increased prostaglandin levels during pregnancy cause intestinal contractions, increasing bowel movements. Diarrhea at or near term typically indicates labor is approaching.
- Pelvic Pain: Pelvic girdle pain (PGP) involves stabbing or burning pain in the pelvis, hips, thighs, and lower back. The baby descends and settles into the pelvis (“baby dropping”) at 40 weeks, lightening abdominal tension, but increasing pelvic pressure. The hormone relaxin loosens joints, making the pelvis unstable. Common triggers of PGP include prolonged postures, walking, sitting, or standing. Twisting, climbing stairs, turning in bed, and having multiple pregnancies typically exacerbate the pain.
- Leg Cramps (Charley Horse): Leg cramps at 40 weeks pregnant are intense, painful muscle contractions in the feet and calves. The expanding uterus adds pressure to the legs and ankles, often triggering cramping. Lower blood calcium levels, caused by the increased relaxin hormone and the baby’s growing demands, further contribute to cramping at 40 weeks pregnant. Leg cramps occur more frequently at night, disrupting sleep and leading to daytime fatigue. Leg cramps affect about 30% of expectant mothers, according to a 2009 study titled “Leg Cramps and Restless Legs Syndrome During Pregnancy,” conducted by Jennifer G. Hensley at the University of Colorado Denver and published in The Journal of Midwifery & Women’s Health.
- Insomnia (Trouble Sleeping): Insomnia is a sleep disorder characterized by difficulty falling or staying asleep. Common causes of trouble sleeping during week 40 of pregnancy include fetal movements, heartburn, physical discomfort, and shortness of breath. 23.7% of pregnancies in the third trimester are affected by trouble falling asleep, according to a 2015 study titled “Insomnia and sleep deficiency in pregnancy,” by Cristina Reichner, published in Obstetric Medicine. Insomnia often worsens right before labor due to the rise in the wake-promoting hormone oxytocin. Sleep problems cause daytime fatigue, worsen labor pain, and increase the likelihood of cesarean section births.
- Nesting: Nesting is the maternal instinct to prepare a safe and comfortable environment for the newborn. Pregnant women experience a burst of energy to clean, organize, and purge household items. Nesting is influenced by hormones and typically peaks in the third trimester.
- Swelling (Edema): Swelling during pregnancy typically affects the lower extremities like the feet, ankles, and legs, and is most common in the third trimester. The expanding uterus compresses pelvic and thigh vessels, while increased body weight and reduced physical activity slow circulation, causing fluid to accumulate in the lower limbs. Blood clots in the veins sometimes worsen swelling by blocking blood flow. Lower limb swelling is frequently accompanied by soreness, a burning sensation, and nighttime cramps, affecting about 80% of pregnant women in the 2017 study from Poland titled “Risk Factors Related to Lower Limb Edema,” conducted by Zbigniew Szygula et al. at the University of Physical Education Kraków and published in Lymphatic Research and Biology.
- Waters Breaking: Water breaking occurs when the amniotic membrane surrounding the baby ruptures, causing fluid to leak from the vagina. Breaking water is sometimes mistaken for urine leakage. Prompt medical attention is necessary if water breaking is accompanied by early labor signs such as regular contractions and bloody vaginal discharge from the loss of mucus plug in the cervix (“bloody show”).
What Is The Importance Of Understanding Being 40 Weeks Pregnant?
The importance of understanding that being 40 weeks pregnant involves understanding that labor and delivery are likely to happen soon. Preparation for contractions, crowning, and the breaking of water remains necessary. Tracking contraction frequency and intensity distinguishes true labor from Braxton Hicks, which occurs irregularly and causes less pain.
The 40 week baby is fully developed (full term pregnancy) and ready for birth, typically weighing 3617 grams (127.59 ounces or 7.97 pounds). Lightening, the baby dropping lower into the pelvis, increases bladder pressure and causes frequent micturition (urination). Knowledge of body changes keeps mothers informed and prepared for discomforts like pelvic pain, leg cramps, and swelling (edema), which occur normally as the body prepares for delivery.
Regular prenatal checkups at 40 weeks are vital. OBGYNs monitor the baby’s health through fetal movement tracking, size measurements, and ultrasounds. Biophysical profiling evaluates the baby’s well-being and placental health. Monitoring detects potential complications like placental abruption or fetal distress, ensuring maternal and fetal safety.
Your baby’s developmental milestones at 40 weeks include lung maturity for breathing outside the womb and the shedding of lanugo, the fine hair once covering the skin. Some lanugo sometimes remains at birth. The baby’s skin thickens in preparation for life outside the womb, and consistent movements, though reduced due to space limitations, indicate a healthy 40 week fetus.
Dietary and exercise habits at 40 weeks support the health of the mother and baby. Pregnancy week by week adjustments to nutrition help ensure the mother is consuming foods rich in calcium, iron, iodine, and vitamins, strengthen the body. Gentle exercises, such as walking and pelvic floor stretches, reduce discomfort and prepare the body for labor. Rest becomes crucial as fatigue often arises due to insomnia, leg cramps, and belly size.
Emotional readiness plays a significant role. Forgetfulness persists, while anxiety and excitement often occur. Support from partners, family, or friends helps with daily tasks and provides comfort. Contacting the OBGYN for extreme swelling, severe headaches, or reduced fetal movement ensures safety and prevents complications. Understanding the factors involved in week 40 pregnancy allows mothers to approach labor with confidence and awareness.
What To Expect At 40 Weeks Pregnant?
The 40 weeks pregnant mother should expect a variety of physical and emotional symptoms as the body prepares for labor and the baby’s arrival. Forgetfulness, often called “pregnancy brain,” is common due to glucose being redirected to the baby, impacting memory and focus. Contractions are third-trimester symptoms that become more frequent, with true labor contractions causing pain and progressing regularly, while Braxton Hicks are less intense and irregular. Crowning occurs during labor when the baby’s head becomes visible, often causing a burning sensation.
Digestive changes like diarrhea in the third trimester of pregnancy often signal labor approaching, triggered by increased prostaglandins stimulating bowel movements. Pelvic pain intensifies due to increased pressure and loosening joints as the baby descends into the pelvis, often exacerbated by movement. Leg cramps, caused by the baby’s growing pressure on the legs and reduced calcium, cause discomfort, especially at night.
Insomnia is common due to physical discomfort and hormonal shifts, leading to difficulty sleeping and increased daytime fatigue. Many mothers experience a surge in energy known as nesting, leading to cleaning and organizing in preparation for the baby. Swelling (edema) in the legs and feet worsens, especially after prolonged standing or sitting, due to fluid retention. Finally, the water breaking signifies the rupture of the amniotic sac, marking the start of labor.
Your baby is the size of a pumpkin at week 40 pregnancy, weighing about 7.97 pounds, with key developmental milestones including fully matured lungs, functional eyes, and continued muscle growth. The baby has likely shed most of the fine hair (lanugo), and the skin is developing to regulate body temperature after birth. Fetal movement remains active at full-term pregnancy, with the baby practicing swallowing and thumb-sucking.
The mother typically undergoes prenatal tests in preparation for labor, such as physical exams, blood tests, and biophysical profiling, to assess the baby’s health and readiness for birth.
How Is The Baby Developing At 40 Weeks Pregnant?
Your 40 week baby is fully developed and ready for birth. The fetus at 40 weeks is about the size of a pumpkin, weighing around 7.97 pounds (127.59 ounces or 3617 grams). One key milestone in the last trimester is the baby dropping lower into the pelvis, a process called “lightening,” which often leads to increased pressure on the mother’s bladder, causing frequent urination. Most of the fine hair (lanugo) covering the baby’s body earlier in development has shed, though some babies still have small patches at birth.
The baby’s lungs are mature, with enough air sacs (alveoli) to support breathing outside the womb. Eye development is advanced, with pupils reacting to light and the baby able to perceive basic shapes and light changes. The skin has fully developed all layers, though the skin continues to mature. The protective waxy coating called vernix has mostly shed, and some dry skin is likely visible after birth.
Internally, the baby’s organs are prepared for life outside the womb. The liver, kidneys, and digestive system function, and the bones have gained significant mineral content. Muscle development is complete, with muscles making up about 20.5% of the baby’s body weight. The baby is actively moving, practicing reflexes such as swallowing and sucking, which are essential for feeding after birth.
Fetal milestones at week 40 indicate the baby is physically ready for birth, with most systems and reflexes supporting life outside the womb.
How Big Is Your Baby At Week 40 Of Pregnancy?
Your baby size at 40 weeks is often measured in biparietal diameter, head circumference, abdominal circumference, femur length, and humerus length rather than crown-rump length (CRL). The 40-week fetus is about the size of a pumpkin. The 50th percentile measurements for 40-week fetal growth are as follows: the biparietal diameter (BPD) is 96 millimeters, the head circumference (HC) is 342 millimeters, the abdominal circumference (AC) is 363 millimeters, the femur length (FL) is 73 millimeters, and the humerus length (HL) is 64 millimeters.
How big is a baby at 40 weeks? The 40-week-old fetus weighs 3617 grams (127.59 ounces or 7.97 pounds), according to the 2017 World Health Organization Fetal Growth Charts, published in PLoS Medicine.
What Are The Key Developmental Milestones Of Babies At Week 40 Of Pregnancy?
Key developmental milestones of babies at week 40 of pregnancy include baby dropping, lanugo, lungs, eyes, and skin. Here are 8 key developmental milestones of babies in week 40.
- Fetus Drops: Fetal drops occur when the baby’s position descends into the lower part of the uterus. The added pressure of the baby on the mother’s pelvis and bladder causes bladder symptoms, such as increased urinary frequency. First-time mothers typically experience the baby dropping 2 weeks before labor onset, often feeling lighter as the pressure on the diaphragm and lungs decreases.
- Lanugo: Lanugo (fine hair covering your baby’s body) typically disappears at week 40, although 30% of newborns still have small patches at birth, sometimes indicating premature birth. Lanugo sheds in the amniotic fluid in the third trimester and is replaced by vellus hair (short, thin hair found on the body) and terminal hair (thicker hairs found on the scalp, armpit, and genitalia) as the baby grows.
- Lungs: Your baby’s lungs at 40 weeks are mature and ready for birth. Alveoli (air sacs responsible for gas exchange) continue to multiply and reach about 100-150 million by the full term. Alveolar formation increases after birth to form into an adult lung. Mature lung development is crucial as the baby prepares for independent respiration outside the womb.
- Eyes: Your baby develops consistent pupillary movements and thicker eyelids beginning at 34-36 weeks, helping limit light exposure to the retina. Retinal development and pathways to the visual cortex become functional by 40 weeks, allowing the baby’s vision to detect patterns, movement, and varying light intensities.
- Skin: Your baby’s skin is anatomically mature at 40 weeks, with all five layers present, but remains functionally immature. Fetal skin is actively changing, helping the baby prepare for birth. Vernix caseosa sheds into the amniotic fluid as the skin matures, causing dry skin patches. A dynamic skin barrier and an increased layer of fat enable protective functions, such as thermoregulation, to keep the baby warm.
- Organs and Body Systems: Your baby’s major organs and body systems are nearly fully developed and ready for birth. The fetal liver is mainly responsible for producing blood cells, with most metabolic functions supported by the mother until term. Some liver enzymes remain immature at birth, continuing to develop after delivery. The kidneys have already formed all filtering units (nephrons), essential for waste removal. Lipid and protein levels increase by 40 weeks, while mineral levels remain steady. Bone mineralization quadruples between 25 and 40 weeks, with full-term bone mineral content reaching approximately 62.4 grams. The colon and intestines are maturing to support digestion after birth.
- Muscles: Muscle cells are fully developed by the end of the third trimester, with most growth occurring at 38 weeks. Your baby’s muscle fibers remain small but increase in number and density, making up about 20.5% of the baby’s body weight at 40 weeks.
- Fetal Movement: Fetal movement becomes more active and intentional at 40 weeks as brain development advances. Full-term movements include making fists and thumb-sucking. Swallowing amniotic fluid helps regulate fluid volume, which is important for maintaining a balanced environment. The amount of amniotic fluid swallowed increases to about 500 mL per day during the third trimester, supporting the development of the baby’s sense of taste and smell (chemosensation). Sucking and swallowing actions stimulate sensory receptors and help prepare the baby for feeding after birth.
How To Know If Your Baby Is Healthy During Week 40 Of Pregnancy?
To know if your 40-week-old baby is healthy, track fetal movement and fetal size, attend prenatal appointments, take prenatal screenings, and perform ultrasonography. Here are 5 ways to know if your baby is healthy at 40 weeks.
- Track Fetal Movement: Monitor fetal movements daily by tracking kick counts. Regular and strong fetal movements (10 movements within one hour) typically indicate a healthy baby, while decreased fetal movement is associated with stillbirth. Observe fetal movements closely and report changes in the baby’s movements, such as less frequent or weaker movements than usual.
- Track Fetal Size and Weight: A 38-week-old fetus is approximately the size of a pumpkin, weighing around 3617 grams (127.59 ounces or 7.97 pounds). Attend regular prenatal checkups and have your OBGYN assess your baby’s size, body proportions, and weight to ensure healthy fetal development.
- Attend Prenatal Appointments: Regular visits with your OBGYN are essential for monitoring your baby’s health and ensuring proper development. Have your OBGYN check the baby’s position and discuss signs of labor, such as contractions. Make sure to report any unusual symptoms, such as severe headaches, vision issues like blurriness, light sensitivity, or seeing spots and flashes, to address potential health complications.
- Take Prenatal Screenings: Prenatal screening tests, such as cell-free DNA (cfDNA) testing, are performed throughout pregnancy to assess fetal health and detect genetic conditions like Down Syndrome and trisomy 18. Diagnostic tests help identify health conditions or birth defects early on, allowing for immediate medical interventions. Discuss the results with your OBGYN to proceed with the necessary interventions.
- Perform Ultrasonography: An ultrasound uses high-frequency soundwaves to provide a clear view of your baby in the womb on a screen. A biophysical profile, which evaluates fetal movement, heart rate, and amniotic fluid levels, is often performed at 40 weeks to ensure your baby’s health and well-being as you approach delivery.
What Are The Changes In The Mother’s Body At 40 Weeks Pregnant?
Changes in the mother’s body at 40 weeks pregnant include leg cramps, insomnia, nesting, swelling, and edema. Here are 10 changes to the mother’s body at week 40 of pregnancy.
- Forgetfulness (Pregnancy Brain): Cognitive changes such as forgetfulness, confusion, and poor concentration occur as glucose is redirected to the fetus for development, reducing energy for the mother’s brain.
- Baby’s Head Crowns: The baby’s head becomes visible at the vaginal opening (crowning), signifying the second stage of labor and sometimes causing a burning sensation as the vaginal tissue stretches.
- Contractions: True labor contractions become regular and painful, causing cervical dilation, while Braxton Hicks contractions remain irregular and painless, preparing the body for labor.
- Diarrhea: Frequent, loose stools occur as increased prostaglandin levels stimulate the intestines. Diarrhea at 40 weeks often indicates labor is imminent.
- Pelvic Pain: The mother experiences pelvic girdle pain as the baby descends into the pelvis due to joint loosening from relaxin, causing discomfort in the hips, thighs, and lower back.
- Leg Cramps (Charley Horse): Painful cramps in the legs and calves are triggered by pressure from the expanding uterus and lower blood calcium levels, often worsening at night.
- Insomnia (Trouble Sleeping): Difficulty sleeping is caused by physical discomfort, fetal movements, and hormonal changes, leading to fatigue and worsened labor pain.
- Nesting: A surge of energy driven by hormones prompts the mother to clean and organize in preparation for the baby’s arrival.
- Swelling (Edema): Fluid retention in the feet, ankles, and legs occurs due to slowed circulation from the expanding uterus and reduced physical activity, often accompanied by soreness and nighttime cramps.
- Waters Breaking: The rupture of the amniotic sac causes fluid to leak from the vagina, signaling the start of labor if accompanied by contractions and a bloody show from the cervix.
How Big Is A 40 Weeks Pregnant Belly?
A 40-weeks pregnant belly has a fundal height of around 40 centimeters. The fundal height or symphysis-fundal height (SFH) is the distance from the pubic symphysis (a joint at the front of the pelvis) to the top of the uterus (fundus). The fundal height typically correlates with the gestational age. Therefore, a 40-week baby bump measures around 40 centimeters, between 38 to 42 centimeters. The expanding uterus grows to accommodate the growing fetus. The 40-week pregnant uterus has grown enough to be palpated above the navel level.
Several factors affect uterine size and growth rate, such as the mother’s body mass index (BMI), the number of pregnancies, variations in amniotic fluid levels, or the different sizes of the fetus. For example, women with higher BMI tend to have a slightly larger fundal height measurement than women with lower BMI.
Fundal height measurement has been routinely used in clinical practice to monitor fetal growth. Still, the 2016 World Health Organization (WHO) ANC Guidelines concluded there was inadequate evidence for using the SFH to predict fetal health.
What Are The Major Signs Of Labor At 40 Weeks Pregnant?
Major signs of labor not to be ignored at 40 weeks include uterine contractions, backache, water breaking, loss of the mucus plug, and cervical dilation. Here are 8 key signs labor is near at 40 weeks of pregnancy.
- Uterine Contractions: Strong and regular contractions every 3 to 5 minutes signal the first stage of labor. Labor contractions intensify over time and are characterized by a wrapping pain in the belly and lower back. True labor contractions lead to cervical dilation (widening) and effacement (thinning) unlike painless Braxton-Hicks contractions.
- Backache: Back pain as a sign of labor is caused by the baby’s position in the pelvis. The baby’s head presses against the spine, creating pressure and discomfort. Loose joints, caused by relaxin hormones, make the pelvis unstable, contributing to lower back pain. Back pain intensity varies depending on the mother and baby’s position during labor. Lower back pain was reported by 74% of women during labor, according to a 1987 study from Canada titled “Low-back pain during labor,” by Ronald Melzack et al., published in the American Journal of Obstetrics and Gynecology. Continuous low back pain, described as the most intense labor pain, was reported by 33% of women in the study.
- Water Breaking: Your water breaks when the amniotic sac ruptures, resulting in a slow leak of amniotic fluid from the vagina. Water breaking at 40 weeks pregnant indicates vaginal delivery. Water breaking is often mistaken as urine, and a healthcare provider conducts assessments such as pH tests to determine if the liquid is amniotic fluid.
- Loss of Mucus Plug: The mucus plug is a sticky, thick substance of antibodies and proteins involved in the mother’s immune response. The plug forms a protective mucus over the cervix during pregnancy. Cervical dilations cause the mucus plug to be dislodged, resulting in a noticeable increase in vaginal discharge.
- Cervical Dilation: Thinning (effacement) and opening of the cervix (dilation) occurs during labor to allow the baby to pass through the vagina. The cervix slowly dilates to approximately 6 centimeters during the latent phase and rapidly widens to 10 centimeters during the active phase. Mothers who have previously given birth or had vaginal delivery typically dilate more.
- Bloody Show: Bloody show is a bloodstained vaginal discharge signaling labor. The discharge consists of mucus and a small amount of blood, typically not affecting the mother’s blood flow. Some women experience a bloody show-up to three days before labor begins.
- Baby Drops (Lightening): The baby at 40 weeks pregnant descends and settles into the pelvic cavity, causing pressure in the pelvis. The descent decreases the fundal height (distance between your public bone and the top of your uterus) and the pressure in the abdomen, resulting in a lighter sensation.
- Stomach Issues: Gastric emptying (movement of food and liquid from the stomach to the small intestine) slows down during labor, resulting in stomach issues. Women in labor typically experience nausea and vomiting, with the vomit containing remnants of food eaten several hours earlier, according to a 1970 study, “Gastric emptying time in late pregnancy and labour,” conducted by Joseph S. Davidson et al.

How to Induce Natural Delivery At 40 Weeks Pregnant?
To induce natural delivery at 40 weeks, use nipple stimulation, oxytocin, exercise, cervical ripening, membrane stripping (sweeping of the membranes), and prostaglandin with approval from your OB/GYN. Here are 6 ways to induce natural delivery in the 40th week.
- Stimulate Nipples: Nipple rolling or gentle rubbing elevates oxytocin levels, leading to uterine contractions and cervical ripening. Massaging the breast and nipples for 15 minutes thrice a day helps induce spontaneous labor onset and increases the likelihood of vaginal delivery, according to a 2022 study titled “Cervical ripening and induction of labor,” by Vernon Wheeler et al., published in American Family Physician.
- Receive Oxytocin: Oxytocin is the most commonly used medication to stimulate contractions and induce labor, typically administered intravenously. Variations in uterine receptivity among pregnant women influence how effectively oxytocin induces labor, but the results are usually consistent across different dosages. Oxytocin use carries potential risks, such as excessively rapid contractions with higher doses and postpartum hemorrhage (bleeding) with lower doses, and the American College of Obstetricians and Gynecologists recommends continuous monitoring by your healthcare provider during the process.
- Perform Exercise: Moderate physical activities like walking increase uterine contractions, triggering labor onset. Walking for 30 minutes thrice a week helps low-risk pregnancies induce labor at term, according to a 2020 study titled “Physical exercise at term for enhancing the spontaneous onset of labor: a randomized clinical trial” by Isabel Barros Pereira et al.
- Ripen Cervix: Ripening the cervix stimulates contractions to initiate labor. OBGYNs use medications or devices, such as inserting single- and double-balloon catheters through the cervix and into the intrauterine cavity, to induce cervical dilation. Single-balloon catheters enhance the effectiveness of medications like dinoprostone, misoprostol, and oxytocin in facilitating labor.
- Strip Membranes: Membrane stripping (sweeping) involves inserting a finger into the cervix and using circular motions to detach the amniotic sac from the uterine wall, typically performed by a medical professional. The separation stimulates the release of hormones, such as prostaglandins, resulting in cervix ripening and inducing labor. Membrane sweeping lowers the likelihood of post-term births and reduces the need for further medical interventions.
- Take Prostaglandin: Prostaglandin is a medication helping the cervix soften and dilate. The most common prostaglandin for labor induction is misoprostol (PGE1), which is typically administered vaginally, sublingually (under the tongue), or buccally (inside the cheek). Vaginal misoprostol at 50 µg has the greatest likelihood of resulting in vaginal delivery within 24 hours, according to a 2023 study titled “Methods for the induction of labor: efficacy and safety,” by Luis Sanchez-Ramos et al., published in the American Journal of Obstetrics and Gynecology. Prostaglandin is not recommended for mothers with prior cesarean delivery due to increased risks of uterine rupture.
How Common Are Overdue Pregnancies?
Overdue pregnancies (late-term pregnancies) are relatively uncommon, with only 4.1% of pregnancies classified as late-term and 95.9% occurring in the term range, in a 2023 study titled “The Incidence and Outcomes of Late-Term Pregnancy,” by Amene Ranjbar et al., published in Cureus. The study found late-term pregnancies were more prevalent in first-time mothers and carry a higher risk of complications such as fetal macrosomia (larger-than-average babies), meconium-stained (fetal stool) amniotic fluid, and fetal distress.
Late-term pregnancies sometimes lead to interventions like membrane sweeps or the use of forceps, vacuum devices, or even a C-section to assist in delivery. Labor is induced in some cases if the baby is overdue. Late-term pregnancies had a lower risk of low birth weight than term pregnancies in the study. Late-term pregnancy poses other health risks, however, due to decreased placental function, reducing the supply of oxygen and nutrients to the baby.
What Are The Best Tips For Pregnant Mothers At Week 40?
The best tips for pregnant mothers in week 40 include attending antenatal appointments, labor induction, kegel exercises, physical activity, and resting and relaxing. Here are 5 of the best tips for healthy pregnancy at week 40.
- Attend Antenatal Appointments: Routine antenatal appointments are recommended weekly from week 37 until delivery. Women with uncomplicated pregnancies often require fewer visits, amounting to about 16 appointments from 6 to 41 weeks, while mothers experiencing issues usually require more. Keep in touch with your healthcare provider to address potential medical conditions, ensure the baby arrives on time, and receive necessary vaccinations for maternal and fetal health.
- Labor Induction: Labor induction methods, such as membrane stripping and amniotomy, increase the likelihood of spontaneous labor within 24-48 hours, but the procedure must be approved or conducted by your healthcare provider. Membrane stripping involves sweeping a gloved finger around the cervix to separate the amniotic sac from the uterine walls. Amniotic membrane separation leads to prostaglandin release, helping with cervical ripening. Amniotomy involves artificially rupturing the membranes using a plastic hook, stimulating oxytocin and prostaglandin release to help induce labor.
- Kegel Exercises (Pelvic Floor Muscle Training or Pelvic Floor Exercise): Kegel Exercises help strengthen and improve flexibility in the pelvic floor. Pregnant women are recommended to perform pelvic floor training daily to reduce risks of urinary incontinence (involuntary leakage of urine when laughing, sneezing, or coughing).
- Physical Activity: Exercises like walking and stretching improve blood circulation, relieve muscle tension, and reduce swelling, pain, and discomfort. Physically active women are less likely to experience exhaustion during childbirth and have a lower risk of needing artificial labor induction, episiotomy (a small cut between the vagina and perineum during delivery), abnormal heart rhythms, or cesarean sections, according to a 2013 study from Poland titled “Types of Physical Activity during Pregnancy” by Makara-Studzińska, Marta, et al., published in Polish Annals of Medicine. Stay hydrated and avoid overexertion when working out.
- Rest and Relax: Relaxation positively influences emotional well-being, leading to fewer depressive symptoms, anxiety, and worries, according to a 2012 study from Switzerland titled, “Relaxation during pregnancy: what are the benefits for mother, fetus, and the newborn? A systematic review of the literature” by Nadine S. Fink et al. and published in The Journal of Neonatal and Perinatal Nursing. Relaxation techniques like guided imagination and massage help reduce stress, slow maternal heart rate, and improve blood pressure. Consider learning breathing exercises to help you stay calm during labor and conserve energy for childbirth. Try hot compress and warm baths to help relieve lower back pain.

How To Manage Pain And Discomfort At 40 Weeks Pregnant?
To manage pain and discomfort at 40 weeks, find comfortable resting positions, move around, stretch, and consult your OBGYN regarding compression, hydrotherapy, and heat therapy. Below are 7 ways to manage pain and discomfort during week 40 that are used with approval from your OBGYN or midwife.
- Find Comfortable Resting Positions: A lumbar support while sitting and elevate your feet on a small stool to help alleviate discomfort. Experiment with various sleeping pillows and cushions to find the best support for your spine, abdomen, and legs. Using a heat pack on sore areas helps soothe musculoskeletal tension. Always consult your provider for personalized strategies to manage discomfort effectively.
- Engage Physical Activities: Staying active can help alleviate pain and promote well-being.
- Perform Stretches: Stretching and staying active with daily activities like walking instead of prolonged sitting or standing reduces low back pain. Try stretching to improve muscle strength, resistance, balance, and flexibility. Remember to exercise cautiously, avoid overexertion, and stay hydrated to protect yourself and your baby’s health.
- Apply Compression: Compression therapy (compressive bandaging and using compression garments like support hoses or compression socks) improves blood flow, reducing swelling, according to a 2017 study from Poland titled “Risk Factors Related to Lower Limb Edema, Compression, and Physical Activity During Pregnancy: A Retrospective Study” by Katarzyna Ochalek, PT et al. at the University of Physical Education and published in Lymphatic Research and Biology. Wearing low-heeled shoes and using footstools promote better posture and ease lumbar discomfort. Applying heat packs and icing sore areas contributes to relieving back pain.
- Use Hydrotherapy: Hydrotherapy involves immersing the body in water, such as pools or tubs, to relieve pain and discomfort. The sensation of weightlessness eases the strain on muscles and joints, while the warmth of the water reduces muscle tension and spasms. The combination improves blood circulation and oxygen flow, promoting healing in body tissues, according to a 2010 study titled “The Effect of Aquatic Physiotherapy on Low Back Pain in Pregnant Women” by Esther Intveld et al. and published in the International Journal of Aquatic Research and Education.
- Use Heat Therapy: Heat therapy involves applying heat to different body parts, such as the back, to relieve pain and discomfort. Taking warm baths and showers helps soothe headaches and manage insomnia. Washing and massaging the breasts with warm water reduces breast pain and tenderness, and keeping the feet warm helps with frequent urination. Heating pads typically ease back pain. Remember to avoid hot tubs and saunas to prevent risks of overheating.
- Manage Cramping: Managing cramps typically involves massage, which is further associated with reduced leg and back pain, depression, and anxiety during pregnancy, according to a 2010 study titled “Pregnancy and labor massage” by Tiffany Field at the University of Miami School of Medicine and published in Expert Review of Obstetrics & Gynecology. Taking warm baths or using heat packs helps relax the muscles and joints, soothing muscular discomfort and tension.
Pain management requires guidance from an OBGYN or midwife. Consult your healthcare provider for advice before proceeding with any method.
What Are The Breathing Techniques For Pre-Labor?
Breathing techniques for pre-labor include abdominal, cleansing, counted, pant-pant-blow, engaged, and light accelerated breathing. Here are 6 types of breathing techniques to practice and learn before labor.
- Abdominal Breathing: Abdominal breathing involves slowly inhaling through the nose, holding the breath briefly in the stomach, and exhaling through the mouth. The technique relaxes the abdominal muscles, helping to reduce pain during contractions. Deep, slow abdominal breaths help decrease fatigue and improve oxygen flow to the womb, supporting the mother during labor.
- Cleansing Breath: Cleansing breath involves an exaggerated inhalation through the nose followed by an exhalation through the mouth to organize breath and gather focus and control during labor. The technique is recommended for mothers to signal the start and end of a contraction or the beginning of another breathing pattern.
- Counted Breathing: Counted breathing involves inhaling through the nose for a specific count (e.g., 1-5), then exhaling through the mouth for a matching count (e.g., 5-1). A 1-2 count pause is sometimes added to start a new breathing cycle.
- Pant-Pant-Blow Breathing: Pant-pant-blow breathing involves a “hee-hee-hoo” pattern of breathing shallowly through the mouth. Pant-pant-blow breathing helps reduce the active stage of labor when performed with shallow and accelerated breathing, according to a 2017 study titled “The effects of breathing techniques training on the duration of labor and anxiety levels of pregnant women.” Practicing the technique before labor is essential to ensure effect in the labor duration.
- Engaged Breathing: Engaged breathing involves a focused deep breath, followed by slow inhalation through the nose and exhalation through pursed lips. The breathing remains slow and controlled, with a gradual exhale during contractions.
- Light Accelerated Breathing: Light accelerated breathing involves rapid, shallow breaths through the mouth, resembling a pant. The rate and depth of breathing are adjusted based on contraction intensity, becoming quicker and lighter as contractions strengthen. Light accelerated breathing decreases anxiety and reduces the active stage of labor duration, according to a 2017 study titled “The effects of breathing techniques training on the duration of labor and anxiety levels of pregnant women.”
Pregnant women are encouraged to learn breathing techniques during prenatal care to reduce discomfort and better manage contractions. Learning and practicing breathing techniques before labor helps you achieve the best results for your childbirth experience. Your doctor and midwife guide you in choosing different methods during labor. Follow the instructions provided by your healthcare provider.
What Are The Tips For Prenatal Care During Week 40?
Tips for prenatal care during week 40 include attending antenatal appointments, preparing for labor and delivery, maintaining a healthy diet, staying well-rested, and staying active. Here are 5 tips for healthy pregnancy at week 40.
- Attend Regular Antenatal Appointments: Routine antenatal appointments are recommended weekly from week 37 until delivery. Prenatal visits typically include monitoring your blood pressure, weight, fetal growth, and heartbeat. Additional monitoring is often necessary for high-risk pregnancies. Start discussing options for delivery, including the possibility of a C-section if needed. Keep in touch with your healthcare provider to address potential medical conditions and promote overall fetal and maternal well-being before delivery.
- Prepare for Labor and Delivery: Discuss various methods for inducing labor with your OB/GYN or midwife, including hormones like oxytocin to induce contractions, balloon catheters to help with cervical dilation, or procedures like amniotomy (artificially rupturing the amniotic sac) and membrane stripping, (separation of the amniotic sac from the uterine wall). Know how to monitor contractions and immediately contact your healthcare provider when labor starts.
- Maintain a Healthy Diet and Lifestyle: A balanced diet is crucial for maternal and fetal health as you approach delivery. Focus on consuming various nutrient-rich foods, including fruits and vegetables, and stay hydrated by drinking plenty of fluids throughout the day. Steer clear of high-risk foods such as soft cheeses, deli meats, raw or undercooked meats and seafood, pre-prepared salads, uncooked bean sprouts, and raw eggs to avoid food-borne illnesses like listeriosis.
- Stay Well-Rested and Relaxed: Prioritizing rest and relaxation in the final week of pregnancy boosts physical and emotional health. Relaxation techniques, such as deep breathing exercises and meditation, help manage stress and anxiety. Communicate your feelings with loved ones or therapists to help you prepare emotionally for childbirth and parenting.
- Stay Active: Staying active during pregnancy positively impacts the mother’s physical and psychological well-being. Gentle exercises like walking and stretching help improve circulation and alleviate discomfort, such as back pain. Pelvic exercises strengthen pelvic floor muscles and prevent urinary incontinence (urine leakage when laughing, sneezing, or coughing). Avoid overexertion and adjust your exercise routine to prioritize safety and comfort.
What Types Of Foods Are Beneficial To Eat During Week 40 Of Pregnancy?
Types of foods beneficial to eat during 40 weeks of pregnancy include foods rich in calcium, iron, iodine, choline, vitamins A, C, D, B6, B12, and folate to support your health and your baby’s development. Here are 15 beneficial foods to eat during week 40 of pregnancy.
- Calcium: Calcium helps build strong bones and teeth. Try consuming cheese, yogurt, milk, and dark green leafy vegetables.
- Iron: Iron supports red blood cell production and oxygen transport, helping prevent anemia and fatigue. Good sources include lean red meat, iron-fortified cereals, beans, lentils, spinach, and prune juice.
- Iodine: Iodine is crucial for healthy brain development. Consume iodized table salt, eggs, and dairy products.
- Choline: Choline is important for fetal brain and spinal cord development. Incorporate beef liver, peanuts, and eggs.
- Vitamin A: Vitamin A supports vision and immune function. Get Vitamin A from sweet potatoes, green leafy vegetables, and carrots.
- Vitamin C: Vitamin C strengthens the immune system and supports tissue repair. Try strawberries, tomatoes, citrus fruits, and bell peppers.
- Vitamin D: Vitamin D is vital for bone health and immune function. Consume fortified milk, salmon, sardines, and fortified soy beverages.
- Vitamin B6: Vitamin B6 helps with brain development and red blood cell production. Obtain Vitamin B6 from whole-grain cereals, pork, bananas, and chicken.
- Vitamin B12: Vitamin B12 supports nerve function and red blood cell formation. Have fish, milk, poultry, and eggs.
- Folic acid: Folic acid prevents birth defects and supports overall growth. Consume enriched bread, dark green leafy vegetables, beans, and lentils.
- Grains: Grains supply energy and fiber. Try brown rice, quinoa, oats, whole-wheat bread, and millet.
- Fruits: Fruits provide vitamins and minerals for your baby’s growth. Choose from fresh fruit, dried fruit, or frozen fruit.
- Vegetables: Vegetables provide essential vitamins and minerals. Try raw vegetables, canned vegetables, and 100% vegetable juice.
- Protein: Protein supports tissue growth and development. Get protein from seafood, poultry, lean meat, soy products, nuts, seeds, and lentils.
- Dairy: Dairy provides calcium and protein. Consume milk, cheese, yogurt, lactose-free dairy, and fat-free dairy.
What Exercises Can You Do During Week 40 Of Pregnancy?
Exercises you can do during week 40 of pregnancy include walking, swimming, stretching, pelvic floor exercises, and stationary cycling, according to the 2020 World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour. Here are the 5 exercises you can do during week 40 of pregnancy.
- Walking: A gentle walk remains an excellent way to stay active, improve circulation, and promote relaxation as you approach labor. Walking encourages the baby’s descent by leveraging gravity and the back-and-forth motion of your hips.
- Swimming: Swimming or water-based exercises help reduce swelling and provide a low-impact way to stay fit, easing the pressure on your joints.
- Stretching: Stretching helps alleviate tension in common areas of discomfort at 40 weeks, including the back and legs. Incorporating breathing techniques like inhaling and exhaling when stretching enhances relaxation.
- Pelvic floor exercises: Daily pelvic floor muscle training (Kegels) strengthens pelvic muscles, helps with labor, and reduces risks of postpartum incontinence.
- Stationary cycling: Using a stationary bike keeps your cardiovascular fitness up without straining the body. Low-impact exercises like stationary cycling help maintain fitness as your due date approaches.
Aim for at least 150 minutes of moderate-intensity exercises, even at week 40. Make sure to avoid exercises with risks of falling or high-impact movements. Always stay hydrated, especially if exercising in warmer conditions.
What Are The Things To Avoid At 40 Weeks Pregnant?
Things to avoid at 40 weeks pregnant include alcohol, smoking, recreational drugs, caffeine, certain medications and supplements, and high-mercury fish. Here are 14 things you must avoid at 40 weeks pregnant.
- Alcohol: Avoid alcohol completely. Alcohol consumption leads to developmental problems, birth defects, and cognitive issues in your baby, as emphasized by a 2020 study, “Alcohol Use in Pregnancy,” published in Clinical Obstetrics and Gynecology.
- Smoking and Secondhand Smoke: Smoking causes complications like low birth weight, fetal macrosomia, and preterm labor. Smoking in pregnancy poses several risks, as outlined by a 2020 study published in the International Journal of Environmental Research and Public Health. Quit smoking to protect your baby’s well-being.
- Recreational Drugs: Substances like cannabis and other drugs harm your baby’s development, leading to complications like low birth weight and developmental delays.
- Caffeine: Limit caffeine intake to under 200mg per day. Excessive caffeine consumption increases the risk of complications like low birth weight.
- Certain Medications and Supplements: Always consult your healthcare provider before taking any medications or supplements. Certain medications pose risks to your baby, especially as the cervix thins and dilates in preparation for labor.
- High Mercury Fish: Avoid high-mercury fish such as sharks and swordfish to prevent mercury exposure, which affects your baby’s brain development.
- Undercooked or Raw Meat: Stick to well-cooked meats to avoid infections like toxoplasmosis, harmful to your baby.
- Unpasteurized Foods: Avoid unpasteurized dairy and soft cheeses to prevent listeria infection, which causes pregnancy complications.
- Deli Meats: Ensure your deli meats are heated thoroughly to prevent exposure to harmful bacteria.
- Hot Tubs and Saunas: Avoid exposure to high temperatures, as overheating harms you and your baby.
- Strenuous Physical Activity: Avoid intense physical activities or contact sports to prevent injury or preterm labor. Contact your healthcare provider if you experience discomfort or dizziness during exercise.
- Exposure to Harmful Chemicals: Minimize exposure to toxic chemicals such as household cleaners and pesticides.
- Stress: Try to manage stress levels, as high stress affects labor and delivery. Engage in calming activities like stretching to relax the mind and body.
- Hair Dye: Hair dye exposure has been linked to infant health issues. Consider waiting until after delivery before dyeing your hair, or opt for natural products if necessary.
What Are The Possible Complications That Can Happen At 40 Weeks Pregnant?
Possible complications that can happen at 40 weeks pregnant include gestational diabetes, stillbirth, hypertension and preeclampsia, placenta previa, and placental abruption. Here are 5 possible complications that occur during week 40.
- Gestational Diabetes: Gestational diabetes mellitus (GDM) is a type of diabetes developing during pregnancy, leading to elevated blood sugar and glucose levels. GDM increases maternal risks for conditions such as gestational hypertension, pre-eclampsia, cesarean section births, and delivery complications, including fetal macrosomia (a condition of larger than average fetal growth). GDM raises the risk of breathing problems in the newborn, as well as type 2 diabetes and cardiovascular problems for the mother and baby.
- Stillbirth: Stillbirth involves pregnancy losses after 20 weeks. Key factors leading to stillbirth include fetal abnormalities (such as chromosomal issues), maternal health problems (like cervical incompetence, hormonal imbalances, or chronic conditions), placental complications, and infections.
- Hypertension (High Blood Pressure) and Preeclampsia: Preeclampsia (PE) is a pregnancy-related disorder occurring after week 20. Symptoms of PE include hypertension (high blood pressure), protein in the urine, sudden weight gain, persistent headaches, and vision changes. Preeclampsia occurs in 3%-5% of pregnancies globally and often leads to serious complications such as eclampsia (seizures), kidney failure, and even death if left untreated. Contact your OBGYN immediately if you experience any PE symptoms.
- Placenta Previa: Placenta previa is a pregnancy complication characterized by a low-positioned placenta covering part or all of the cervical opening. Placenta previa often raises the likelihood of cesarean delivery due to the risks of severe bleeding and shock, leading to postpartum hemorrhage and maternal mortality. Symptoms of placenta previa include painless or heavy vaginal bleeding during the second or third trimester, sometimes triggered by intercourse or medical examinations. Consult your OBGYN for proper testing and management upon experiencing vaginal bleeding.
- Placental Abruption: Placental abruption involves placental detachment from the uterus before delivery, leading to significant vaginal bleeding and severe maternal and fetal risks. Symptoms include abdominal pain, heavy bleeding, and uterine tenderness. Placental abruption often leads to complications such as low birth weight, developmental delays, and neonatal mortality. Monitoring for signs of placental abruption is crucial, especially for women with risk factors such as high blood pressure or preeclampsia. Immediate medical attention is essential if symptoms arise.
How Can A Partner Support The Mother At 40 Weeks Pregnant?
A partner can support the mother at 40 weeks pregnant through physical task assistance, involvement in maternal health, partner communication, physical affection, and encouraging healthy habits. Here are 5 ways a partner can support the mother at 40 weeks.
- Physical Task Assistance: Provide physical support by doing household chores like cleaning, grocery shopping, and preparing meals to ease daily burdens. Take on physical work, especially heavy lifting, to keep your partner well-rested while preparing for labor and delivery. Encourage the mother to avoid strenuous housework and rest as much as possible. Engage in stress-relief activities, such as gentle exercises, to reduce anxiety and contribute to a more comfortable pregnancy experience.
- Involvement in Maternal Health: Offering practical and emotional support and preparing for the baby’s arrival enhances the connection between partners. Attend prenatal appointments and keep a list of questions to stay informed about the pregnancy. Help pack the hospital bag, know the birth plan, and consider hiring a doula for additional support. Learn how to assist with labor and delivery, such as guiding your partner’s breathing, holding her hand, and wiping her face to provide comfort and encouragement.
- Partner Communication: Start open and honest discussions to understand each other’s feelings, ask questions, and share your experiences. Discuss any fears or concerns with your partner, providing reassurance and support throughout the pregnancy journey. Be a reliable support system by building trust and encouraging your partner to seek additional guidance from others when necessary. Being open and honest ensures you are ready for your baby’s arrival as a team.
- Physical Affection: Offer your partner hugs, hold hands, or give a kiss to show affection through small gestures of intimacy. Even gentle bumps or touches help them feel loved and supported. Acts of affection help strengthen the bond between partners, reduce stress and anxiety, enhance security, and promote well-being, according to a 2006 study, “Effective social support: Antecedents and consequences of partner support during pregnancy.” Supporting each other through physical affection is especially important for partners during pregnancy.
- Encourage Healthy Habits: Promote healthy habits by engaging in a balanced diet and regular physical activity together. Foster a supportive environment by making healthy choices, such as increasing fruit and vegetable consumption and collaborating on meal planning and physical activities. Advocate for your partner by helping to avoid unsafe foods and being mindful of ingredients during meal prep. Proactively promoting healthy habits strengthens your partnership and ensures a healthier pregnancy.
What Prenatal Tests Are Needed At 40 Weeks Pregnant?
Prenatal tests necessary at 40 weeks include a prenatal checkup, blood tests, and biophysical profiling.
A prenatal appointment at 40 weeks often includes physical and gynecological exams, such as a breast exam to address potential breastfeeding concerns and pelvic or vaginal exams to evaluate labor progress. Screening ultrasounds during prenatal care helps monitor fetal heartbeat and growth. Papanicolaou smears (pap smears) are offered based on recommended intervals and smear history to ensure cervical health but are not usually repeated during pregnancy.
Blood tests include monitoring rubella IgG levels to assess rubella immunity. A complete blood count (CBC) helps detect infections, including HIV and syphilis. The Rhesus (Rh) factor blood test checks for Rh incompatibility, in which the mother’s antibodies attack the baby’s red blood cells. Urine tests, such as urinalysis, check for protein and sugar in the urine to screen for complications like preeclampsia, anemia, and gestational diabetes.
Biophysical profiling (BPP) uses fetal ultrasound and non-stress tests to monitor fetal movement, breathing, muscle tone, heart rate, and amniotic fluid levels. BPP helps ensure the baby receives adequate oxygen and nutrient supply in the womb.
When To Call Your Doctor If Something Feels Wrong At Week 40 Of Pregnancy?
Call your doctor if something feels wrong at 40 weeks pregnant or if you experience symptoms like extreme swelling, decreased fetal movement, severe headaches, excessive bleeding, and severe abdominal pain. Here are 5 symptoms you must report to your doctor at 40 weeks of pregnancy.
- Decreased Fetal Movement: Decreased fetal movement is linked to fetal growth restriction and stillbirth, according to a 2008 study, “Fetal Movement Assessment,” by J. Frederik Frøen et al., published in Seminars in Perinatology. Monitor fetal kicks closely and contact your OBGYN immediately if you feel fewer than ten movements in an hour. Regularly tracking movements helps ensure your baby’s well-being in the final stages of pregnancy.
- Extreme/Sudden Swelling: Extreme swelling or puffiness in the face, hands, or lower extremities often indicates preeclampsia, a complication characterized by high blood pressure and protein in the urine. Monitor for additional symptoms such as persistent headaches, confusion, and vision problems. Report any severe, sudden swelling to your healthcare provider for prompt treatment.
- Severe Headaches: Severe, persistent headaches often indicate preeclampsia (high blood pressure after 20 weeks gestation), especially if accompanied by symptoms like blurred vision, flashing lights, dizziness, or fainting spells. Preeclampsia causes a spike in the mother’s blood pressure, leading to severe complications if left untreated.
- Excessive Vaginal Bleeding: Heavy and prolonged vaginal bleeding signals serious complications like placental abruption. Contact your OBGYN if you experience symptoms like severe pain in the lower abdomen, weakness, or severe abdominal pain. Multiple episodes of heavy bleeding risk leading to low birth weight and delivery complications.
- Severe Abdominal Pain: Severe abdominal pain indicates serious conditions like placental abruption, acute appendicitis, or uterine complications. Contact your OBGYN if you experience intense, frequent cramping in the lower abdomen, sharp belly pain, or contractions. Heavy bleeding alongside sharp pain often signals a more severe issue and warrants immediate medical attention.
What are the 40 weeks pregnant symptoms not to ignore? 40 weeks pregnant symptoms not to ignore include decreased fetal movement, extreme swelling, headaches, vaginal bleeding, and severe abdominal crampings. Always trust your instincts during pregnancy. If something feels off, reach out to your OB/GYN or healthcare provider, even if you aren’t experiencing any specific symptoms that seem alarming. You are the best judge of how you feel.
Are There Prenatal Vitamins Needed To Be Taken During Week 40 Of Pregnancy?
Yes, key prenatal vitamins must be taken during week 40 of pregnancy to support the mother and baby, as recommended by the American College of Obstetricians and Gynecologists (ACOG).
Calcium, at 1,000 milligrams, supports the mother’s bones, which are under stress during pregnancy. Calcium ensures the development of strong fetal bones and teeth.
Iron, with a recommended 27 milligrams of iron daily, plays a key role in oxygen transport to the baby. Iron is crucial as the body requires more blood to support the mother and baby. Adequate iron levels help prevent anemia, a common issue in the later stages of pregnancy.
Iodine, at 220 micrograms, remains essential for the baby’s brain and nervous system development. Thyroid functions regulated by iodine support the baby’s growth and neurological functions.
Choline, at 450 milligrams, contributes to the ongoing development of the baby’s brain and spinal cord. Choline supports neural functions significantly until after birth.
Vitamin A, at 770 micrograms, maintains healthy skin and eyesight for the mother and baby. Vitamin A supports the development of the baby’s organs, including the heart, lungs, and kidneys.
Vitamin C, at 85 milligrams, enhances the mother’s immune system, helps with iron absorption, and supports healthy gums, teeth, and bones.
Vitamin D, at 600 international units, supports the baby’s bones and teeth development. Vitamin D aids in calcium absorption and fetal skeletal system development
Vitamin B6, at 1.9 milligrams, remains essential in helping the body process protein, fat, and carbohydrates, while contributing to red blood cell production. Vitamin B6 helps manage pregnancy-related symptoms, such as nausea.
Vitamin B12, at 2.6 micrograms, supports the mother’s nervous system and aids red blood cell production. Vitamin B12 ensures the healthy development of the baby’s nervous system.
Folic acid, at 600 micrograms per day, remains critical throughout pregnancy, to prevent neural tube defects (NTDs) and support overall fetal development. Folic acid aids the baby’s central nervous system and organ development.
Talk to your healthcare provider to choose the best prenatal supplement, especially as you approach delivery.
What Does Parenting Styles Suggest About 40 Weeks Pregnant?
Parenting Styles suggests double-checking your hospital bag for all the essentials and reviewing breastfeeding techniques. Ensure you haven’t forgotten anything on your hospital bag checklist, including comfy clothes for you and the cutest outfits for your little one. Refresh your knowledge of breastfeeding techniques if you decide to breastfeed. Read up-to-date resources or watch instructional videos to familiarize yourself with current best practices.
“Having a well-stocked hospital bag is one less thing to worry about,” says Pamela Li, the Founder and Editor-in-Chief of Parenting Styles.
Congratulations on being 40 weeks pregnant! You are at the finishing line.